Healthcare providers have been sounding the alarm for years, but the federal government shutdown that stretched through October and into early November 2025 made it impossible to ignore. Critical telehealth programs and hospital-at-home waivers remain tied to short-term spending legislation, turning them into hostages every time Congress fights over the budget.
When the shutdown finally ended, Medicare telehealth waivers came back. But the relief was temporary. Healthcare organizations found themselves right back in the same exhausting cycle they’ve lived through repeatedly since the COVID-19 public health emergency ended. They advocate for extensions, prepare backup plans for potential gaps in coverage, and operate under constant uncertainty about whether their programs will be funded beyond the next few months.
This isn’t how you run a healthcare system. It’s crisis management dressed up as policy.
What Actually Happened During the Shutdown
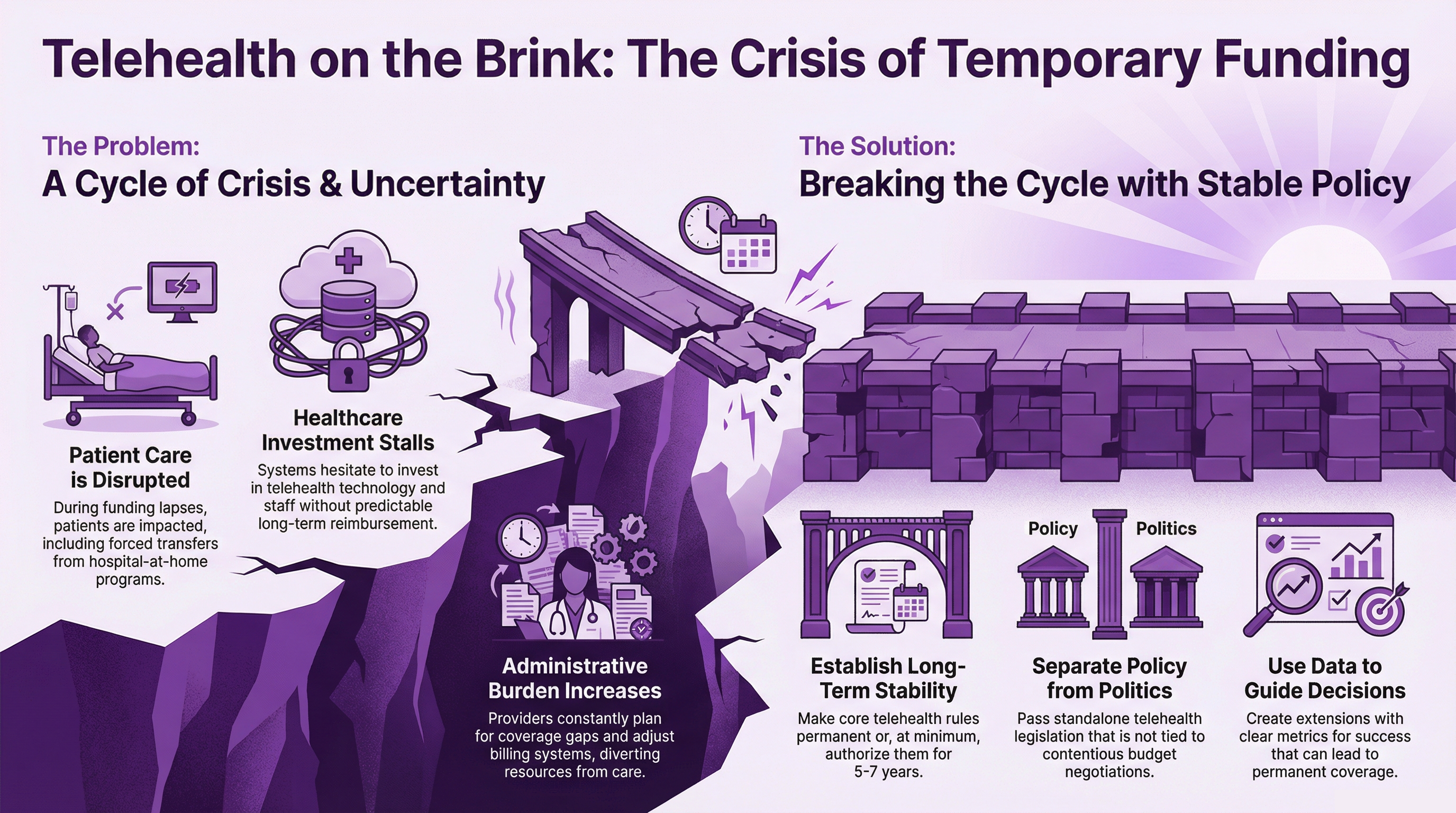
 The federal government shutdown didn’t just inconvenience bureaucrats. It disrupted actual patient care. Medicare telehealth waivers expired because they were attached to the spending bill that finances the federal government. When that bill lapsed, the waivers went with it. Hospital-at-home programs got caught in the same mess.
