Moving your medical practice to a new location sounds exciting until you hit the credentialing reality. Whether you’re shifting to a new state, opening a second office across town, or expanding into border regions, the credentialing process can feel like starting from scratch. Honestly…? Sometimes it is.
Let’s talk about what actually happens when you relocate and how to manage the credentialing maze without losing your mind or your revenue stream.
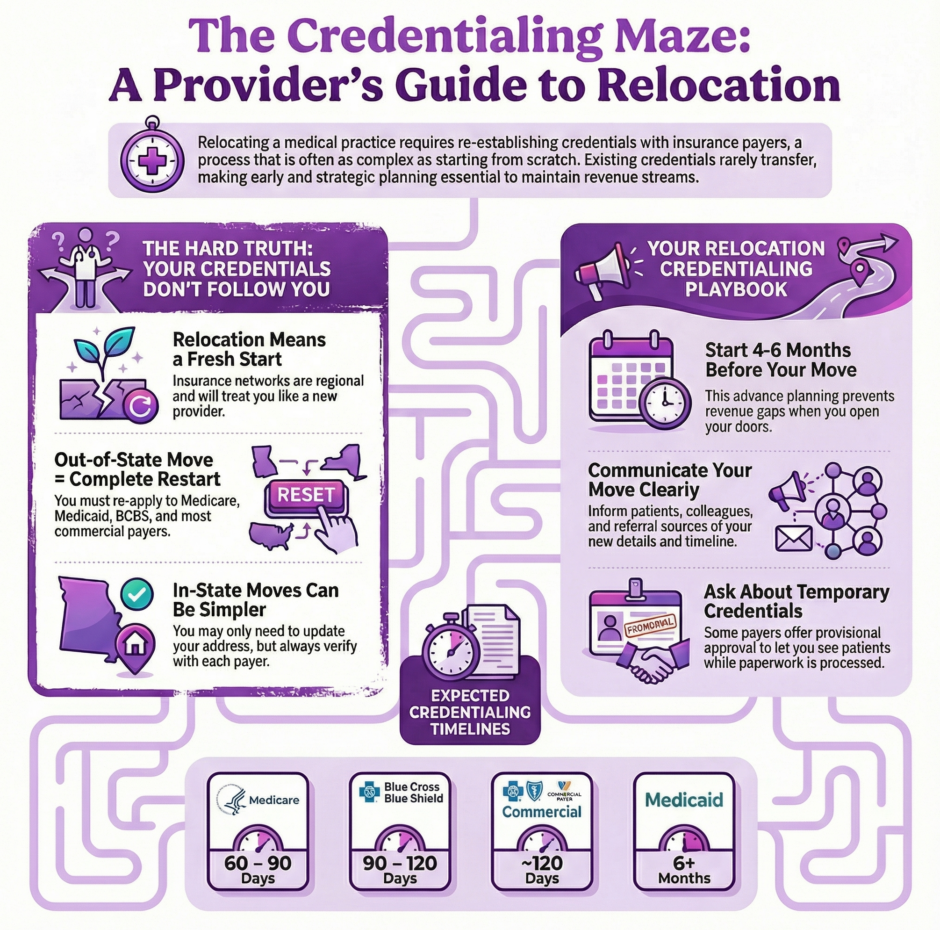
The Hard Truth About Relocation Credentialing
 Here’s what catches most providers off guard: your credentials don’t automatically follow you. Even if you’re staying with the same insurance companies you’ve worked with for years, even if you’re moving just one state over, you’re likely looking at a fresh credentialing process. That Blue Cross contract you had in Pennsylvania? It doesn’t transfer to your new New Jersey office. Your Aetna credentials in Texas won’t carry over to Oklahoma.
Here’s what catches most providers off guard: your credentials don’t automatically follow you. Even if you’re staying with the same insurance companies you’ve worked with for years, even if you’re moving just one state over, you’re likely looking at a fresh credentialing process. That Blue Cross contract you had in Pennsylvania? It doesn’t transfer to your new New Jersey office. Your Aetna credentials in Texas won’t carry over to Oklahoma.
Why? Because insurance networks operate regionally. Each state has its own Blue Cross Blue Shield association with separate contracts and credentialing requirements. National carriers like Cigna, Aetna, and UnitedHealthcare might have the same name everywhere, but they manage provider networks at the state or regional level. Your previous credentialing file provides zero benefit when you’re setting up in a new location.
This regional structure means you’re essentially a new provider in the eyes of most payers when you relocate. The credentialing committees in your new state haven’t reviewed your application. The local network hasn’t approved your participation. Your old approvals, sadly, mean nothing in your new territory.
