When you walk into a doctor’s office or hospital, you probably assume the medical professionals treating you are qualified to do their jobs. You trust that your surgeon actually went to medical school, that your primary care physician holds a valid license, and that the specialist you’re seeing has the right training and certifications. But who makes sure all of that is true? The answer is credentialing specialists, the unsung heroes working behind the scenes to verify that every healthcare provider meets strict standards before they can treat patients.
 Credentialing specialists serve as the gatekeepers of healthcare safety. Their work happens long before you ever step into an exam room, and most patients never know these professionals exist. Yet, their role is absolutely critical to protecting patient safety and maintaining the integrity of our healthcare system.
Credentialing specialists serve as the gatekeepers of healthcare safety. Their work happens long before you ever step into an exam room, and most patients never know these professionals exist. Yet, their role is absolutely critical to protecting patient safety and maintaining the integrity of our healthcare system.
What Credentialing Actually Means
Credentialing is the process of verifying and evaluating the qualifications of healthcare providers. This includes doctors, nurses, dentists, therapists, and any other licensed medical professional who treats patients. The process involves checking education, training, licenses, certifications, work history, and even criminal background checks.
Think of credentialing specialists as detective-investigators for the medical world. They dig through documentation, contact schools and training programs, verify licenses with state boards, check for malpractice claims, and ensure that every piece of a provider’s professional background checks out. It’s meticulous work that requires incredible attention to detail and persistence.
The stakes couldn’t be higher. When credentialing specialists miss something or skip a verification step, unqualified or dangerous individuals could end up treating patients. On the flip side, when they do their jobs well, patients can trust that the healthcare providers caring for them meet rigorous professional standards.
The Verification Process: More Than Just Paperwork
Many people think credentialing is just shuffling papers and filling out forms. In reality, it’s an intensive investigation that can take weeks or even months to complete.
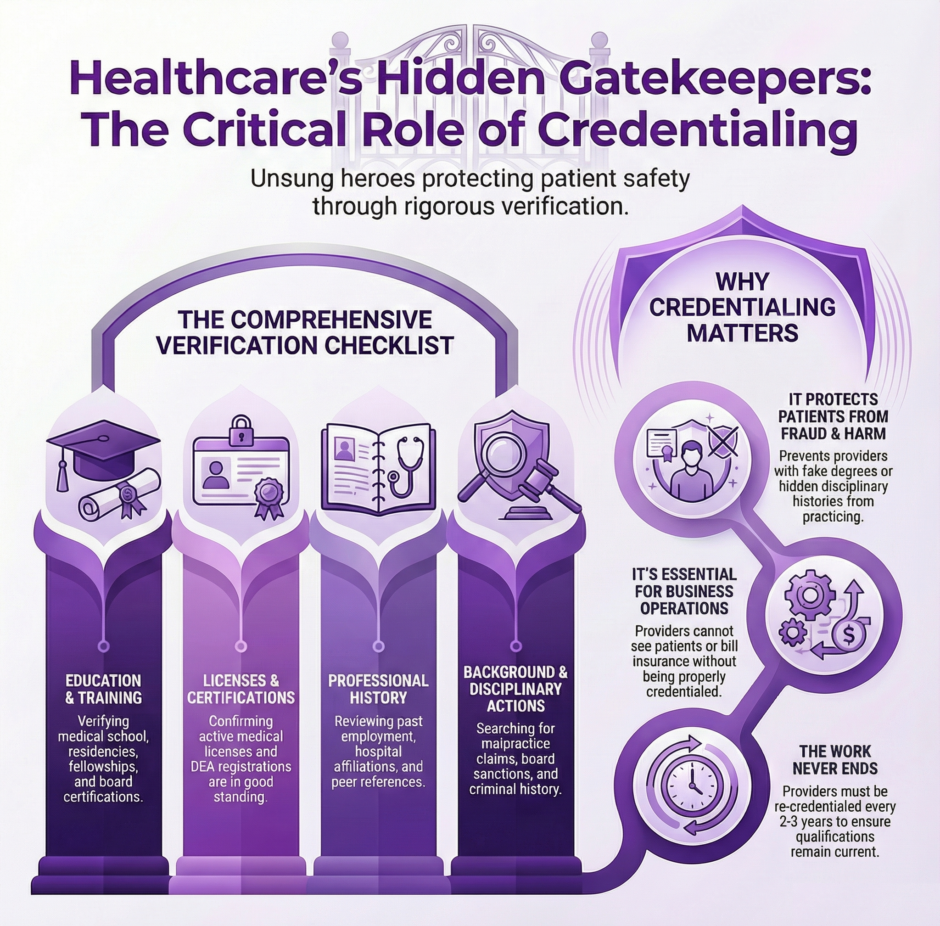
Here’s what credentialing specialists actually verify:
Education and Training
- Medical school attendance and graduation
- Residency program completion
- Fellowship training for specialists
- Continuing education requirements
- Board certifications in specific medical specialties
Licenses and Certifications
- Active medical licenses in good standing
- DEA registration for prescribing controlled substances
- State-specific licenses for practice locations
- Specialty board certifications
- CPR and other required certifications
Professional History
- Previous employment and clinical privileges
- Peer references from other medical professionals
- Hospital affiliations and credentialing status
- Any gaps in work history that need explanation
- Volume and types of procedures performed
Background Checks
- Criminal history searches
- Malpractice claims and settlements
- Disciplinary actions by medical boards
- Medicare and Medicaid sanctions
- National Practitioner Data Bank reports
Each of these categories requires contacting multiple sources, waiting for responses, following up on missing information, and documenting everything thoroughly. A single credentialing file can contain hundreds of pages of documentation by the time the process is complete.
