Getting credentialed with insurance companies should be straightforward, but for many healthcare providers, it turns into a months-long headache. You’ve spent years earning your medical degree, completing residencies, and building your practice. Yet somehow, filling out insurance forms becomes one of the most frustrating parts of starting or expanding your healthcare business.
The credentialing process determines whether insurance companies will recognize you as an in-network provider. Without it, patients either pay out-of-pocket or they go somewhere else. Neither option is good for your practice. Typically, a credentialing project involves multiple insurance companies, each with their own requirements, timelines, and quirks. When things go wrong, and they often do, providers can wait six months or longer before seeing insurance reimbursements.
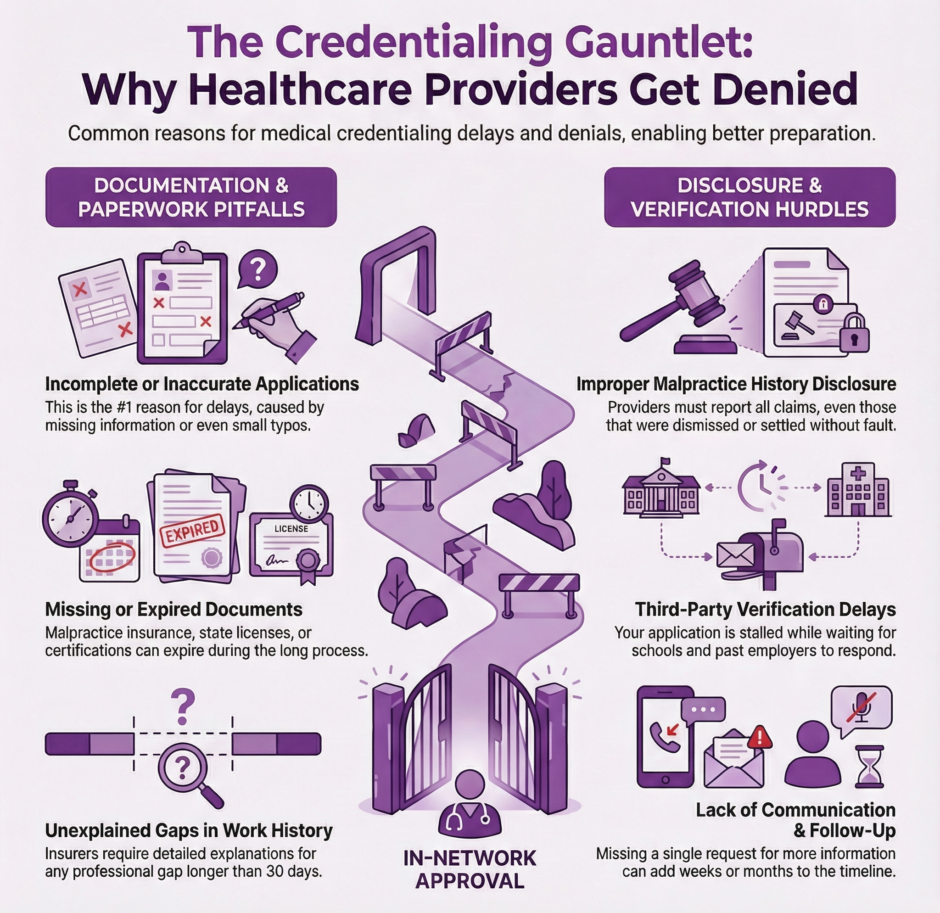
Let’s look at the most common roadblocks that delay or derail provider credentialing, and what you can do about them.
Incomplete or Inaccurate Application Materials
This is the number one reason applications get rejected or delayed. Insurance companies are incredibly picky about the information they receive. If something is missing, incorrect, or unclear, they’ll either send the application back or simply let it sit in a pile somewhere.
What makes this frustrating is that different insurance companies ask for slightly different information. One insurer might need your DEA certificate, while another wants a copy of your state license. Some require detailed employment history going back ten years, while others only want five years. Keeping track of what each company needs is like juggling plates while riding a unicycle.
Common documentation requirements include:
- DEA certificates and state medical licenses
- Employment history ranging from five to ten years back
- Detailed explanations for any gaps in work history (maternity leave, sabbaticals, career transitions)
- Professional liability insurance certificates
- Board certifications and specialty credentials
- Hospital affiliations and privileges
- Educational transcripts and diplomas
Even small mistakes can cause big delays. A misspelled name, an old address, or a signature in the wrong spot can send your application to the bottom of the pile. Some providers don’t realize they need to include explanations for any gaps in their work history. Taking six months off to have a baby or care for a sick parent? You’ll need to document that. Switching jobs without a clear transition? Better have a good explanation ready.
