Medical billing has become the backbone of healthcare revenue, yet it remains one of the most challenging aspects of running a medical practice. Between changing regulations, insurance requirements, and the constant pressure to reduce claim denials, billing departments are stretched thin while managing increasingly demanding workloads.
 The statistics paint a sobering picture: the average medical practice spends 14% of its revenue on billing and collection activities, with some practices spending even more. Administrative costs continue climbing while reimbursement rates face downward pressure. Meanwhile, billing staff juggle multiple systems, chase down missing information, and spend countless hours on tasks that could be automated.
The statistics paint a sobering picture: the average medical practice spends 14% of its revenue on billing and collection activities, with some practices spending even more. Administrative costs continue climbing while reimbursement rates face downward pressure. Meanwhile, billing staff juggle multiple systems, chase down missing information, and spend countless hours on tasks that could be automated.
This is where Robotic Process Automation (RPA) enters the conversation. Far from being a futuristic concept, RPA is already transforming medical billing operations across the country. By automating repetitive tasks and eliminating human error from routine processes, RPA offers a practical solution to the mounting challenges facing today’s billing departments.
The Current State of Medical Billing Challenges
Before exploring how RPA can help, it’s worth examining the specific pain points that make medical billing so resource-intensive. Most billing departments face similar challenges regardless of their size or specialty.
- Manual Data Entry and Processing
Billing staff spend enormous amounts of time manually entering patient information, procedure codes, and insurance details across multiple systems. This process is not only time-consuming but also prone to errors that can result in claim denials and delayed payments. - Insurance Verification Bottlenecks
Verifying patient insurance coverage and benefits requires staff to log into multiple payer portals, wait on hold with insurance companies, and manually update patient records with the latest information. This process can take 15-30 minutes per patient, creating significant bottlenecks in the billing workflow. - Claims Status Monitoring
Tracking the status of submitted claims requires constant vigilance. Staff must regularly check payer portals, identify claims that need attention, and follow up on denials or requests for additional information. This monitoring process is essential but extremely time-intensive. - Prior Authorization Management
Prior authorizations have become increasingly common, requiring detailed documentation and frequent follow-up with insurance companies. The process often involves multiple phone calls, faxes, and document submissions, all while managing strict deadlines that can impact patient care. - Denial Management and Appeals
When claims are denied, billing staff must analyze the reason, gather additional documentation, and resubmit or appeal the decision. This process requires significant expertise and time, and delays in addressing denials directly impact cash flow.
What RPA Brings to Medical Billing
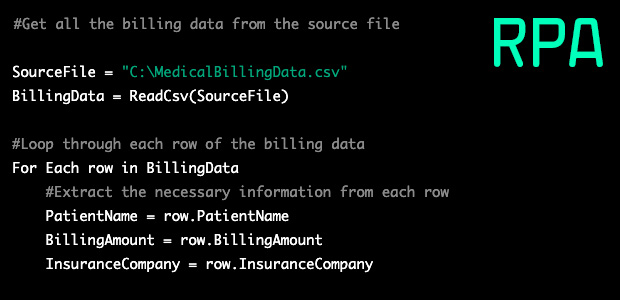
 Robotic Process Automation uses software robots to perform rule-based tasks that humans currently handle manually. In medical billing, this means automating many of the repetitive processes that consume staff time while introducing opportunities for error.
Robotic Process Automation uses software robots to perform rule-based tasks that humans currently handle manually. In medical billing, this means automating many of the repetitive processes that consume staff time while introducing opportunities for error.
RPA bots work within your existing systems, mimicking the actions that staff members currently perform. They can log into multiple applications, extract and enter data, generate reports, and even make decisions based on predefined rules. The key advantage is that these bots work continuously, never get tired, and perform tasks with perfect consistency.
For medical billing departments, this technology represents a fundamental shift from reactive to proactive operations. Instead of staff spending their day on data entry and routine follow-up tasks, RPA handles these activities automatically, allowing human workers to focus on exceptions, problem-solving, and strategic initiatives that require critical thinking and expertise.
Transforming Key Billing Processes
Patient Registration and Insurance Verification
One of the most immediate impacts of RPA in medical billing is the transformation of patient registration and insurance verification processes. Currently, these tasks require significant manual effort and are prone to errors that cascade through the entire billing cycle.
RPA bots can automatically extract patient information from various sources, including online registration forms, referral documents, and previous visit records. They can then populate your practice management system with this information while simultaneously verifying insurance coverage through payer portals.
The automation extends to real-time eligibility checking, where bots continuously monitor and update patient insurance information, ensuring that coverage details are current before services are rendered. This proactive approach prevents many billing issues that would otherwise require costly rework later in the process.
