If you’re a healthcare provider looking to expand your practice and serve more patients, getting credentialed with Medicaid is a smart move. Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. By becoming a credentialed Medicaid provider, you open your doors to a significant patient population that needs your services.
 The credentialing process can feel overwhelming at first. There are forms to fill out, documents to gather, and specific requirements to meet. The good news? Once you know what to expect and how to prepare, the process becomes much more manageable. This guide will walk you through everything you need to know about getting credentialed with Medicaid, from start to finish.
The credentialing process can feel overwhelming at first. There are forms to fill out, documents to gather, and specific requirements to meet. The good news? Once you know what to expect and how to prepare, the process becomes much more manageable. This guide will walk you through everything you need to know about getting credentialed with Medicaid, from start to finish.
What Does It Mean to Be Credentialed?
Credentialing is the process that verifies your qualifications as a healthcare provider. Think of it as Medicaid’s way of making sure you have the proper education, training, licenses, and experience to provide quality care to their members. When you’re credentialed, you’re officially approved to see Medicaid patients and receive payment for your services.
Every state runs its own Medicaid program, which means the credentialing requirements can vary depending on where you practice. Some states handle credentialing directly through their Medicaid agency, while others work with managed care organizations (MCOs) that have their own credentialing procedures. This is important to keep in mind as you begin the process.
Why Should You Get Credentialed with Medicaid?
You might be wondering if the effort is worth it.
Here’s why many providers choose to accept Medicaid patients:
- You’ll significantly increase your potential patient base. In some communities, Medicaid beneficiaries make up a large percentage of residents who need healthcare services. By accepting Medicaid, you’re making your practice accessible to people who might otherwise struggle to find care.
- It’s a way to give back to your community. Many Medicaid patients face barriers to healthcare access, and by opening your practice to them, you’re providing a valuable service. You’re helping ensure that everyone, regardless of their financial situation, can receive the medical care they need.
- While Medicaid reimbursement rates are typically lower than private insurance, the steady stream of patients can help stabilize your practice’s revenue. Plus, some states offer enhanced payment rates for certain services or provider types, which can make accepting Medicaid more financially viable.
What You’ll Need to Get Started
 Before you dive into the application process, it’s helpful to gather all the necessary documentation ahead of time. This preparation will make the process smoother and faster. You’ll typically need your medical degree and any other relevant diplomas, proof of completed residency and fellowship training, current state medical license, DEA registration (if applicable), and board certification documents.
Before you dive into the application process, it’s helpful to gather all the necessary documentation ahead of time. This preparation will make the process smoother and faster. You’ll typically need your medical degree and any other relevant diplomas, proof of completed residency and fellowship training, current state medical license, DEA registration (if applicable), and board certification documents.
You’ll also need to provide your National Provider Identifier (NPI) number, which is a unique identification number for healthcare providers. If you don’t have one yet, you can apply for it through the National Plan and Provider Enumeration System (NPPES). The application is free and can be done online.
Additionally, be prepared to share information about your malpractice insurance coverage, including your policy numbers and coverage amounts. Most states require specific minimum coverage amounts, so check your state’s requirements. You’ll also need to provide details about your work history, including where you’ve practiced over the past several years.
