Provider credentialing can feel like learning a new language when you first encounter it. The terminology, timelines, and requirements seem designed to confuse rather than clarify. Credentialing is just a systematic process of verifying that healthcare providers have the qualifications they claim and getting them approved to bill insurance companies. Once you know the steps, it becomes manageable.
What Provider Credentialing Actually Means
 At its core, credentialing is verification. Insurance companies, hospitals, and healthcare facilities need proof that providers are who they say they are and can do what they claim they can do. This means verifying medical school degrees, state licenses, board certifications, work history, and malpractice insurance. The process protects patients, reduces liability for healthcare organizations, and ensures providers meet specific quality standards.
At its core, credentialing is verification. Insurance companies, hospitals, and healthcare facilities need proof that providers are who they say they are and can do what they claim they can do. This means verifying medical school degrees, state licenses, board certifications, work history, and malpractice insurance. The process protects patients, reduces liability for healthcare organizations, and ensures providers meet specific quality standards.
Without proper credentialing, providers can’t bill insurance companies for their services. They can’t admit patients to hospitals. They can’t participate in Medicare or Medicaid programs. In practical terms, lack of credentialing means lack of income. A physician might be brilliant and highly trained, but if they’re not credentialed, they’re unemployable in most healthcare settings.
The credentialing process has grown more rigorous over the years. Regulatory requirements have tightened, verification standards have become more demanding, and insurance companies face increasing pressure to ensure network providers meet quality benchmarks. What used to take a few weeks now takes months. What used to require basic documentation now demands primary source verification from original institutions.
The Main Players in Credentialing
Several organizations play critical roles in the credentialing ecosystem, and knowing who does what helps you work more efficiently.
- CAQH (Council for Affordable Quality Healthcare) operates the primary database that most commercial insurance companies use for provider credentialing. Providers enter their information once into CAQH ProView, and participating payers can access that information directly. This eliminates the need to fill out separate applications for each insurance company. However, your CAQH profile must be complete, accurate, and attested every 120 days to remain active.
- NPPES (National Plan and Provider Enumeration System) manages the NPI (National Provider Identifier) system. Every healthcare provider needs an NPI to bill for services. Individual providers get Type 1 NPIs, while organizations get Type 2 NPIs. Your NPI follows you throughout your career and serves as your universal identification number across all payers and healthcare systems.
- PECOS (Provider Enrollment, Chain and Ownership System) is the CMS portal for Medicare enrollment. Any provider wanting to see Medicare patients must enroll through PECOS. The system collects detailed information about ownership, practice locations, and provider backgrounds. Medicare enrollment typically takes 60-90 days and requires meticulous attention to detail, as CMS rejects applications for even minor errors.
- State Medical Boards license physicians and other healthcare providers to practice within their states. Every state has different requirements, renewal schedules, and continuing education mandates. Providers practicing in multiple states need separate licenses for each one, and letting any license lapse creates immediate credentialing problems.
- Credentialing Verification Organizations (CVOs) are third-party companies that handle primary source verification for hospitals, health systems, and sometimes insurance companies. These organizations contact medical schools, training programs, licensing boards, and previous employers to verify credentials directly from the source.
The Complete Credentialing Lifecycle
Credentialing isn’t a one-time event. It’s an ongoing cycle that starts before a provider joins your practice and continues throughout their employment. Here’s how the lifecycle unfolds.
