Provider credentialing is a critical process in the healthcare industry that ensures medical professionals meet specific standards of education, training, and experience before they can join an insurance network.
We inspect the intricacies of credentialing with Aetna, one of the largest health insurance providers in the United States, offering valuable insights for healthcare providers seeking to join the Aetna network.
Understanding Provider Credentialing
Provider credentialing is a thorough vetting process that validates a healthcare provider’s qualifications, experience, and practice history.
This process serves multiple purposes:
- Ensuring patient safety and quality of care
- Minimizing the risk of medical malpractice
- Meeting regulatory requirements
- Maintaining the integrity of the insurance network
For Aetna, this process is particularly rigorous, as they strive to maintain a network of high-quality healthcare providers for their members.
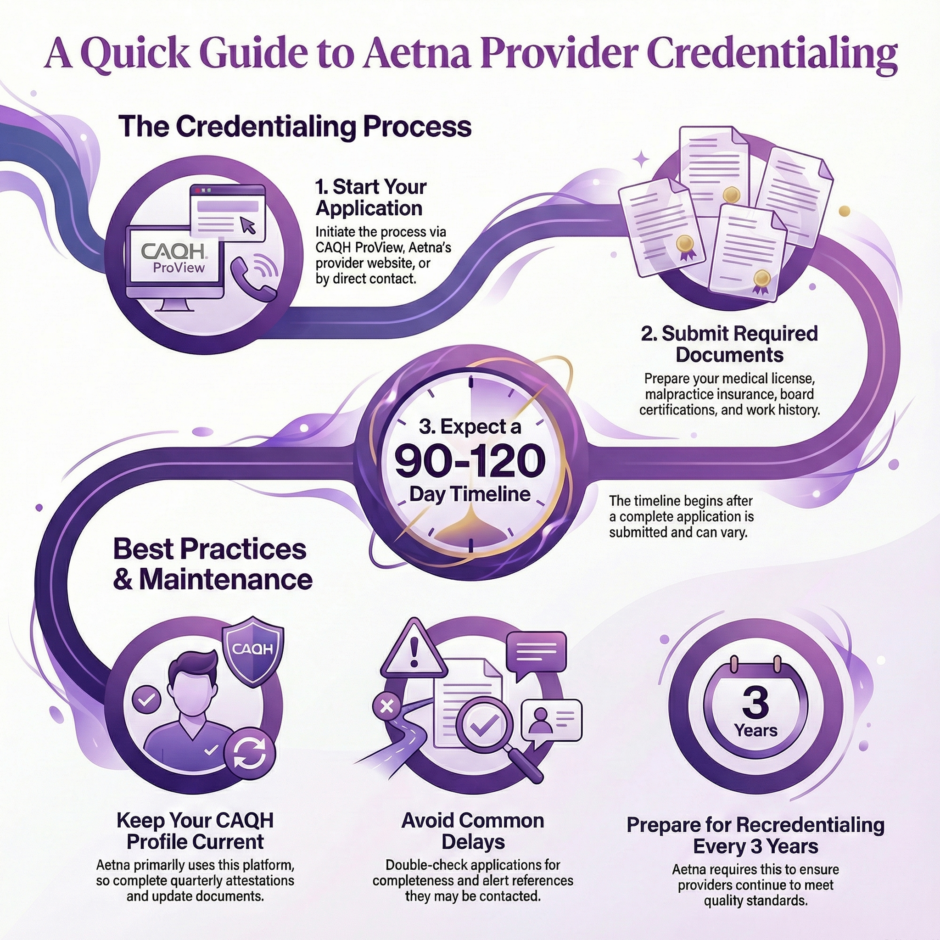
The Aetna Credentialing Process
Initial Application

The credentialing process with Aetna begins with the submission of an application.
Providers can initiate this process through:
- CAQH ProView / CAQH Provider Data Portal – The Council for Affordable Quality Healthcare’s standardized platform
- Aetna’s provider website
- Direct contact with Aetna’s Provider Relations department
Required documentation typically includes:
- Medical license
- DEA certificate (if applicable)
- Malpractice insurance documentation
- Board certifications
- Educational background verification
- Work history
- Hospital privileges
- References
Timeline and Expectations
The credentialing process with Aetna typically takes 90-120 days from the submission of a complete application.