The Application Process
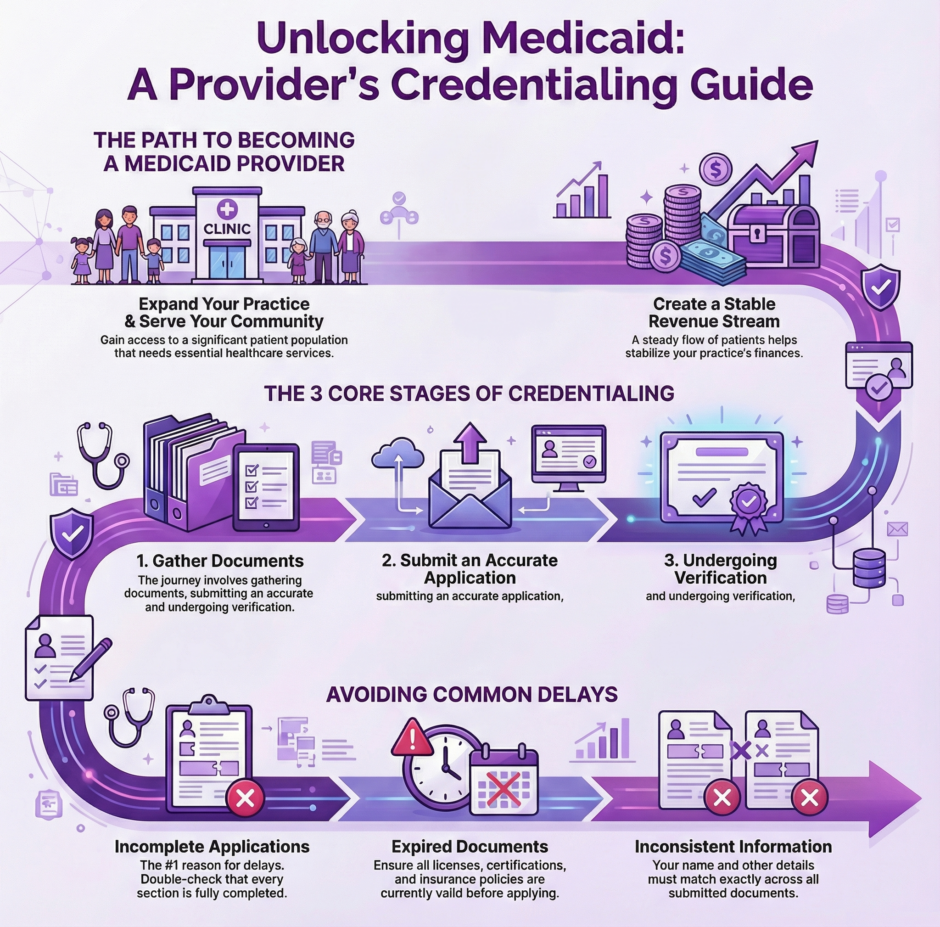
The credentialing application itself is where many providers feel stuck, but breaking it down into steps makes it more approachable. Start by determining which application you need to complete. If your state uses managed care organizations, you might need to apply separately to each MCO. Some states participate in the Council for Affordable Quality Healthcare (CAQH), which allows you to complete one application that multiple payers can access.
When filling out your application, accuracy is crucial. Double-check every piece of information you enter. A small error or inconsistency can delay your application for weeks or even months. Make sure your name appears exactly the same way on all documents, and verify that all dates are correct.
One of the most time-consuming parts is explaining any gaps in your work history or training. If you took time off for personal reasons, additional education, or research, be prepared to provide documentation and explanations. Medicaid credentialing committees want to see a continuous record of your professional activities.
You’ll also need to disclose any history of malpractice claims, license actions, or sanctions. This doesn’t automatically disqualify you, but failing to disclose this information can result in denial or termination of your credentials. Honesty is always the best policy in the credentialing process.
Background Checks and Verification

Once you submit your application, Medicaid will verify everything you’ve provided. They’ll check your medical education, licenses, board certifications, work history, and references. They’ll also conduct background checks, which may include criminal history checks and queries to the National Practitioner Data Bank.
This verification process takes time because Medicaid contacts each institution and organization directly. Medical schools need to confirm your graduation, licensing boards need to verify your licenses, and previous employers need to confirm your work history. This is why the credentialing process often takes 90 to 180 days, though it can sometimes take longer.
During this waiting period, respond quickly to any requests for additional information. If Medicaid can’t verify something or needs clarification, they’ll reach out to you. The faster you respond, the faster your application can move forward.
Site Visits and Inspections
Depending on your state and the type of practice you have, Medicaid may require a site visit before approving your credentials. During a site visit, a representative will come to your practice location to ensure it meets certain standards. They’ll check that your office is accessible to patients with disabilities, that you have appropriate equipment and supplies, and that your facility meets health and safety regulations.
If you know a site visit is coming, take time to prepare. Make sure all required signage is posted, emergency exits are clearly marked, and your waiting area is clean and welcoming. Have your medical records system organized and ready to demonstrate if asked. These visits aren’t meant to be intimidating. They’re simply a way for Medicaid to ensure that patients will receive care in an appropriate setting.
What Happens After Approval?
