Healthcare is shifting dramatically. Hospitals are merging with health systems, private practices are joining larger networks, and independent physicians are finding themselves part of massive organizational structures they never imagined joining just a decade ago. This wave of consolidation brings many changes, but one area that often gets overlooked is how these mergers and acquisitions impact provider credentialing timelines.
If you’re a healthcare administrator, physician, or anyone involved in the credentialing process, you’ve likely experienced firsthand how consolidation can turn what should be routine credentialing into a months-long ordeal. The reasons behind these delays are multifaceted and often frustrating, but they’re becoming increasingly important to recognize and address as healthcare consolidation shows no signs of slowing down.
The Current State of Healthcare Consolidation
 Healthcare consolidation has accelerated rapidly over the past two decades. Large health systems are acquiring smaller hospitals, physician practices are being absorbed into hospital networks, and insurance companies are purchasing provider groups at an unprecedented rate. This trend is driven by several factors: the desire to achieve economies of scale, improve care coordination, negotiate better rates with payers, and respond to value-based care initiatives.
Healthcare consolidation has accelerated rapidly over the past two decades. Large health systems are acquiring smaller hospitals, physician practices are being absorbed into hospital networks, and insurance companies are purchasing provider groups at an unprecedented rate. This trend is driven by several factors: the desire to achieve economies of scale, improve care coordination, negotiate better rates with payers, and respond to value-based care initiatives.
However, what looks good on paper doesn’t always translate smoothly in practice. When two healthcare organizations merge, they don’t just combine their patient populations and revenue streams. They also merge their administrative processes, technology systems, policies, and procedures. Credentialing, which relies heavily on standardized processes and documentation, becomes particularly challenging during these transitions.
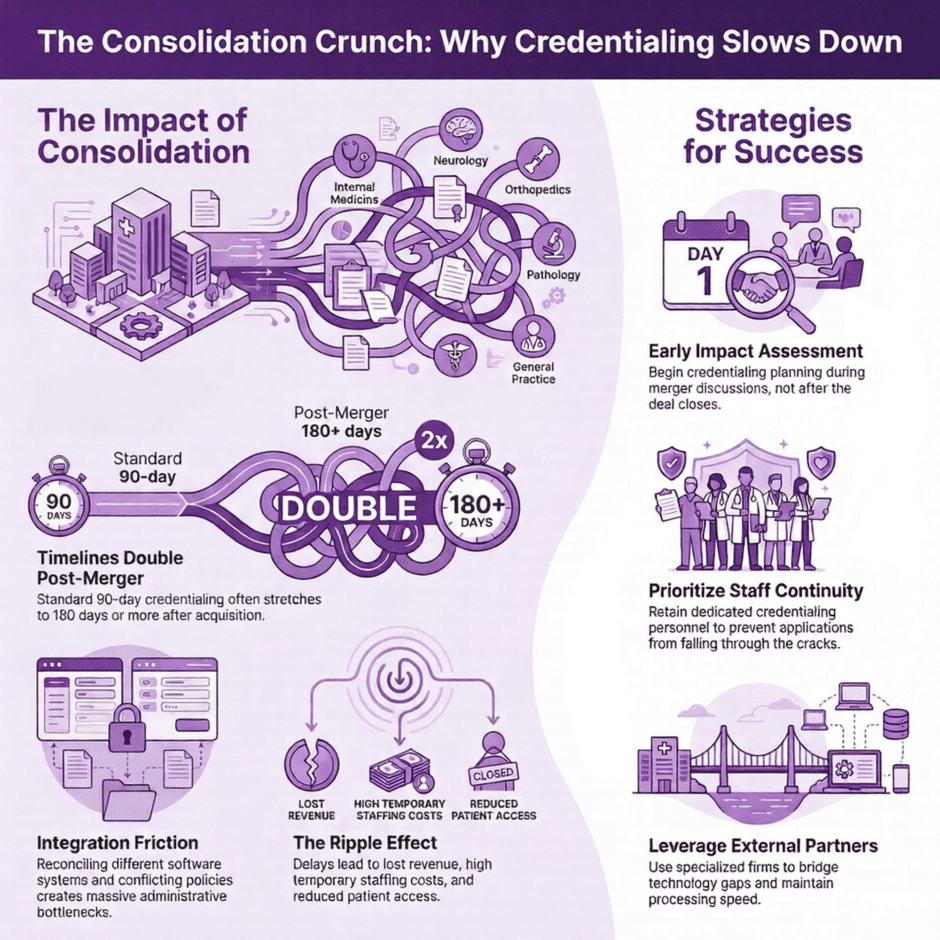
The impact on credentialing timelines is often immediate and significant. What might have taken 90 days in a smaller, independent practice can suddenly stretch to 180 days or more when that practice becomes part of a larger health system. This delay affects not just the providers waiting for approval, but also patients who may face longer wait times for appointments and reduced access to care.