The federal government shutdown didn’t just inconvenience bureaucrats. It disrupted actual patient care. Medicare telehealth waivers expired because they were attached to the spending bill that finances the federal government. When that bill lapsed, the waivers went with it. Hospital-at-home programs got caught in the same mess.
The Centers for Medicare & Medicaid Services told hospitals that patients receiving acute care at home needed to be transferred to traditional facilities or discharged. Healthcare organizations scrambled to relocate patients who were getting hospital-level treatment in their own homes. These moves disrupted treatment plans and created nightmares for families and medical teams who had to coordinate mid-treatment transfers that served no medical purpose.
Telehealth providers serving Medicare patients in rural areas or treating people with mobility problems faced immediate problems. Services that had become routine suddenly weren’t available. Providers couldn’t bill Medicare for telehealth visits that didn’t fall under the narrow pre-pandemic coverage rules. They had to choose between providing care they couldn’t bill for or turning away patients who depended on virtual visits.
Kyle Zebley, senior vice president of public policy at the American Telemedicine Association, described the situation plainly in an interview with Chief Healthcare Executive. Even with bipartisan support for telehealth, the healthcare community “ended up the victim” of budget politics.
The Pattern: Short-Term Extensions Pretending to Be Policy
When asked about the chances for permanent reform or at least a multi-year extension, Zebley’s answer wasn’t encouraging. He predicted another short-term funding bill with another short-term extension of Medicare telehealth flexibilities and acute hospital care at home attached. “That’s how it works now, unfortunately and has worked for a few decades, and it’s getting worse every year,” he said.
This cycle didn’t start yesterday. Medicare telehealth coverage has been expanded and contracted through temporary legislative patches for years. What changed during COVID-19 was the scale. Telehealth utilization exploded when in-person care became difficult or dangerous. The Section 1135 waivers issued during the public health emergency made major changes. Medicare beneficiaries could receive telehealth services regardless of where they lived. Audio-only visits became acceptable for certain services. More types of providers could deliver telehealth. Patients could receive care at home instead of traveling to healthcare facilities.
When the public health emergency ended in May 2023, Congress extended many of these changes on a temporary basis. Then they extended them again. And again. Each extension gets tied to broader spending legislation, turning telehealth policy into a bargaining chip in budget negotiations instead of letting it be evaluated as healthcare policy on its own merits.
According to the Medicare Payment Advisory Commission (MedPAC), telehealth utilization among Medicare fee-for-service beneficiaries peaked at approximately 52 visits per 1,000 beneficiaries per month during the height of the pandemic. By 2024, utilization had stabilized at roughly 35 to 40 visits per 1,000 beneficiaries monthly. That’s substantially higher than pre-pandemic levels but well below the pandemic peak. The numbers suggest telehealth has found a sustainable role in Medicare coverage, filling gaps in access without replacing in-person care entirely.
Yet, despite evidence that telehealth has become integrated into normal care delivery, Congress keeps treating it as a temporary experiment that needs periodic reauthorization.