When discrepancies are identified, bots can automatically flag these cases for human review while continuing to process straightforward registrations. This exception-based workflow ensures that staff attention is focused where it’s most needed while routine cases flow through the system efficiently.
Claims Creation and Submission
 The process of creating and submitting claims involves multiple steps, each requiring attention to detail and knowledge of specific payer requirements. RPA can automate much of this workflow while maintaining the accuracy that’s critical for clean claims.
The process of creating and submitting claims involves multiple steps, each requiring attention to detail and knowledge of specific payer requirements. RPA can automate much of this workflow while maintaining the accuracy that’s critical for clean claims.
Bots can automatically extract procedure codes from clinical documentation, match them with appropriate diagnosis codes, and apply the correct billing rules for different payers. They can also verify that all required fields are completed and that the claim meets specific payer formatting requirements before submission.
Once claims are prepared, RPA can automatically submit them to the appropriate clearinghouses or directly to payers, depending on your billing workflow. The bots can also generate submission reports and update claim tracking systems, providing real-time visibility into the status of your billing pipeline.
This automation dramatically reduces the time between service delivery and claim submission, improving cash flow while reducing the manual effort required from billing staff.
Claims Status Monitoring and Follow-up
Monitoring claim status and following up on outstanding items represents a significant portion of billing department workload. RPA can automate these activities, ensuring that no claims fall through the cracks while reducing the manual effort required for routine follow-up.
Bots can automatically check claim status across multiple payer portals, identifying claims that require attention and categorizing them based on the type of action needed. For routine inquiries, bots can automatically generate and send follow-up communications, while more complex situations are flagged for human intervention.
The automation can extend to automatic resubmission of claims when appropriate, such as when a claim was rejected due to a temporary system issue or minor formatting problem. This immediate response capability can significantly reduce the time claims spend in limbo.
Denial Management and Appeals
 When claims are denied, RPA can help streamline the resolution process by automatically analyzing denial reasons and routing claims to the appropriate workflow. Bots can categorize claim denials based on the reason codes, identify those that can be automatically corrected and resubmitted, and flag complex cases that require human expertise.
When claims are denied, RPA can help streamline the resolution process by automatically analyzing denial reasons and routing claims to the appropriate workflow. Bots can categorize claim denials based on the reason codes, identify those that can be automatically corrected and resubmitted, and flag complex cases that require human expertise.
For appeals that require additional documentation, RPA can automatically generate appeal letters using templates and patient-specific information, attach relevant supporting documents, and submit appeals within the required timeframes. This automation ensures that appeals are processed promptly while maintaining the quality and accuracy required for optimal outcomes.
The Financial Impact of RPA in Medical Billing
The financial benefits of implementing RPA in medical billing extend far beyond simple cost reduction. While labor savings are significant, the real value comes from improved cash flow, reduced errors, and enhanced operational efficiency.
- Accelerated Revenue Cycle
By automating routine tasks and eliminating delays in the billing process, RPA can significantly reduce the time between service delivery and payment receipt. Claims are submitted faster, follow-up happens automatically, and issues are resolved more quickly. This acceleration in the revenue cycle improves cash flow and reduces the amount of outstanding receivables. - Reduced Error Rates
Manual processes inevitably introduce errors, and in medical billing, errors are expensive. Each denied claim requires staff time to investigate, correct, and resubmit. RPA dramatically reduces these errors by following consistent rules and validation checks. The result is higher clean claim rates and fewer resources spent on rework. - Improved Staff Productivity
When RPA handles routine tasks, billing staff can focus on activities that require human judgment and expertise. This shift typically results in higher job satisfaction and better utilization of skilled workers. Instead of hiring additional staff to handle growing volume, practices can often absorb increased workload through automation. - Enhanced Compliance and Reporting
RPA systems maintain detailed logs of all activities, providing comprehensive audit trails that support compliance efforts. Automated reporting capabilities also provide better visibility into billing performance, helping identify trends and opportunities for improvement.
Implementation Strategy for Medical Billing RPA
Successfully implementing RPA in medical billing requires a thoughtful approach that considers both technical and human factors. The goal is to achieve meaningful improvements while minimizing disruption to current operations.