This timeline can vary based on:
- The accuracy and completeness of the submitted information
- The responsiveness of references and verification sources
- The complexity of the provider’s history
- Current credentialing volume at Aetna
Best Practices for Successful Credentialing
Maintain Current CAQH ProView Profile
Keep your CAQH ProView / CAQH Provider Data Portal profile up-to-date, as Aetna primarily uses this platform for credentialing.
Ensure:
- Quarterly attestations are completed
- All documents are current and not expired
- Contact information is accurate
- Practice locations are updated
Prepare Documentation in Advance
Gather all necessary documentation before starting the application process:
- Verify that all licenses and certifications are current
- Ensure malpractice insurance meets Aetna’s requirements
- Prepare a complete CV detailing work history
- Have professional references ready to respond
Follow Up Regularly
Stay proactive during the credentialing process:
- Keep a record of all submitted documentation
- Follow up every 2-3 weeks for status updates
- Respond promptly to any requests for additional information
Common Challenges and Solutions
Challenge 1: Incomplete Applications
Solution: Use a credentialing checklist and double-check all requirements before submission. Consider using a credentialing specialist or service to ensure accuracy.
Challenge 2: Delays in Verification
Solution: Alert references and previous employers that they may be contacted for verification. Provide accurate contact information to expedite the process.
Challenge 3: Expired Documentation
Solution: Set up a tracking system for license and certification expiration dates. Begin renewal processes well in advance to avoid gaps.
Recredentialing with Aetna
Aetna requires recredentialing every three years. This process ensures that providers continue to meet quality standards and maintain necessary qualifications.
Recredentialing Best Practices
- Mark your calendar – Set reminders for the three-year recredentialing cycle
- Maintain documentation – Regularly update your credentials and keep records organized
- Stay compliant – Address any quality issues or complaints promptly
- Monitor performance metrics – Be aware of your quality scores and patient satisfaction ratings
Specialized Credentialing Requirements
Different specialties may have additional credentialing requirements:
Mental Health Providers
- Specific licensure requirements
- Additional documentation of specialized training
Surgical Specialists
- Detailed surgical logs
- Hospital privileges verification
Primary Care Physicians
- Patient panel information
- After-hours coverage documentation
The Role of Technology in Credentialing
Aetna has embraced technological advancements to streamline the credentialing process:
- Online portals for application submission and tracking
- Automated verification systems for certain credentials
- Digital document management for faster processing
- Integration with CAQH ProView for standardized data collection
Financial Considerations
Understanding the financial aspects of credentialing is crucial:
Costs Associated with Credentialing
- Application fees (if applicable)
- Time investment in gathering and submitting documentation
- Potential lost revenue during the credentialing process
Reimbursement Implications
- In-network status affects reimbursement rates
- Retroactive billing policies
- Impact on patient out-of-pocket costs
Legal and Compliance Aspects
Providers should be aware of the legal implications of the credentialing process:
- Accuracy of Information – Providing false information can result in serious consequences
- Disclosure Requirements – Obligation to report adverse events or changes in status
- Appeals Process – Rights and procedures for appealing credentialing decisions
- Compliance with Regulations – Understanding state and federal requirements
Maintaining Credentialed Status
Once credentialed with Aetna, providers should focus on maintaining their status:
Quality Metrics
- Monitor patient satisfaction scores
- Track clinical outcomes
- Participate in quality improvement initiatives
Compliance Requirements
- Adhere to Aetna’s policies and procedures
- Maintain accurate billing practices
- Participate in required training or education
Communication
- Keep contact information current
- Promptly report any changes in practice status
- Maintain open lines of communication with Aetna representatives
Summary: A Guide to Provider Credentialing with Aetna
![]()
Successful credentialing with Aetna requires careful preparation, attention to detail, and ongoing maintenance. Understanding the process, requirements, and best practices outlined in this article enables healthcare providers to manage the credentialing journey more effectively. Remember that credentialing is not just a bureaucratic hurdle but an important quality assurance process that benefits both providers and patients.
Staying informed about credentialing requirements and maintaining high standards of practice will ensure a successful partnership with Aetna and other insurance providers. Follow the guidelines and best practices presented here. Then, providers can approach the credentialing process with confidence and increase their chances of a smooth and successful outcome.
*If you decide to work with Medwave and you require it, please see our complete CAQH ProView Form (we do the work for you, once you’ve filled out the form). Contact us to work all of your Aetna credentialing needs and/or challenges.