Why Permanent Reform Stays Out of Reach
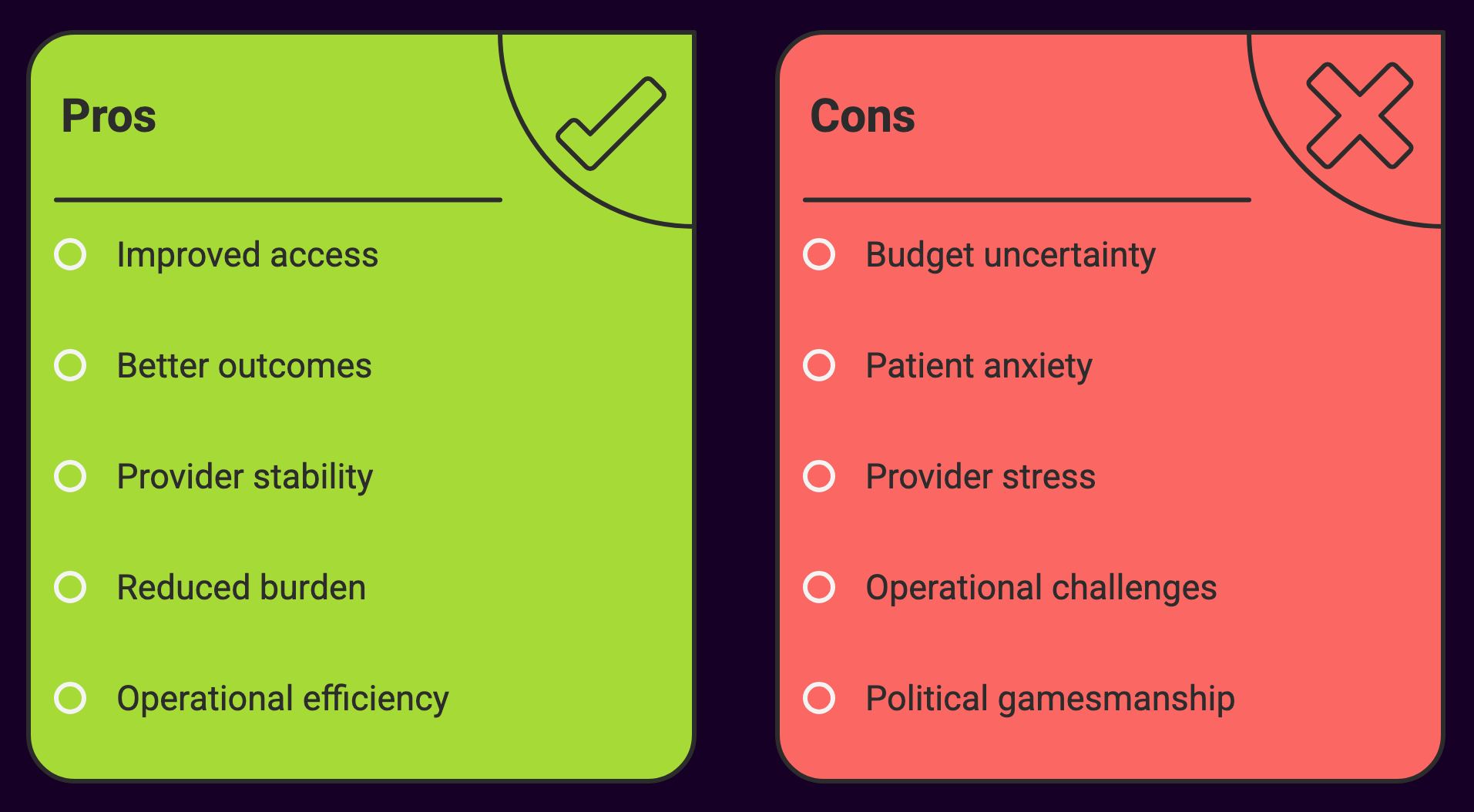
 The political situation makes no sense on the surface. Telehealth has broad bipartisan support. Rural legislators recognize that telehealth helps constituents who live hours from specialty care. Urban representatives see telehealth addressing transportation barriers and improving access for disabled and elderly constituents. Provider organizations across specialties support permanent telehealth flexibilities. Patient advocacy groups consistently lobby for continuation.
The political situation makes no sense on the surface. Telehealth has broad bipartisan support. Rural legislators recognize that telehealth helps constituents who live hours from specialty care. Urban representatives see telehealth addressing transportation barriers and improving access for disabled and elderly constituents. Provider organizations across specialties support permanent telehealth flexibilities. Patient advocacy groups consistently lobby for continuation.
As Zebley noted, “I say that, totally being grateful for bipartisan support. Never will we as a community take that for granted. But despite all that support and despite all that gratitude that we’ve shown for it, we still have ended up the victim here.”