Moving Within the Same State or Area
If you’re staying within the same general area or state, you might catch a break. The key is verifying whether your current credentials remain valid for your new location. Start by contacting your insurance companies directly. Provide your NPI number and name, then ask about your current standing and what happens if you change office locations.
In many cases, you can transfer your association from one practice group to another without starting over. This is particularly true if you’re joining an established group that already has contracts with your payers. The transition involves switching your billing association from your old group’s NPI to the new group’s NPI. Once that switch happens, you continue billing and providing services under the new group’s contract.
The process sounds simple because it often is, but don’t skip the verification step. Confirm everything before you make any changes. Get confirmation in writing if possible. The last thing you need is to assume everything transferred smoothly only to have claims denied because the payer never updated their records.
Working with Multiple Groups Simultaneously
 Here’s something that surprises people, you can be credentialed with multiple groups at the same time, even under the same insurance company. This flexibility works great for providers taking part-time positions with different practices or covering multiple locations.
Here’s something that surprises people, you can be credentialed with multiple groups at the same time, even under the same insurance company. This flexibility works great for providers taking part-time positions with different practices or covering multiple locations.
Each group bills under its own contract and NPI, and you show up as a network provider under each one. Your individual provider number (NPI) stays the same, but you’re associated with multiple group billing entities. This arrangement doesn’t affect your autonomy as a provider. You’re still practicing medicine according to your own clinical judgment, just billing through different entities depending on where you’re working that day.
The critical piece is making sure each group properly credentials you and that your associations are correctly documented with each payer. If Group A credentials you but Group B assumes you’re automatically covered, you’ll have billing problems when Group B submits claims.
The Out-of-State Relocation Challenge
Moving to a different state triggers a complete restart of the credentialing process with virtually every payer. Yes, even national insurance companies. That Medicare enrollment you had in Florida? You need a new one in North Carolina. Your BCBS contract in Ohio? Starting fresh in Michigan.
Each state has different administrators handling these programs. Medicare uses Medicare Administrative Contractors (MACs) that operate by state or region. You must submit a complete enrollment package to the MAC administering your new state’s program. This includes enrolling both your business entity and yourself individually to obtain new Provider Transaction Numbers (PTANs). Plan on 60-90 days for Medicare to process everything, assuming you submit a clean application with no errors.
Blue Cross Blue Shield operates through state associations, and your contract absolutely does not travel with you. Some exceptions exist in border areas where BCBS associations have reciprocal agreements, but these are rare. Generally, you’re applying for credentialing and contracting as if you’ve never worked with BCBS before. Allow 90-120 days for completion.
Commercial insurance credentialing follows similar patterns. Most networks require new applications, primary source verification, committee review, and fresh contracts for your new location. A handful of national PPO networks might only need a new contract issued, but that’s the exception, not the rule. Most companies treat you as a brand new applicant. Typical timeline? Around 120 days, though some move faster and others slower.
The Medicaid Maze
 State Medicaid programs are completely separate entities, and enrolling in one state doesn’t help you in another. Like Medicare, most Medicaid programs require you to enroll both your business entity and individual providers separately.
State Medicaid programs are completely separate entities, and enrolling in one state doesn’t help you in another. Like Medicare, most Medicaid programs require you to enroll both your business entity and individual providers separately.
The frustrating part? Medicaid credentialing is notoriously slow. Some states take six months or longer just to credential a single provider. Many are transitioning to electronic applications that should improve turnaround times, but plenty still use paper-based systems with poor tracking and processing controls. If Medicaid patients make up a significant portion of your practice, start this process as early as possible. Seriously, the earlier the better.
Border State Considerations
Practicing near state borders or planning to see patients in multiple states creates unique situations. Some insurance companies recognize that providers naturally serve patients across state lines and have developed processes to handle this. Others remain rigid about their state-by-state credentialing requirements.
Your best move is contacting provider relations representatives directly and asking specific questions about your situation. Can they expedite multi-state credentialing? Do they have streamlined processes for border area providers? Will they consider your existing credentials when processing new state applications?
The worst they can say is no. But many payers have solutions in place for these scenarios because they’re increasingly common. You won’t know unless you ask, and asking might save you months of processing time.
Communicating Your Move to Patients
Your patients need to know about your relocation well before moving day arrives. Early, clear communication prevents confusion and maintains the trust you’ve built. Send notices through multiple channels: email, postal mail, patient portals, and in-office signage. Consider sending several notifications as the move date approaches rather than one single announcement.
Include specific details in your communications:
- Your new address and contact information
- Your moving date
- How the move affects their care
- Whether their insurance will still work at the new location
- Alternative providers if the move means you can no longer serve them
That last point matters especially for out-of-state moves. If your relocation means some patients can no longer see you because you won’t be in their insurance network, help them find alternatives. Provide referrals, offer to transfer records, and make the transition as smooth as possible. Patients remember how you handled difficult situations.