Why Consolidation Complicates Credentialing
When healthcare organizations merge, they face the monumental task of reconciling different credentialing systems, policies, and procedures. Each organization brings its own way of doing things, and finding common ground isn’t always straightforward.
Consider what happens when a 50-physician practice joins a 500-physician health system. The practice might have used a streamlined, informal credentialing process where the medical director personally knew many of the providers and could expedite applications based on relationships and local knowledge. The health system, meanwhile, likely has a formal credentialing committee, standardized application processes, and multiple layers of review designed to manage risk across a much larger organization.
The newly acquired practice must now adapt to the health system’s credentialing requirements, which often means starting from scratch with applications that were previously approved. Providers who were already credentialed with the practice may need to go through an entirely new credentialing process to meet the health system’s standards. This creates a bottleneck as the health system’s credentialing department suddenly faces a influx of new applications while still managing their existing workload.
Technology integration presents another significant hurdle. Many healthcare organizations use different credentialing software systems, and these systems don’t always communicate with each other effectively. During a merger, organizations must decide whether to migrate all data to one system, maintain parallel systems temporarily, or invest in new technology altogether. Each option comes with its own timeline and potential for delays.
The Ripple Effects of Extended Credentialing Timelines
 When credentialing timelines stretch beyond normal parameters, the effects ripple throughout the healthcare system. Providers who are waiting for credentialing approval may be unable to see patients, prescribe medications, or perform procedures, even if they were fully credentialed at their previous organization just weeks earlier. This creates immediate revenue impacts for both the provider and the organization.
When credentialing timelines stretch beyond normal parameters, the effects ripple throughout the healthcare system. Providers who are waiting for credentialing approval may be unable to see patients, prescribe medications, or perform procedures, even if they were fully credentialed at their previous organization just weeks earlier. This creates immediate revenue impacts for both the provider and the organization.
Patients bear much of the burden of these delays. When providers can’t be credentialed quickly, patient access to care suffers. Appointment wait times increase, and patients may be forced to seek care elsewhere or delay treatment entirely. In specialized areas of medicine, where there may already be provider shortages, credentialing delays can create serious access issues for entire communities.
The financial implications extend beyond lost revenue. Organizations must often pay temporary staffing costs or locum tenens fees to maintain service levels while waiting for permanent providers to be credentialed. These costs can quickly escalate, particularly in high-demand specialties where temporary staffing commands premium rates.
Staff morale and retention also suffer when credentialing timelines extend indefinitely. Providers who are eager to start their new positions may become frustrated with lengthy delays, and some may even choose to accept positions elsewhere rather than wait for the credentialing process to finish. This creates additional costs related to recruitment and hiring replacement providers.
Specific Challenges in Post-Merger Credentialing
Healthcare consolidation creates several specific challenges that don’t exist in stable organizational environments. One of the most significant is the need to reconcile different credentialing standards. Organizations may have different requirements for background checks, reference verifications, or continuing education credits. When they merge, they must decide which standards to adopt, and this decision-making process alone can add weeks or months to credentialing timelines.
Payer contract negotiations also become more intricate after consolidation. The newly formed organization must renegotiate contracts with insurance companies, and these negotiations can affect provider credentialing with those payers. Providers may find themselves unable to bill certain insurance plans while contract negotiations are ongoing, creating additional delays and administrative burden.
Documentation requirements often change post-merger as well. Providers may need to submit additional paperwork, update their applications to meet new organizational standards, or provide documentation that wasn’t required by their previous organization. This back-and-forth process of requesting and submitting additional documentation can significantly extend credentialing timelines.
Communication breakdowns are another common challenge. During consolidation, staff members may be reassigned, laid off, or given new responsibilities. The people who were previously responsible for credentialing may no longer be available, and new staff members may not be familiar with pending applications or organizational requirements. This can lead to applications sitting in queues for weeks while staff members figure out their new roles and responsibilities.
Strategies for Managing Credentialing During Consolidation
 While healthcare consolidation will likely continue, there are strategies that organizations can employ to minimize the impact on credentialing timelines. The key is planning ahead and maintaining focus on the credentialing process even amid all the other changes that come with merger or acquisition.
While healthcare consolidation will likely continue, there are strategies that organizations can employ to minimize the impact on credentialing timelines. The key is planning ahead and maintaining focus on the credentialing process even amid all the other changes that come with merger or acquisition.
Early planning makes a significant difference. Organizations should begin assessing credentialing implications as soon as merger discussions begin, not after the deal closes. This includes inventorying all current provider credentials, identifying differences in credentialing requirements between organizations, and developing a timeline for reconciling these differences.
Maintaining dedicated credentialing staff during transitions helps ensure continuity. While many departments may experience staffing changes during consolidation, keeping experienced credentialing personnel in place can prevent applications from falling through the cracks. If staff changes are unavoidable, organizations should ensure proper knowledge transfer and documentation of all pending applications.