Why This Work Matters
 You might wonder why healthcare organizations can’t just take a doctor’s word that they’re qualified. Unfortunately, credential fraud does happen. Some individuals have practiced medicine with fake degrees, lapsed licenses, or hidden disciplinary histories. Without thorough credentialing, these dangerous situations would occur far more often.
You might wonder why healthcare organizations can’t just take a doctor’s word that they’re qualified. Unfortunately, credential fraud does happen. Some individuals have practiced medicine with fake degrees, lapsed licenses, or hidden disciplinary histories. Without thorough credentialing, these dangerous situations would occur far more often.
Consider what could happen without proper credentialing. A surgeon could claim expertise in a procedure they’ve never actually performed. A doctor with multiple malpractice suits could move to a new state and start fresh without anyone knowing their history. Someone who lost their medical license in one state could simply practice in another. Credentialing specialists prevent these scenarios by verifying every claim and checking every credential against primary sources.
Beyond preventing fraud, credentialing also ensures quality. Healthcare organizations want the best providers on their teams. By thoroughly vetting qualifications and checking references, credentialing specialists help identify providers who not only meet minimum requirements but excel in their fields. This benefits patients, healthcare organizations, and insurance companies alike.
The Insurance Company Connection
Credentialing doesn’t just happen when a provider joins a hospital or medical practice. It also occurs when providers want to join insurance networks. If you’ve ever wondered why your doctor accepts some insurance plans but not others, credentialing is often part of the answer.
Insurance companies maintain panels of approved providers who can treat their members. Before a doctor can join an insurance panel, they must go through the insurer’s credentialing process. This is separate from the credentialing that happens when joining a hospital or practice, which means providers often go through multiple credentialing processes throughout their careers.
Insurance credentialing presents its own challenges. Each insurance company has slightly different requirements and timelines. Some process applications quickly, while others take months. During this waiting period, providers can’t see patients with that insurance or bill for their services. This creates financial strain for medical practices and limits patient access to care.
Credentialing specialists who work with insurance panels must stay current on each company’s specific requirements, track application status, and follow up persistently to move things along. They serve as the liaison between healthcare providers and insurance companies, translating requirements and ensuring nothing falls through the cracks.
