Every healthcare organization faces the same frustrating problem. You recruit a talented physician, negotiate a great contract, and set a start date. Then credentialing begins, and suddenly everything crawls to a halt. Weeks turn into months. The provider sits idle, unable to see patients. Revenue that should be flowing in never materializes.
This scenario plays out thousands of times across healthcare facilities every year. The culprit isn’t lazy staff or incompetent administrators. It’s credentialing bottlenecks, those stubborn obstacles that turn what should be a straightforward process into a months-long ordeal.
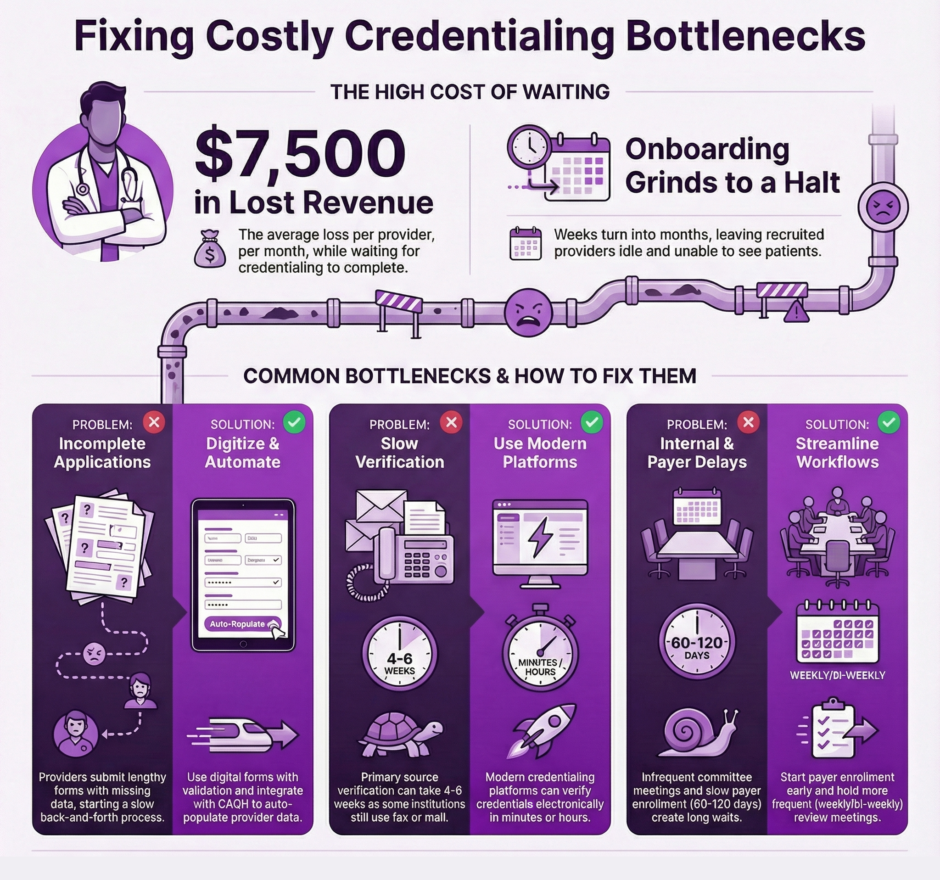
The financial impact is staggering. Healthcare organizations lose an average of $7,500 per provider per month while waiting for credentialing to complete. For a group practice bringing on three new physicians, that’s over $22,000 lost every month where the process drags.
But there’s good news. Once you identify where bottlenecks occur and what causes them, you can take specific actions to speed up the process. This article explores the most common credentialing bottlenecks and practical solutions to get providers seeing patients faster.
The Application Bottleneck: Where Most Delays Start
The credentialing journey begins when a provider submits their application. This seems simple enough, but it’s actually where many of the biggest problems start. Application forms are often lengthy, confusing, and demand information that applicants don’t have readily available.