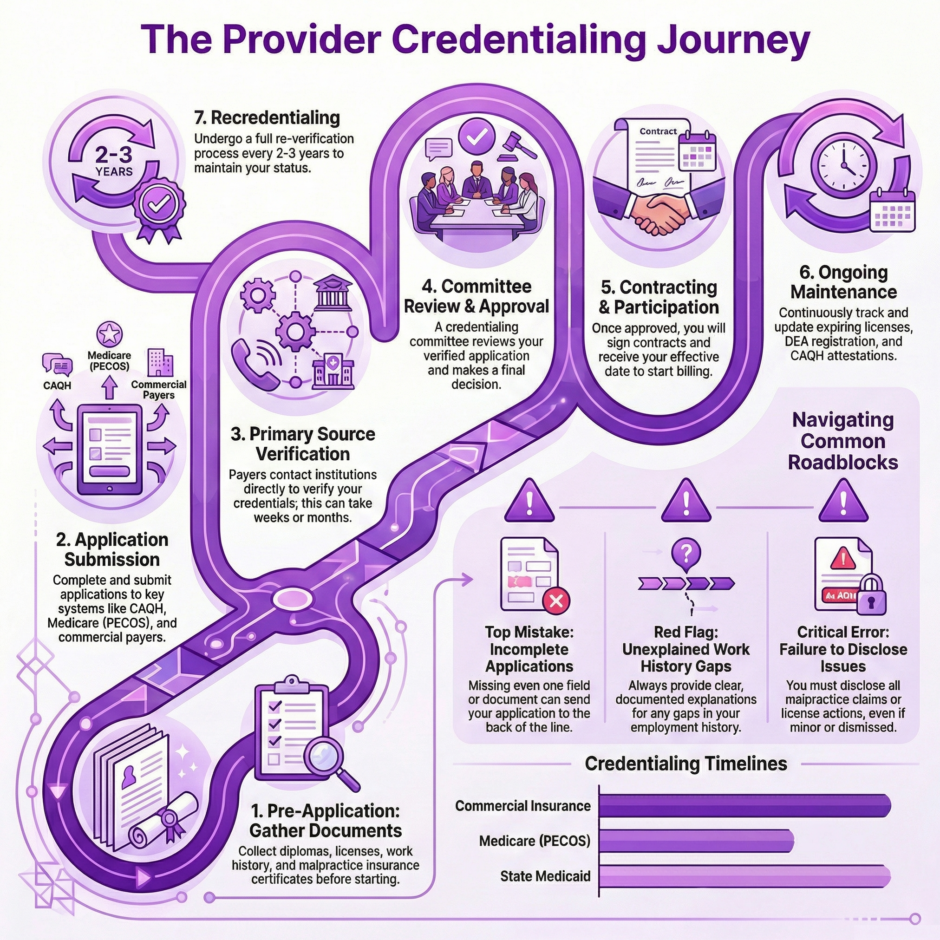
- Pre-Application Phase begins as soon as you decide to hire a new provider. Smart practices start gathering documents and preparing applications months before the provider’s official start date. You’ll need copies of medical school diplomas, residency certificates, state licenses, DEA registrations, board certifications, malpractice insurance policies, and detailed work history. Creating a checklist for each provider ensures nothing gets missed.
- Application Submission involves completing applications for CAQH, Medicare (if applicable), Medicaid (if applicable), and individual commercial payers. Each application asks for similar information but in slightly different formats. Some accept electronic submissions, others require paper applications mailed to specific addresses. Attention to detail matters enormously here because incomplete applications get rejected or delayed.
- Primary Source Verification happens behind the scenes after you submit applications. Credentialing organizations contact medical schools to verify degrees, state boards to confirm licenses, certification boards to validate specialty certifications, and previous employers to check work history. This verification process takes weeks or months depending on how responsive these organizations are.
- Committee Review occurs after verification completes. Insurance companies, hospitals, and health systems have credentialing committees that review applications and make decisions about approval, denial, or requests for additional information. Committee meetings typically happen monthly, so if your application just misses a meeting, you’re waiting another month before it gets reviewed.
- Approval and Contracting comes next if the committee approves your application. You’ll receive contracts to sign, effective dates for participation, and sometimes welcome packets with billing information and contact details. At this point, your provider can finally start seeing patients with that particular insurance.
- Ongoing Maintenance continues throughout the provider’s employment. CAQH profiles need quarterly attestation. Licenses, certifications, and DEA registrations have expiration dates that require tracking. Malpractice insurance renewals need documentation updates. Any changes in practice location, name, or employment status trigger credentialing updates.
- Recredentialing happens every 2-3 years with most payers. This process re-verifies that providers maintain their qualifications and haven’t developed any issues like malpractice claims or license restrictions. Recredentialing takes less time than initial credentialing but still demands careful attention to prevent credential lapses.
Essential Documents Every Provider Needs
Gathering the right documentation upfront prevents delays and rejected applications.
Here’s what you’ll need for virtually every credentialing application:
Educational Documents:
- Medical school diploma
- Medical school transcripts
- Residency completion certificate
- Fellowship certificates (if applicable)
- Continuing medical education records
Licenses and Registrations:
- Current state medical license for each state of practice
- DEA registration certificate (if prescribing controlled substances)
- State controlled substance licenses (if required)
- ACLS/BLS certifications
- Specialty-specific certifications
Professional History:
- Detailed work history for past 5-10 years with no gaps
- Explanation letters for any employment gaps
- Hospital privileges documentation
- Previous practice affiliations
- Professional references (typically 3-5 required)
Insurance and Legal Documents:
- Current malpractice insurance certificate showing coverage limits
- Malpractice claims history for past 10 years
- Any disciplinary actions or sanctions (must be disclosed)
- Medicare/Medicaid opt-out forms (if applicable)
Common Credentialing Mistakes That Cost Time and Money
Certain errors appear repeatedly in credentialing applications, causing unnecessary delays. Avoiding these mistakes keeps your credentialing on track.