Recredentialing: The Work Never Ends
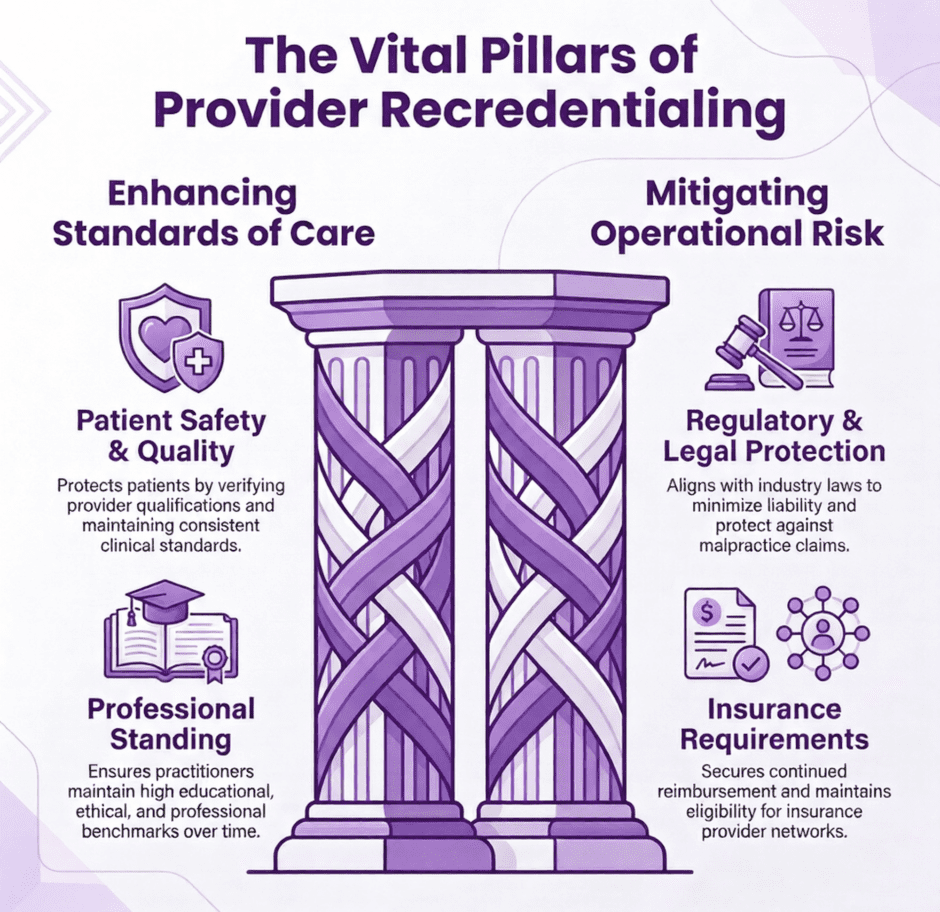
Here’s something most people don’t realize, credentialing isn’t a one-time event. Healthcare providers must be recredentialed periodically, typically every two to three years. This means credentialing specialists are constantly working through renewals while also processing new applications.
Recredentialing involves reverifying all the same information that was checked initially. Licenses must still be active. Board certifications need to be current. New malpractice claims or disciplinary actions must be investigated. Work history since the last credentialing must be documented. It’s essentially starting the whole process over again.
The recredentialing cycle creates an ongoing workload that never truly ends. For a large hospital system with hundreds of providers, credentialing specialists are always juggling multiple files at various stages of completion. Missing a recredentialing deadline can result in a provider losing their privileges or being removed from insurance panels, which directly impacts their ability to work and earn income.
The Skills Required
Becoming a credentialing specialist requires a unique combination of skills. It’s not a job that just anyone can do well. The most important qualities include:
Attention to detail is paramount. Missing a single expired license or overlooking a disciplinary action could have serious consequences. Credentialing specialists must carefully review every document and catch any discrepancies or red flags.
Persistence matters tremendously. Getting responses from medical schools, licensing boards, and previous employers often requires multiple follow-up attempts. Credentialing specialists can’t give up when someone doesn’t respond to the first inquiry.
Organization is essential when managing dozens of files simultaneously. Each application has different requirements and deadlines. Credentialing specialists must track what’s been submitted, what’s still needed, and when follow-ups are necessary.
Communication skills help credentialing specialists work effectively with providers, administrators, and external agencies. They need to explain requirements clearly, request missing information diplomatically, and keep everyone informed about application status.
Problem-solving abilities come into play when documents are missing, licenses have lapsed, or issues arise with a provider’s background. Credentialing resources must figure out how to address these problems while following proper procedures.
The Technology Factor
 Modern credentialing has become increasingly digitized, which brings both benefits and challenges. Credentialing software can track applications, send automated reminders, and store documents electronically. Many primary sources now allow online verification of licenses and certifications, which speeds up the process.
Modern credentialing has become increasingly digitized, which brings both benefits and challenges. Credentialing software can track applications, send automated reminders, and store documents electronically. Many primary sources now allow online verification of licenses and certifications, which speeds up the process.
However, technology hasn’t eliminated the human element. Credentialing specialists still need to interpret requirements, make judgment calls about questionable information, and handle situations where automated systems don’t work as intended. Some sources still require phone calls or written requests. Not all documentation arrives in digital format.
The rise of telehealth has also created new credentialing challenges. When providers treat patients across state lines via video visits, they may need licenses in multiple states. Credentialing resources must ensure providers maintain proper licensure everywhere they practice, even virtually. This adds layers of verification and tracking to an already intensive process.