 Congratulations! Once you’re approved, you’ll receive notification along with your Medicaid provider number. This number is what you’ll use when billing for services. Make sure you understand your state’s billing requirements and procedures. Each state has specific rules about how to submit claims, what documentation is required, and what time limits apply.
Congratulations! Once you’re approved, you’ll receive notification along with your Medicaid provider number. This number is what you’ll use when billing for services. Make sure you understand your state’s billing requirements and procedures. Each state has specific rules about how to submit claims, what documentation is required, and what time limits apply.
You’ll also want to make sure your staff knows how to verify Medicaid eligibility. Before each appointment, check that the patient’s Medicaid coverage is active. This simple step can prevent billing issues down the road.
Keep in mind that credentialing isn’t a one-time event. You’ll need to go through recredentialing every few years. Medicaid will send you renewal notices, but it’s your responsibility to track these deadlines and submit updated information on time. Missing a recredentialing deadline can result in a lapse in your provider status, which means you won’t be able to see Medicaid patients or receive payment until you’re reinstated.
Common Challenges and How to Avoid Them
Many providers run into similar obstacles during the credentialing process.
Here are the most common issues and how to prevent them:
- Incomplete applications: This is the number one reason for delays. Before submitting your application, review it carefully to ensure every section is complete and every required document is attached.
- Expired documents: Make sure all your licenses, certifications, and insurance policies are current. If something is set to expire soon, renew it before applying.
- Inconsistent information: Your information must match across all documents. If you’ve changed your name, make sure all documents reflect the current name or include legal documentation of the name change.
- Missing signatures: Many applications require signatures in multiple places. A missing signature can hold up your entire application.
- Unresponsive references: Choose references who you know will respond promptly to verification requests. Give them a heads up that they might be contacted.
Working with Managed Care Organizations

If your state uses managed care organizations, you’ll need to decide which MCOs to join. Research the different plans available in your area. Look at their provider networks, patient populations, and reimbursement rates. Some providers choose to join all available MCOs to maximize their patient base, while others are more selective.
Each MCO will have its own credentialing application, though many accept CAQH applications. Be prepared for the fact that credentialing with multiple MCOs means multiple applications, multiple verification processes, and potentially multiple site visits. The timeline for each MCO may differ as well.
How Medwave Can Help
At Medwave, we specialize in billing, credentialing, and payer contracting. We know that managing the credentialing process on your own takes valuable time away from patient care. Our team can handle your Medicaid credentialing from start to finish, ensuring your application is complete, accurate, and submitted promptly. We track all deadlines, respond to verification requests, and keep you informed throughout the process. Whether you’re applying for the first time or going through recredentialing, Medwave can simplify the process and help you get approved faster.
Staying Compliant After Credentialing
Once you’re credentialed, staying compliant with Medicaid requirements is essential. This means keeping your provider information up to date. If you move your practice, add a new location, or change your contact information, notify Medicaid right away. Similarly, if you obtain new certifications or licenses, update your file.
You’ll also need to stay current with continuing medical education requirements and maintain appropriate malpractice insurance coverage. Keep good records of all your CME activities, you’ll need to provide this documentation during recredentialing.
Billing compliance is equally important. Follow all Medicaid billing guidelines, document services thoroughly, and never bill for services you didn’t provide. Medicaid conducts audits, and billing violations can result in serious consequences, including loss of your credentials, fines, or legal action.
Summary: Medicaid Credentialing
 Getting credentialed with Medicaid requires effort and patience, but it’s an achievable goal that can benefit both your practice and your community. By following the steps outlined in this guide and staying organized throughout the process, you’ll be well on your way to becoming a Medicaid provider. Remember that while the initial credentialing process takes time, it gets easier with recredentialing, especially once you’ve established a good track record.
Getting credentialed with Medicaid requires effort and patience, but it’s an achievable goal that can benefit both your practice and your community. By following the steps outlined in this guide and staying organized throughout the process, you’ll be well on your way to becoming a Medicaid provider. Remember that while the initial credentialing process takes time, it gets easier with recredentialing, especially once you’ve established a good track record.
Whether you choose to handle credentialing yourself or work with a professional service like us at Medwave, the key is to start early, be thorough, and stay responsive throughout the process. Your future Medicaid patients will be grateful that you took the time to join their network of providers.