The paperwork itself is overwhelming. Between insurance applications, hospital privileging forms, and various licenses, providers often submit hundreds of pages of documentation. It’s easy to miss something when you’re drowning in forms.
Missing or Expired Documentation
Insurance companies want proof of everything, and timing matters just as much as having the right documents. Here’s where many providers trip up: they gather all their documents at the beginning of the credentialing process, but then forget that some of these documents have expiration dates.
Documents that commonly expire during credentialing include:
- Professional liability (malpractice) insurance policies
- State medical licenses
- DEA registrations
- Board certifications
- CPR and ACLS certifications
- Hospital privileges
- Background check authorizations
 Your malpractice insurance might expire in the middle of the credentialing process. Your state license might need renewal right when the insurance company is reviewing your application. If the insurer sees an expired document, they stop processing your application until you provide an updated version.
Your malpractice insurance might expire in the middle of the credentialing process. Your state license might need renewal right when the insurance company is reviewing your application. If the insurer sees an expired document, they stop processing your application until you provide an updated version.
Some documents are harder to obtain than others. Medical school transcripts might require a formal request and a processing fee. Previous employers might take weeks to respond to verification requests. If you trained at a hospital that has since closed or merged with another institution, tracking down your training verification can feel impossible.
Then there’s the issue of immunization records. Yes, even as a practicing physician, you need to prove you’ve had your measles, mumps, and rubella shots. Many providers don’t keep these records handy, and tracking them down from childhood doctors or college health centers can take considerable time.
Work History Gaps and Inconsistencies
Insurance companies want to account for every moment of your professional life since medical school. Any gap longer than 30 days requires an explanation. This catches many providers off guard, especially those who have taken time off for family reasons, illness, research positions, or career transitions.
The problem isn’t just having gaps, it’s properly documenting them. Insurance companies don’t just want you to say “I took time off to raise my children.” They want specific dates, and sometimes they want proof. Did you do any locum tenens work during that time? They need to verify it. Were you on sabbatical? They’ll want documentation from your previous employer.
Inconsistencies between different documents also raise red flags. If your CV says you worked at Hospital A from 2018 to 2020, but your employment verification letter says 2018 to 2019, the insurance company will have questions. These discrepancies might seem minor to you, but to a credentialing specialist reviewing hundreds of applications, they look like potential problems that need investigation.
Career changers face particular challenges. Physicians who previously worked in non-clinical roles, took time to pursue research, or worked in other countries often struggle to explain these experiences in a way that satisfies insurance company requirements.
Malpractice History and Disclosure Issues
 Any malpractice claims or settlements must be disclosed during credentialing, even if they were dismissed or settled without admission of fault. This is where honesty becomes crucial, but also where the process gets tricky.
Any malpractice claims or settlements must be disclosed during credentialing, even if they were dismissed or settled without admission of fault. This is where honesty becomes crucial, but also where the process gets tricky.
Some providers don’t realize that they need to report claims that were filed against them, even if those claims were dropped. Others forget about incidents that happened years ago. Insurance companies conduct thorough background checks, and if they find something you didn’t disclose, it looks like you were trying to hide it, even if you simply forgot.
The disclosure requirements extend beyond lawsuits.
Here are items that must be reported during credentialing:
- Any malpractice claims filed against you, even if dismissed
- Hospital privileges that were restricted, suspended, or revoked
- Medical board investigations, regardless of outcome
- DEA license questions or restrictions
- Medicare or Medicaid sanctions
- Loss of medical staff membership at any facility
- Professional liability claims settled out of court
When you do have something to report, how you explain it matters enormously. Simply stating the facts isn’t enough, you need to provide context, explain the resolution, and demonstrate what you learned from the experience. This requires thoughtful, detailed explanations that many busy providers don’t have time to craft properly.
Credential Verification Delays
Even when you submit everything perfectly, you’re at the mercy of third parties who need to verify your information. Medical schools, previous employers, and licensing boards all need to confirm your credentials, and they don’t always respond quickly.
Some organizations charge fees for verification services and take weeks to process requests. Others have outdated contact information or staff shortages. If you went to medical school overseas or trained at multiple institutions, the verification process becomes even more time-intensive.
Primary source verification is particularly slow. Insurance companies can’t just take your word that you graduated from medical school or completed your residency—they need to hear it directly from those institutions. Each verification request goes into a queue, and some organizations process these requests once a month or even less frequently.