Common Challenges and Obstacles
Credentialing specialists face numerous obstacles in their daily work. Slow response times from verification sources can delay the entire process. Medical schools and licensing boards may take weeks to respond to verification requests. Previous employers might not have good record-keeping systems.
Incomplete applications from providers create extra work. When providers don’t submit all required documents or leave gaps in their work history, credentialing resources must track down missing information. This back-and-forth extends timelines and frustrates everyone involved.
Changing requirements add another layer of difficulty. Insurance companies update their credentialing requirements periodically. New regulations affect what must be verified and how. Credentialers must stay current on these changes and adjust their processes accordingly.
Issues in a provider’s background require careful handling. When malpractice claims, disciplinary actions, or license restrictions appear, credentialers must investigate thoroughly and present findings to decision-makers. These situations demand discretion and professionalism.
The Impact on Patient Care
 While credentialing happens behind the scenes, it directly affects patient care in multiple ways. Thorough credentialing protects patients from unqualified or dangerous providers. It ensures that the person treating you actually has the knowledge and skills they claim.
While credentialing happens behind the scenes, it directly affects patient care in multiple ways. Thorough credentialing protects patients from unqualified or dangerous providers. It ensures that the person treating you actually has the knowledge and skills they claim.
Efficient credentialing processes help patients access care more quickly. When providers can be credentialed and added to insurance panels promptly, patients have more choices for their healthcare. Delays in credentialing can mean patients can’t see the provider they want or must wait longer for appointments.
Quality credentialing supports better outcomes. By verifying training, certifications, and track records, credentialing helps ensure patients receive care from qualified professionals. This contributes to safer procedures, better diagnoses, and improved treatment results.
The Business Side
From a healthcare organization’s perspective, credentialing specialists provide essential business functions. Providers can’t see patients or bill for services without proper credentialing. This means credentialing directly impacts revenue and operations.
Hospitals and medical practices need credentialed providers to maintain their capacity and meet patient demand. When credentialing gets delayed, it creates gaps in coverage and forces existing providers to take on extra patients. This can lead to burnout and reduced quality of care.
Insurance credentialing determines which patients a provider can treat. If a medical practice wants to accept a particular insurance plan, their providers must be credentialed with that insurer. The more insurance panels a practice joins, the larger their potential patient base becomes.
Many healthcare organizations find credentialing so time-consuming and specialized that they outsource it to experts. Companies like Medwave specialize in credentialing alongside billing and payer contracting services. These specialized firms have dedicated teams, established relationships with verification sources, and systems designed specifically for managing credentialing workflows. By partnering with credentialing experts, healthcare organizations can ensure the work gets done thoroughly and efficiently while their internal staff focuses on patient care.
Credentialing Specialist Adaptation
 Credentialing must adapt. Interstate licensure compacts are making it easier for providers to practice across state lines, but credentialing specialists must verify compliance with these new arrangements. Value-based care models emphasize provider quality and outcomes, adding new data points for credentialing specialists to track.
Credentialing must adapt. Interstate licensure compacts are making it easier for providers to practice across state lines, but credentialing specialists must verify compliance with these new arrangements. Value-based care models emphasize provider quality and outcomes, adding new data points for credentialing specialists to track.
Cybersecurity concerns affect how sensitive credentialing information gets stored and transmitted. Credentialers must protect provider data while still sharing necessary information with insurance companies and regulatory bodies. Finding the right balance between accessibility and security remains an ongoing challenge.
The COVID-19 pandemic highlighted both the importance of credentialing and the need for flexibility. Emergency waivers allowed faster credentialing processes during the crisis, but raised questions about which requirements are truly essential versus which add bureaucratic burden without improving safety. The industry continues debating how to streamline credentialing without compromising its protective function.
Summary: Healthcare Safety Protected by Credentialing
 Credentialers are the unsung heroes who keep healthcare safe. Their meticulous verification work happens out of sight, but its impact touches every patient who receives medical care. Serving as gatekeepers who ensure only qualified providers can practice shows they play a critical role in maintaining healthcare quality and protecting public safety.
Credentialers are the unsung heroes who keep healthcare safe. Their meticulous verification work happens out of sight, but its impact touches every patient who receives medical care. Serving as gatekeepers who ensure only qualified providers can practice shows they play a critical role in maintaining healthcare quality and protecting public safety.
The next time you visit a doctor or check into a hospital, remember that credentialing specialists verified every credential, checked every license, and confirmed every certification for the people caring for you. Their dedication to thorough, accurate verification helps ensure you receive care from qualified professionals. Credentialing specialists stand guard at the gates, making sure only the best get through.