- Incomplete applications top the list of problems. Leaving even one field blank or missing one document sends your application to the bottom of the pile until you provide what’s missing. Credentialing committees won’t review incomplete applications, so that one missing document can cost you months of waiting.
- Expired credentials create headaches when providers submit licenses, certifications, or insurance policies that expire during the credentialing process. If your medical license renews in two months and credentialing takes three months, you’ll need to provide the renewed license mid-process, adding delays.
- Work history gaps raise red flags with credentialing committees. Any unexplained gap in employment requires documentation. Whether it was family leave, additional training, sabbatical, or something else, you need to explain and document it. Leaving gaps unexplained triggers requests for additional information.
- Inconsistent information across documents causes problems. If your name appears as “John Andrew Smith” on your medical license but “J.A. Smith” on your DEA certificate and “John Smith” on your malpractice policy, payers request clarification. Standardize how information appears on all documents to avoid these questions.
- Failure to disclose malpractice claims, license actions, or hospital privilege issues constitutes dishonesty in credentialing applications. Even if a claim was dismissed or an action was minor, you must disclose it. Non-disclosure can result in permanent denial and difficulty getting credentialed anywhere else.
- Not following up regularly allows applications to stall. Credentialing departments handle hundreds of applications, and yours can easily get overlooked without regular status checks. Calling every two weeks to check progress keeps your application moving and identifies problems early.
Timeline Expectations for Different Credentialing Types

Credentialing timelines vary significantly depending on which type of credentialing you’re pursuing and which organizations are involved. Setting realistic expectations helps you plan appropriately.
Commercial insurance credentialing with major carriers like Aetna, Cigna, United Healthcare, and Anthem typically takes 90-120 days from application submission to approval. Some move faster, others slower. Regional carriers may process applications more quickly or more slowly than national companies depending on their internal processes.
Blue Cross Blue Shield credentialing operates through state associations, and each state has its own timeline. Some BCBS associations approve applications in 60-90 days, others take 120 days or longer. BCBS credentialing almost always requires separate applications for each state where you practice, even though the national brand is the same.
Medicare enrollment through PECOS averages 60-90 days for clean applications with no errors or missing information. Applications with problems can take months longer as you respond to requests for additional documentation. Medicare also requires enrollment in each state where you provide services, including telehealth.
Medicaid credentialing varies wildly by state. Some states process applications in 60-90 days, others take six months or longer. Medicaid programs are notorious for slow processing, poor communication, and applications that seem to disappear into black holes. Starting Medicaid credentialing early prevents major delays in seeing patients who depend on that coverage.
Hospital privileging for physicians typically takes 90-180 days depending on the hospital’s credentialing department efficiency and how often their medical staff committee meets. Teaching hospitals and large health systems may move faster because they have dedicated credentialing teams. Smaller community hospitals might take longer because credentialing is handled by fewer staff members.
Multi-State Credentialing Challenges
Providers practicing in multiple states face significantly more credentialing work. Each state requires its own medical license, and each payer requires separate credentialing for each state where you practice. A physician licensed in Pennsylvania, New Jersey, and Delaware needs separate credentials with every insurance company in all three states.
Some states participate in interstate licensure compacts that streamline the licensing process. The Interstate Medical Licensure Compact allows physicians to expedite licensing in multiple states through a single application. However, not all states participate, and even with compact licensing, you still need separate payer credentialing in each state.
Border area practices serving patients in multiple states need particularly careful credentialing planning. Insurance companies increasingly allow providers near state borders to see patients from adjacent states, but this requires specific credentialing arrangements and documentation of your service area.
Telehealth providers face multi-state credentialing even if their physical office is in just one location. Seeing patients via video across state lines requires medical licenses in each state where patients are located, along with appropriate insurance credentialing for each state’s payers.
Specialty-Specific Credentialing Considerations

Different medical specialties face unique credentialing requirements beyond basic provider credentialing. Knowledge of these specialty-specific needs prevents surprises during the application process.
Surgeons need hospital privileges documentation showing which procedures they’re credentialed to perform. Many insurance companies want proof of minimum case volumes for certain procedures before approving providers to perform them. Surgical specialties also face more intensive peer review and references from other surgeons.
Behavioral health providers including psychiatrists, psychologists, clinical social workers, and licensed counselors have profession-specific licensing requirements that vary significantly by state. Many behavioral health providers also face closed insurance panels, meaning some insurance companies aren’t accepting new behavioral health providers at all due to network saturation.