Think about what a typical credentialing application requires:
- Work history for the past 10 years with exact dates and addresses
- Details about every hospital privilege, license, and certification ever held
- Explanations for any gaps in employment
- References with current contact information
- Malpractice history going back years
Providers are busy people. They’re wrapping up responsibilities at their current job, possibly relocating, and juggling family obligations. So they submit applications with blank spaces, approximated dates, or missing documents. The application hits your desk incomplete, and now the back-and-forth begins.
Every email requesting additional information adds days or weeks to the timeline. The provider might not respond immediately because they’re in clinic or surgery. When they do respond, they might not provide exactly what you need, requiring another follow-up.
How to Fix Application Bottlenecks
- Use digital applications with built-in validation that won’t let providers submit incomplete forms
- Integrate with CAQH to automatically populate application forms instead of making providers manually enter data
- Create a pre-submission checklist with tips like “Check with your previous employer for exact dates before submitting”
- Assign a point person who can answer provider questions in real-time during the application process
- Provide clear instructions with examples for sections that commonly cause confusion
The Primary Source Verification Bottleneck: The Waiting Game
Once you have a complete application, the real waiting begins. Primary source verification, where you confirm credentials directly with the original source, is crucial for patient safety but notoriously slow. Medical schools, licensing boards, and certifying organizations aren’t set up to respond quickly. Some still operate by fax or postal mail. Response times of 4 to 6 weeks are common.
The problem compounds when you’re verifying multiple credentials for a single provider. A physician might have degrees from two institutions, licenses in three states, and certifications from two specialty boards. That’s seven separate verifications, each potentially taking weeks.
Common verification challenges include:
- High volumes and limited staff at verification sources
- Errors and discrepancies that require additional research
- Outdated contact information for verification sources
- Systems that still rely on fax or postal mail
How to Fix Primary Source Verification Bottlenecks
- Use modern credentialing platforms that verify credentials electronically in minutes or hours instead of weeks
- Submit verification requests immediately upon receiving a complete application rather than waiting
- Establish relationships with verification sources and use expedited services when available
- Track verification requests closely and follow up proactively at the 4-week mark rather than waiting 6 weeks
- Build a library of contact information for common verification sources with specific department contacts
The Internal Review Bottleneck: When Your Process Gets in the Way
After gathering all necessary information and verifications, applications move to internal review. This should be straightforward since all the hard work of collecting information is done. But many organizations create their own bottlenecks through inefficient review processes.
Common internal review problems:
- Committee meetings scheduled only once a month create built-in delays of 3 to 4 weeks
- Manual file preparation takes time and creates opportunities for errors
- Committee members receive packets right before meetings without time to review properly
- Decision documentation takes days or weeks after the committee actually approves applications
How to Fix Internal Review Bottlenecks
- Schedule committee meetings bi-weekly or weekly instead of monthly to cut waiting time
- Use digital file management so committee members can access applications electronically anytime
- Send files out at least a week before meetings so members can review them in advance
- Implement consent agendas for routine applications that meet all standard criteria
- Automate decision documentation and notifications so providers learn their status immediately
- Empower staff to complete more review before applications reach the committee
The Payer Enrollment Bottleneck: The Final Hurdle
Even after your credentialing committee approves a provider, they still can’t see patients with insurance until they’re enrolled with payers. Insurance companies have their own credentialing processes that must be completed before they’ll pay claims from a new provider. Timeline estimates range from 60 to 120 days, and some payers take even longer.
The challenge multiplies because each payer operates independently. A provider might need enrollment with 10 or 15 different insurance plans to see the patient population your facility serves.