- Process Assessment and Prioritization
The first step involves identifying which processes are best suited for automation. Ideal candidates are highly repetitive, rule-based tasks that don’t require complex decision-making.- Common starting points include:
- Insurance eligibility verification
- Claim status checking
- Routine correspondence generation
- Data entry and validation
- Report generation and distribution
- Common starting points include:
- Pilot Implementation
Rather than attempting to automate everything at once, most practices benefit from starting with a pilot project focused on one or two specific processes. This approach allows the team to learn how RPA works, identify potential issues, and refine the implementation before expanding to other areas. - Staff Training and Change Management
Successful RPA implementation requires buy-in from the billing team. Staff members need to learn how to work alongside automated processes and focus their attention on exceptions and higher-value activities. This transition requires training, clear communication about the benefits of automation, and ongoing support as team members adapt to new workflows. - Continuous Monitoring and Optimization
Once RPA is deployed, ongoing monitoring is essential to ensure optimal performance. This includes tracking key metrics, identifying opportunities for additional automation, and making adjustments as payer requirements or internal processes change.
Measuring RPA Success in Medical Billing
To ensure that your RPA investment delivers the expected returns, it’s important to establish baseline measurements and track improvements over time.
Key metrics to monitor include:
Operational Efficiency Metrics
- Time required to complete specific tasks
- Volume of claims processed per staff member
- Average days in accounts receivable
- Clean claim submission rates
Quality and Accuracy Measures
- First-pass resolution rates for common issues
- Error rates in data entry and claims submission
- Denial rates by payer and procedure type
- Appeal success rates
Financial Performance Indicators
- Cost per claim processed
- Staff productivity measures
- Cash collection rates and timing
- Overall billing department operating costs
These metrics provide concrete evidence of RPA’s impact and help identify areas where additional optimization might be beneficial.
Addressing Common Implementation Concerns
Medical practices considering RPA often have legitimate concerns about security, compliance, and integration with existing systems. Addressing these concerns upfront is crucial for a smooth implementation.
- Security and HIPAA Compliance
RPA solutions designed for healthcare include robust security features and maintain detailed audit trails of all activities. These systems often provide better security than manual processes because they eliminate the risk of human error in handling sensitive information. However, it’s essential to work with vendors who specialize in healthcare automation and can demonstrate compliance with all relevant regulations. - Integration with Existing Systems
Modern RPA platforms are designed to work with existing software without requiring major system changes. They interact with your current practice management and billing systems through the same interfaces that staff members use, which means implementation can proceed without disrupting current operations or requiring expensive system upgrades. - Return on Investment Timeline
While RPA requires upfront investment in software and implementation services, most medical billing operations see positive returns within 12-18 months. The ongoing operational savings, combined with improved cash flow from faster claims processing, typically provide compelling financial justification for the investment.
Automated Medical Billing of Tomorrow
 As healthcare continues to face pressure to reduce costs while improving quality, automation will become increasingly important for maintaining competitive billing operations. RPA represents the foundation of this transformation, but future developments in artificial intelligence and machine learning promise even greater capabilities.
As healthcare continues to face pressure to reduce costs while improving quality, automation will become increasingly important for maintaining competitive billing operations. RPA represents the foundation of this transformation, but future developments in artificial intelligence and machine learning promise even greater capabilities.
Predictive analytics will help identify claims likely to be denied before submission, allowing proactive correction. Natural language processing will automate the extraction of billing information from clinical notes. Advanced decision-making capabilities will handle increasingly sophisticated billing scenarios without human intervention.
Practices that implement RPA now will be better positioned to adopt these advanced technologies as they become available. They’ll have more efficient operations, better financial performance, and staff who are accustomed to working alongside automated systems.
Summary: RPA Can Save Your Medical Billing
 Robotic Process Automation offers medical billing departments a proven path to reduced costs, improved accuracy, and enhanced operational efficiency. By automating routine tasks like insurance verification, claims processing, and denial management, RPA allows billing staff to focus on complex cases and strategic initiatives that require human expertise.
Robotic Process Automation offers medical billing departments a proven path to reduced costs, improved accuracy, and enhanced operational efficiency. By automating routine tasks like insurance verification, claims processing, and denial management, RPA allows billing staff to focus on complex cases and strategic initiatives that require human expertise.
The technology delivers measurable benefits including faster revenue cycles, higher clean claim rates, and improved staff productivity. Implementation can be scaled to match your practice’s needs and resources, with most operations seeing positive returns within 12-18 months.
For medical practices seeking to optimize their billing operations while managing rising costs and increasing complexity, RPA provides a practical solution that works with existing systems and processes. The technology not only addresses current challenges but also positions billing departments for continued success as healthcare automation continues to advance.
At Medwave, we specialize in medical billing, credentialing, and payer contracting services. We recognize that RPA can significantly enhance these operations by automating routine tasks, reducing processing times, and improving accuracy across all aspects of revenue cycle management. The integration of intelligent automation with expert billing services creates powerful opportunities for improved financial performance and operational excellence.