So why hasn’t Congress made these changes permanent? Several factors explain the lack of progress:
Budget Scoring
The Congressional Budget Office must calculate the cost of making telehealth flexibilities permanent. Expanding covered services increases federal spending in CBO projections, even if telehealth potentially reduces costs by preventing emergency department visits, hospital admissions, or disease complications. Budget rules prioritize short-term spending projections over potential long-term savings, making permanent expansions harder to justify financially than temporary extensions.
Fraud and Abuse Concerns
Some policymakers remain worried about fraud risk in telehealth, particularly for behavioral health services and in Medicare Advantage. The Department of Health and Human Services Office of Inspector General has issued reports highlighting vulnerabilities in telehealth billing. Their concerns include questions about medical necessity for services provided without established patient-provider relationships and potential for inappropriate prescribing in audio-only visits.
These concerns aren’t made up. Telehealth fraud schemes have resulted in significant enforcement actions. But the solution should be targeted anti-fraud measures, not blanket restrictions on legitimate telehealth services. Permanent telehealth coverage with strong program integrity safeguards would work better than periodic temporary extensions with minimal oversight.
Competing Priorities
Healthcare policy competes with numerous other legislative priorities. In budget negotiations, telehealth extensions often get bundled into larger packages rather than receiving standalone consideration. This means telehealth policy becomes secondary to broader fiscal debates about government funding, debt limits, and spending levels.
Legislative Mechanics
Passing permanent reforms requires different legislative processes than extending existing temporary policies. Extensions can be included in continuing resolutions and omnibus spending bills through relatively streamlined procedures. Permanent reform would likely require committee consideration, hearings, and potentially reconciliation with other healthcare policies. The path of least resistance is another short-term extension.
The Cost of Uncertainty
The policy uncertainty creates real costs for healthcare organizations in several ways:
Investment Decisions
Health systems hesitate to invest in telehealth infrastructure when they can’t predict whether Medicare will reimburse for services beyond the next few months. Expanding telehealth capacity requires capital investment in technology platforms, training staff, establishing workflows, and ensuring regulatory compliance. Organizations struggle to justify these investments when the return depends on temporary policy extensions that might disappear.
Workforce Planning
Hiring clinicians specifically for telehealth roles or training existing staff on virtual care delivery requires confidence that those capabilities will remain billable. Uncertainty about telehealth coverage makes workforce planning difficult, particularly for rural hospitals and community health centers where telehealth may be essential for maintaining access to care.
Patient Expectations
Patients who have integrated telehealth into their routine care don’t grasp why coverage periodically disappears due to Congressional budget fights. The whiplash of services being available, then unavailable, then available again undermines patient confidence and creates confusion about what’s covered under their benefits.
Administrative Burden
Healthcare organizations must constantly monitor legislative developments, prepare contingency plans for potential lapses, communicate with patients about coverage changes, and adjust billing systems repeatedly as policies change. This administrative overhead diverts resources from patient care. Companies like Medwave, which provide billing, credentialing, and payer contracting services to healthcare providers, find themselves helping clients prepare for policy changes that may or may not happen, then scrambling to implement changes when extensions pass at the last minute.
Hospital-at-Home: Collateral Damage
 The hospital-at-home waiver has become collateral damage in telehealth policy uncertainty. The Acute Hospital Care at Home waiver, launched during COVID-19, allows hospitals to provide acute inpatient care to appropriate patients in their homes while billing at inpatient rates.
The hospital-at-home waiver has become collateral damage in telehealth policy uncertainty. The Acute Hospital Care at Home waiver, launched during COVID-19, allows hospitals to provide acute inpatient care to appropriate patients in their homes while billing at inpatient rates.
Research on hospital-at-home programs has shown promising results. A study published in the Journal of the American Geriatrics Society found that hospital-at-home care was associated with lower costs, shorter lengths of stay, fewer lab tests and procedures, and lower rates of delirium compared to traditional inpatient care. Patient satisfaction scores were consistently higher for home-based acute care.
Despite this evidence, the waiver remains temporary and tied to telehealth extensions. During the shutdown, CMS directed hospitals to transfer patients receiving acute care at home to traditional facilities or discharge them. This forced mid-treatment relocations that served no clinical purpose whatsoever.
Hospital systems that invested in building hospital-at-home programs face the same uncertainty as telehealth providers. Will this waiver be extended again, or will they need to wind down programs that improve outcomes and reduce costs?