Keeping Colleagues and Referral Sources Informed
 Professional relationships drive much of healthcare practice, and your colleagues need to know about your move. Reach out personally to your closest professional contacts through calls, emails, or face-to-face meetings. These relationships are too valuable to risk damaging through poor communication.
Professional relationships drive much of healthcare practice, and your colleagues need to know about your move. Reach out personally to your closest professional contacts through calls, emails, or face-to-face meetings. These relationships are too valuable to risk damaging through poor communication.
For your broader professional network, send formal announcements with details about your new location and how you’ll handle ongoing referrals. If you have patients with active treatment plans that span your move date, discuss transition plans with referring providers. Will you complete current treatment courses before moving? Will you transfer care to another provider? How will you ensure continuity?
Clear communication maintains referral relationships and professional respect in your new setting. Referral sources need to know they can still count on you, even if your address changes.
Managing Medical Records Transfer
Transferring medical records requires careful attention to patient privacy and continuity of care. Obtain written consent from patients before transferring their records to your new location. Use only HIPAA-compliant methods for transfer to ensure data privacy and security.
Once records transfer successfully, notify patients and provide information on accessing them at your new location. If you’re using a new electronic health record system at your new practice, plan extra time for data migration and ensure nothing gets lost in translation.
Checking Your Contracts
 Before you start any credentialing process related to relocation, review your existing contracts. Some agreements include language about location changes, credentialing transfers, or network expansion. Your contract might outline specific procedures you need to follow when relocating or adding new practice locations.
Before you start any credentialing process related to relocation, review your existing contracts. Some agreements include language about location changes, credentialing transfers, or network expansion. Your contract might outline specific procedures you need to follow when relocating or adding new practice locations.
Don’t hesitate to contact provider relations representatives or insurance company customer service lines for clarification. Ask specific questions about your situation. Can they transfer any existing credentials? Do they have expedited processes for providers in good standing? What documentation do they need to process your new location application?
These representatives deal with relocation questions regularly and can often provide shortcuts or solutions you wouldn’t find in standard application materials. They can also tell you exactly what to expect timeline-wise, helping you plan your move more effectively.
Planning Your Credentialing Timeline
Timing is everything when relocating a medical practice. Start credentialing processes 4-6 months before your planned move date, maybe even earlier for particularly slow payers. This advance planning means approvals are waiting when you open your doors at the new location rather than having you sit idle while applications process.
Create a tracking system for each payer showing:
- Application submission date
- Expected completion date
- Follow-up dates and contact information
- Any issues or requests for additional information
- Approval status
Check in regularly with payers on application status. Squeaky wheels get attention, and gentle persistence often speeds up processing. If a payer requests additional information, provide it immediately. Delays in responding extend your timeline significantly.
What About Temporary Credentials?
Some insurance companies offer temporary or provisional credentials that let you start seeing patients while full credentialing processes. These temporary approvals typically last 90-120 days, giving you time to generate revenue while paperwork moves through committees.
Ask every payer whether they offer temporary credentialing options. Not all do, but for those that do, it can bridge the gap between your move and full approval. Be aware that temporary credentials come with conditions. You’ll need proof of current licenses, malpractice insurance, and sometimes expedited primary source verification.
Maintaining Credentials During Transition
While focusing on new location credentialing, don’t let existing credentials lapse. Continue updating your CAQH profile quarterly. Renew licenses and certifications on schedule. Maintain malpractice insurance without gaps. Keep DEA registrations current.
Letting existing credentials expire while trying to establish new ones creates compounding problems. Stay current everywhere until your transition is complete and you’re fully operational at your new location.
How Medwave Can Help Your Relocation
 Relocating a medical practice involves dozens of credentialing tasks, tight timelines, and coordination across multiple payers. At Medwave, we specialize in billing, credentialing, and payer contracting. Our team manages relocation credentialing so you can focus on packing boxes and preparing your new space instead of chasing paperwork.
Relocating a medical practice involves dozens of credentialing tasks, tight timelines, and coordination across multiple payers. At Medwave, we specialize in billing, credentialing, and payer contracting. Our team manages relocation credentialing so you can focus on packing boxes and preparing your new space instead of chasing paperwork.
We track application deadlines, follow up with payers, handle documentation requests, and keep your credentialing moving forward. Doesn’t matter if you’re moving across town or across the country, we make sure you’re approved and ready to see patients when you open your doors. Our expertise in multi-state credentialing and payer contracting helps avoid delays that cost you revenue during transition periods.