DME suppliers providing durable medical equipment need supplier credentialing separate from provider credentialing. This includes facility inspections, accreditation from organizations like ACHC or Joint Commission, surety bonds, and detailed inventory management documentation.
Laboratory and diagnostic testing facilities require CLIA certification, CAP accreditation (for some), and facility-specific credentialing beyond individual provider credentials. These facilities also need technical director credentialing and documentation of quality control procedures.
Managing Credentialing for Growing Practices
As your practice grows, credentialing becomes more complicated. You’re tracking credentials for multiple providers, managing various renewal dates, and ensuring everyone stays current with all payers.
Creating robust tracking systems prevents credential lapses. Spreadsheets work for small practices, but dedicated credentialing software becomes necessary as you grow. Track application submission dates, expected completion dates, renewal dates for all licenses and certifications, CAQH attestation deadlines, and recredentialing due dates.
Designating a credentialing coordinator or working with an outside credentialing service becomes essential when you have more than 2-3 providers. One person needs responsibility for monitoring all credentialing activities, following up with payers, responding to requests for additional information, and ensuring nothing falls through the cracks.
Building buffer time into your hiring process accounts for credentialing delays. If you need a provider to start seeing patients on January 1st, extend the job offer by late summer and start credentialing immediately. This ensures approvals are ready or nearly ready when the provider begins work.
Technology and Credentialing
 Credentialing technology has improved significantly in recent years, though plenty of manual work remains. CAQH ProView serves as the foundation for commercial insurance credentialing, allowing providers to maintain one profile that multiple payers can access. However, CAQH doesn’t eliminate all redundant work because many payers still require supplemental applications beyond CAQH information.
Credentialing technology has improved significantly in recent years, though plenty of manual work remains. CAQH ProView serves as the foundation for commercial insurance credentialing, allowing providers to maintain one profile that multiple payers can access. However, CAQH doesn’t eliminate all redundant work because many payers still require supplemental applications beyond CAQH information.
Electronic credentialing portals are becoming more common. Medicare’s PECOS system operates entirely online. Many commercial payers now accept electronic application submissions through their provider portals. Some state Medicaid programs have moved to online applications, though many still require paper submissions.
Primary source verification is becoming more automated through database checks and electronic verification systems. The National Student Clearinghouse allows electronic degree verification from many medical schools. License verification often happens through online state medical board databases. However, some credentials still require manual verification through phone calls, emails, and mailed requests to institutions.
Credentialing management software helps practices track multiple providers across multiple payers with automated reminders for upcoming renewals and recredentialing deadlines. These systems can store documents, track application status, and generate reports showing credentialing status across your entire provider panel.
When to Outsource Credentialing
Many practices eventually decide that credentialing requires too much specialized knowledge and time to handle internally. Outsourcing to credentialing experts makes sense in several situations.
New practices starting from scratch benefit enormously from credentialing expertise. Getting your initial credentials right the first time prevents delays in opening your doors and seeing patients. Credentialing services know exactly what each payer requires and can navigate the process efficiently.
Practices adding multiple providers simultaneously often lack the internal capacity to handle that much credentialing work at once. Hiring three new physicians means credentialing them with 15-20 payers each, which overwhelms most internal staff.
Multi-state practices face exponentially more credentialing work because every state requires separate licensing and separate payer credentialing. Managing credentials across multiple states requires dedicated attention that many practices can’t provide internally.
Practices experiencing credentialing problems like repeated denials, excessive delays, or credential lapses need expert help to fix systemic issues. Credentialing services can identify what’s going wrong and implement proper procedures.
How Medwave Simplifies Provider Credentialing
 At Medwave, we specialize in billing, credentialing, and payer contracting for healthcare practices of all sizes. Our credentialing team handles the entire credentialing lifecycle so you can focus on patient care instead of paperwork.
At Medwave, we specialize in billing, credentialing, and payer contracting for healthcare practices of all sizes. Our credentialing team handles the entire credentialing lifecycle so you can focus on patient care instead of paperwork.
We start credentialing as soon as you hire a new provider, gathering all required documents, creating CAQH profiles, submitting applications to all relevant payers, and following up consistently until approvals come through. Our established relationships with insurance company credentialing departments help expedite processing when possible.
We track every deadline for every provider across all licenses, certifications, insurance policies, CAQH attestations, and recredentialing requirements. You’ll never miss a renewal or let credentials lapse because our systems alert us months in advance of any expiration dates.
For multi-state practices, we manage separate licensing and credentialing in each state where you operate. We know which states participate in licensure compacts, which payers require separate applications for each state, and how to coordinate everything efficiently.