Payer enrollment challenges:
- Each insurance company has its own application requirements and timelines
- Some payers still use paper applications that must be mailed and manually processed
- Incomplete applications get rejected and returned for corrections, adding weeks
- Payers require specific document formats that differ from your internal credentialing needs
How to Fix Payer Enrollment Bottlenecks
- Start payer enrollment applications before your internal credentialing process finishes
- Use CAQH for payer enrollment since most major commercial payers accept CAQH attestations
- Assign staff who specialize in payer enrollment and know the quirks of different insurance companies
- Maintain templates and checklists specific to each major payer to ensure complete applications
- Follow up proactively at day 45 instead of waiting until day 90 to check on application status
- Build relationships with payer representatives who can help expedite applications when needed
The Communication Bottleneck: When Information Doesn’t Flow
Poor communication creates bottlenecks throughout the credentialing process. Providers don’t know what’s needed from them. Staff members don’t coordinate with each other. Committee members lack context for applications. Everyone operates with incomplete information, leading to delays and mistakes.
Communication problems include:
- Providers hear nothing for weeks and don’t know if applications were received or are complete
- Internal gaps mean staff doesn’t know organizational priorities for which applications to rush
- Committee questions that arise between meetings sit unanswered for 3 to 4 weeks
- Payer requests for additional information go to email addresses that aren’t monitored regularly
How to Fix Communication Bottlenecks
- Implement automated status updates for providers at key milestones like application receipt and committee review
- Create a centralized tracking system visible to all credentialing staff and relevant administrators
- Establish regular weekly check-ins between credentialing staff and hiring managers
- Use collaborative tools that allow asynchronous communication among committee members between meetings
- Set up dedicated communication channels with major payers and know who to contact for questions
Putting It All Together: A Faster Path Forward
Credentialing bottlenecks aren’t inevitable. They result from outdated processes, inadequate technology, poor communication, and systems that weren’t designed with speed in mind. Each bottleneck has known solutions that organizations can implement to dramatically reduce timelines.
Steps to eliminate bottlenecks:
- Map your current credentialing process from application submission through payer enrollment
- Document how long each step takes and where applications typically get stuck
- Prioritize bottlenecks based on their impact on overall timelines
- Invest in technology that automates manual processes and enables electronic verification
- Train staff on best practices and measure performance with specific metrics
- Communicate timelines clearly to providers from day one
The most effective credentialing processes combine smart technology with experienced staff who know how to work with providers, verification sources, and payers efficiently. They build parallel workflows so multiple steps happen simultaneously rather than sequentially. They communicate clearly and frequently with all stakeholders. And they continuously measure performance to identify and eliminate new bottlenecks as they emerge.
Summary: Speed Matters for Your Organization and Your Providers
 Every day a credentialed provider sits idle represents lost revenue, frustrated patients who need care, and potentially a demoralized new hire questioning their decision to join your organization. Credentialing bottlenecks are expensive, fixable problems that too many healthcare organizations simply accept as inevitable.
Every day a credentialed provider sits idle represents lost revenue, frustrated patients who need care, and potentially a demoralized new hire questioning their decision to join your organization. Credentialing bottlenecks are expensive, fixable problems that too many healthcare organizations simply accept as inevitable.
At Medwave, we specialize in credentialing along with medical billing and payer contracting. We’ve seen how credentialing delays impact healthcare organizations financially and operationally. Our approach focuses on identifying bottlenecks in your specific process and implementing targeted solutions that deliver measurable results.
Your credentialing process directly affects your ability to recruit providers, maintain adequate staffing, and generate revenue. In competitive healthcare markets, providers have choices about where to work. Organizations known for fast, smooth credentialing have an advantage attracting talent. Those known for drawn-out, frustrating credentialing processes struggle to recruit and sometimes lose candidates who accept offers elsewhere rather than wait.
Take a hard look at your credentialing bottlenecks. Where do applications get stuck? What causes the longest delays? What frustrates your staff and your providers? The answers point you toward the improvements that will make the biggest difference. With focused effort and the right tools, you can cut credentialing timelines substantially, getting qualified providers seeing patients faster and improving your organization’s financial performance in the process.