What Happens Next
Zebley’s prediction for the immediate future offers little comfort. He expects the healthcare community will be “back in that circumstance, at the very least for this next measure that will reopen the federal government.” Translation: another short-term extension tied to the next spending bill.
The pattern is likely to continue. Temporary extensions measured in months rather than years, each requiring renewed advocacy, each creating another potential gap in coverage, each perpetuating uncertainty for providers and patients.
Zebley expressed hope that “this lapse will be a rallying cry that will prove to policy-makers the error of their ways.” He argued for building “a case for why we need permanency, and again, if not permanency, at the very least a multi-year extension of these flexibilities.”
But hope isn’t policy. And rallying cries have been issued before without producing lasting change.
Breaking the Cycle
Breaking this cycle requires Congress to treat telehealth as core healthcare policy rather than a budget bargaining chip.
Several approaches could achieve this:
Permanent Baseline Coverage with Periodic Review
Make core telehealth flexibilities permanent while requiring CMS to report to Congress annually on utilization, outcomes, and program integrity. This provides stability while maintaining oversight.
Multi-Year Authorizations
If permanent coverage isn’t politically viable, authorize telehealth flexibilities for five to seven years rather than months. This allows adequate time to evaluate outcomes and provides sufficient stability for healthcare organizations to invest appropriately.
Separate Telehealth from Budget Negotiations
Pass standalone telehealth legislation outside the context of government funding bills. This allows telehealth policy to be evaluated on healthcare merits rather than fiscal bargaining dynamics.
Evidence-Based Sunset Provisions
Structure extensions with clear metrics for checking whether they’re working. If telehealth meets defined benchmarks for access, quality, and cost-effectiveness, coverage becomes permanent. If metrics aren’t met, Congress revisits the policy with actual data to guide decisions.
None of these approaches are radical. They simply apply standard policy-making practices to telehealth instead of treating it as a perpetual temporary measure.
Healthcare (Telehealth) Deserves Better
 The October and November 2025 shutdown demonstrated once again that tying essential healthcare services to short-term budget legislation creates unnecessary disruption for patients and providers. The question is whether Congress will learn from this latest gap in coverage or simply set up the next crisis a few months down the road.
The October and November 2025 shutdown demonstrated once again that tying essential healthcare services to short-term budget legislation creates unnecessary disruption for patients and providers. The question is whether Congress will learn from this latest gap in coverage or simply set up the next crisis a few months down the road.
Healthcare deserves better than governing by crisis. Patients receiving hospital-level care at home deserve not to be relocated mid-treatment because of budget politics. Rural beneficiaries who rely on telehealth for specialty care deserve certainty that those services will remain available. Healthcare organizations deserve the policy stability necessary to invest in care delivery models that improve access and outcomes.
Healthcare providers have adapted remarkably well to policy uncertainty. They’ve built contingency plans, maintained flexibility in their operations, and found ways to continue serving patients despite legislative chaos. But adaptation to dysfunction shouldn’t be necessary. The burden shouldn’t fall on providers and patients to work around Congress’s inability to make stable policy decisions.
For companies like Medwave that handle billing, credentialing, and payer contracting for healthcare providers, the constant policy shifts create operational challenges. We help our clients prepare for potential lapses, adjust their billing systems when extensions pass, and work with insurance companies to clarify coverage when rules change. But we’d much rather help providers operate under stable, predictable policies that allow them to focus on patient care rather than Congressional budget cycles.
Short-term extensions may be politically expedient, but they’re clinically and operationally disruptive. Every temporary extension means providers must prepare for the possibility that coverage will lapse. Every last-minute reauthorization means scrambling to implement changes quickly. Every budget fight that holds telehealth hostage means patients wondering whether their next appointment will be covered.
It’s time for Congress to make telehealth policy permanent, or at minimum, stable enough that patients and providers aren’t perpetually bracing for the next lapse. The evidence supporting telehealth is clear. The bipartisan support exists. The operational need is obvious. What’s missing is the political will to treat healthcare policy as more important than budget leverage.
Until that changes, healthcare providers will continue preparing for the next crisis while hoping it doesn’t come. Patients will continue wondering whether the care they depend on will be available next month or disappear again when Congress can’t agree on a budget. That’s no way to run a healthcare system, but it’s the reality we’re living with until Congress decides that healthcare access matters more than political gamesmanship.