Technology planning should also begin early in the consolidation process. Organizations need to determine how they’ll handle credentialing software integration, data migration, and system compatibility. Waiting until after the merger to address these issues almost guarantees significant delays in credentialing processing.
Clear communication with providers throughout the process helps manage expectations and reduces frustration. Providers should be informed about potential credentialing delays well in advance and given regular updates on their application status. This transparency helps maintain relationships and reduces the likelihood that providers will seek opportunities elsewhere while waiting for credentialing completion.
The Role of External Partners in Streamlining Credentialing
Many healthcare organizations are discovering that working with external credentialing partners can help mitigate the challenges that come with consolidation. These partners bring specialized expertise, established processes, and dedicated resources that can help maintain credentialing timelines even during periods of organizational change.
External partners can provide continuity when internal staff members are dealing with multiple competing priorities during consolidation. They often have established relationships with payers, primary source verification organizations, and other entities involved in the credentialing process, which can help expedite applications even when internal processes are in flux.
Technology resources available through external partners can also bridge gaps during system integration periods. Rather than waiting months for internal systems to be fully integrated, organizations can leverage external platforms to keep credentialing processes moving forward. This approach can significantly reduce the time between merger completion and full credentialing capability.
The expertise that external partners bring to credentialing can be particularly valuable during consolidation. They’ve often worked with multiple healthcare organizations and have experience managing credentialing challenges across different organizational structures and requirements. This experience can help newly consolidated organizations avoid common pitfalls and implement best practices more quickly.
Industry-Specific Considerations
 Different types of healthcare consolidation create different credentialing challenges. When hospitals merge with other hospitals, the focus is often on reconciling medical staff bylaws, credentialing committee structures, and privileging processes. These organizations typically have established credentialing departments, so the challenge is more about integration than building new processes.
Different types of healthcare consolidation create different credentialing challenges. When hospitals merge with other hospitals, the focus is often on reconciling medical staff bylaws, credentialing committee structures, and privileging processes. These organizations typically have established credentialing departments, so the challenge is more about integration than building new processes.
When hospitals acquire physician practices, the challenges are often greater because the practice may not have had formal credentialing processes in place. The hospital must bring the practice’s providers up to hospital credentialing standards, which can involve extensive documentation gathering and verification processes that the practice never previously required.
Private equity acquisitions of healthcare organizations create their own unique credentialing challenges. These new owners often implement standardized processes across multiple acquired organizations, which means providers may need to adapt to new requirements even if they’re not directly merging with another healthcare organization.
Insurance company acquisitions of provider organizations add another layer of considerations, as these arrangements often involve both provider credentialing and network participation requirements. Providers may find themselves navigating both traditional credentialing processes and payer enrollment procedures simultaneously.
Tomorrow’s Credentialing Trends
As healthcare consolidation continues, the industry is likely to see continued pressure on credentialing timelines unless organizations proactively address these challenges. The trend toward larger healthcare organizations shows no signs of slowing, which means credentialing departments will need to become more efficient and scalable to handle the volume of applications that come with growth.
Technology solutions will likely play an increasingly important role in managing credentialing during consolidation. Automated verification processes, artificial intelligence applications for document review, and blockchain-based credential verification are all emerging technologies that could help reduce credentialing timelines regardless of organizational changes.
Industry standardization efforts may also help reduce consolidation-related credentialing delays. As organizations recognize the costs associated with extended credentialing timelines, there may be increased pressure to develop standard credentialing requirements and processes that can be more easily transferred between organizations.
The regulatory environment will also continue to shape credentialing practices. As value-based care initiatives expand and quality reporting requirements become more stringent, credentialing processes may become more intensive, but they may also become more standardized across organizations.
Summary: How Healthcare Consolidation Affects Credentialing Timelines
 Healthcare consolidation is reshaping the industry in fundamental ways, and its impact on credentialing timelines represents just one of many operational challenges that organizations must address. The delays and complications that often accompany post-merger credentialing can have far-reaching effects on provider satisfaction, patient access, and organizational finances.
Healthcare consolidation is reshaping the industry in fundamental ways, and its impact on credentialing timelines represents just one of many operational challenges that organizations must address. The delays and complications that often accompany post-merger credentialing can have far-reaching effects on provider satisfaction, patient access, and organizational finances.
However, these challenges are not insurmountable. With proper planning, dedicated resources, and strategic approaches to managing credentialing during transitions, healthcare organizations can minimize the impact of consolidation on credentialing timelines. The key is recognizing that credentialing should be considered a critical component of merger planning, not an afterthought to be addressed once the deal is complete.
For healthcare organizations facing consolidation, partnering with experienced credentialing specialists like Medwave, which provides billing, credentialing, and payer contracting services, can provide the expertise and resources needed to maintain efficient credentialing processes during times of organizational change. As the healthcare landscape continues to shift, the organizations that prioritize maintaining efficient credentialing processes will be better positioned to attract and retain quality providers while ensuring continued patient access to care.