Hospital privileging often runs parallel to insurance credentialing, which means you’re waiting on multiple organizations simultaneously. If the hospital takes six months to grant privileges, and the insurance company won’t finalize your credentialing without proof of hospital privileges, you’re stuck in a waiting game.
Poor Communication and Follow-Up
 Credentialing isn’t a one-and-done process. Insurance companies regularly request additional information, clarifications, or updated documents. If providers don’t respond quickly to these requests, their applications stall.
Credentialing isn’t a one-and-done process. Insurance companies regularly request additional information, clarifications, or updated documents. If providers don’t respond quickly to these requests, their applications stall.
The problem is that providers are busy seeing patients, managing staff, and running their practices. When a credentialing specialist emails asking for additional information, it’s easy for that request to get lost in an overflowing inbox. Missing one email can add weeks or months to the credentialing timeline.
Insurance companies also don’t always make follow-up easy. They might email from generic addresses that look like spam. They might call during clinic hours when you can’t answer. They might send physical letters to an old address. Keeping track of correspondence from multiple insurance companies while managing patient care requires dedicated time and attention that many providers simply don’t have.
Some insurance companies provide online portals for checking application status, but these portals aren’t always user-friendly or regularly updated. Providers log in expecting to see progress, only to find that their application status hasn’t changed in three months with no explanation.
State License and DEA Issues
Your state medical license and DEA registration are fundamental to credentialing, but issues with these credentials can stop the entire process. If your license is up for renewal during credentialing, or if there’s any notation or restriction on your license, insurance companies will pause everything until it’s resolved.
Some providers don’t realize they need separate licenses for different practice locations. If you see patients in multiple states, you need licenses in each state, and insurance credentialing in each state. Managing renewals across multiple states adds another layer of difficulty.
DEA registrations come with their own challenges. These need to match your practice locations exactly. If you move offices or add a new location, you need to update your DEA registration before insurance companies will credential you at that address. This seems straightforward until you realize that DEA updates can take weeks or months to process.
Any disciplinary actions, even minor ones, need extensive documentation and explanation. A late license renewal that resulted in a brief lapse? You’ll need to explain it. A complaint filed with the medical board that was dismissed? Still needs to be disclosed and documented.
Not Knowing When to Get Help
 Many providers try to handle credentialing themselves, thinking it will save money and give them more control over the process. While this approach can work, it often leads to frustration and delays. Credentialing has become increasingly technical, with each insurance company maintaining different requirements and procedures.
Many providers try to handle credentialing themselves, thinking it will save money and give them more control over the process. While this approach can work, it often leads to frustration and delays. Credentialing has become increasingly technical, with each insurance company maintaining different requirements and procedures.
Professional credentialing services exist because this process has become so time-consuming and detail-oriented that it makes more sense to outsource it. Companies like, us at Medwave, specialize in rcm, credentialing, and payer contracting, which means they know exactly what each insurance company needs, how to avoid common pitfalls, and how to keep applications moving through the system.
The cost of doing credentialing wrong or slowly often exceeds the cost of getting professional help. Every month you’re not credentialed is a month you’re either not seeing patients or not getting paid by insurance companies. For a busy practice, that can mean tens of thousands of dollars in lost revenue.
Moving Forward
Credentialing doesn’t have to be a nightmare, but it does require attention to detail, organization, and consistent follow-up. Whether you handle it yourself or work with a professional service, knowing these common issues helps you avoid them.
Here are practical steps to keep your credentialing on track:
- Start gathering documents early, at least six months before you need to be credentialed
- Create a master checklist of every document each insurance company requires
- Keep digital copies of everything in an organized cloud storage system
- Set calendar reminders three months before any credential expires
- Prepare written explanations for any work history gaps or malpractice claims
- Designate one email address specifically for credentialing correspondence
- Check application status weekly and follow up on anything pending over 30 days
- Keep a spreadsheet tracking each insurance company’s application status and required documents
Be honest and thorough in your disclosures. It’s always better to over-explain than to leave questions unanswered. If you have gaps in your employment history or any malpractice history, prepare clear, factual explanations in advance.
 Respond quickly to any requests for additional information. Consider setting up a separate email folder for credentialing correspondence so nothing gets lost. If you’re not getting responses from insurance companies, follow up regularly, the squeaky wheel really does get the grease in credentialing.
Respond quickly to any requests for additional information. Consider setting up a separate email folder for credentialing correspondence so nothing gets lost. If you’re not getting responses from insurance companies, follow up regularly, the squeaky wheel really does get the grease in credentialing.
Most importantly, be patient but persistent. Credentialing takes time under the best circumstances, but staying on top of the process prevents small delays from becoming major setbacks. Your future patients, and your practice revenue, depend on it.

