For many organizations, credentialing remains a cumbersome, time-consuming workflow filled with inefficiencies and bottlenecks. The undermentioned content explores the nuances of credentialing workflow optimization. We break down what it is, why it matters, and how organizations can transform their approach to this essential function.
The Current Credentialing Terrain
 Credentialing, at its core, is the process of verifying that professionals have the necessary qualifications, licenses, and experience to perform their jobs effectively and safely. It’s a gatekeeper function that ensures quality, compliance, and risk management. But let’s be honest, it’s also often viewed as administrative drudgery, a necessary evil that consumes resources without adding obvious value.
Credentialing, at its core, is the process of verifying that professionals have the necessary qualifications, licenses, and experience to perform their jobs effectively and safely. It’s a gatekeeper function that ensures quality, compliance, and risk management. But let’s be honest, it’s also often viewed as administrative drudgery, a necessary evil that consumes resources without adding obvious value.
This perception exists largely because many credentialing processes remain stuck in outdated methodologies. Paper forms, manual verification calls, spreadsheet tracking, and disjointed systems create a perfect storm of inefficiency. The consequences aren’t just operational headaches, as they include delayed onboarding, revenue loss, compliance risks, and even impacts on service quality.
The good news? There’s tremendous opportunity for optimization in this space. Organizations that effectively streamline their credentialing workflows can realize significant benefits, from faster processing times to better resource allocation and improved professional satisfaction.
The Hidden Costs of Suboptimal Credentialing
Before diving into solutions, it’s worth understanding the full impact of inefficient credentialing processes:
- Delayed Revenue Generation: Every day a qualified professional waits for credentials is a day they can’t generate revenue. This is particularly acute in healthcare, where studies suggest the average credentialing delay costs between $7,000 and $15,000 per provider per month in lost billings.
- Staff Burden: Traditional credentialing processes are labor-intensive. Staff members spend countless hours chasing documentation, making verification calls, and managing follow-ups – time that could be better spent on higher-value activities.
- Compliance Risks: Manual processes increase the likelihood of errors and oversights, potentially exposing organizations to regulatory penalties, accreditation issues, and even liability claims.
- Professional Frustration: Nothing dampens a new hire’s enthusiasm faster than getting caught in a bureaucratic credentialing quagmire. This frustration can set a negative tone for the employment relationship and even lead to early attrition.
- Competitive Disadvantage: In competitive hiring markets, organizations with streamlined credentialing processes have a distinct advantage in securing top talent, as professionals increasingly factor onboarding efficiency into their employment decisions.
Core Elements of Credentialing Workflow Optimization
Meaningful optimization goes beyond simply digitizing paper forms.
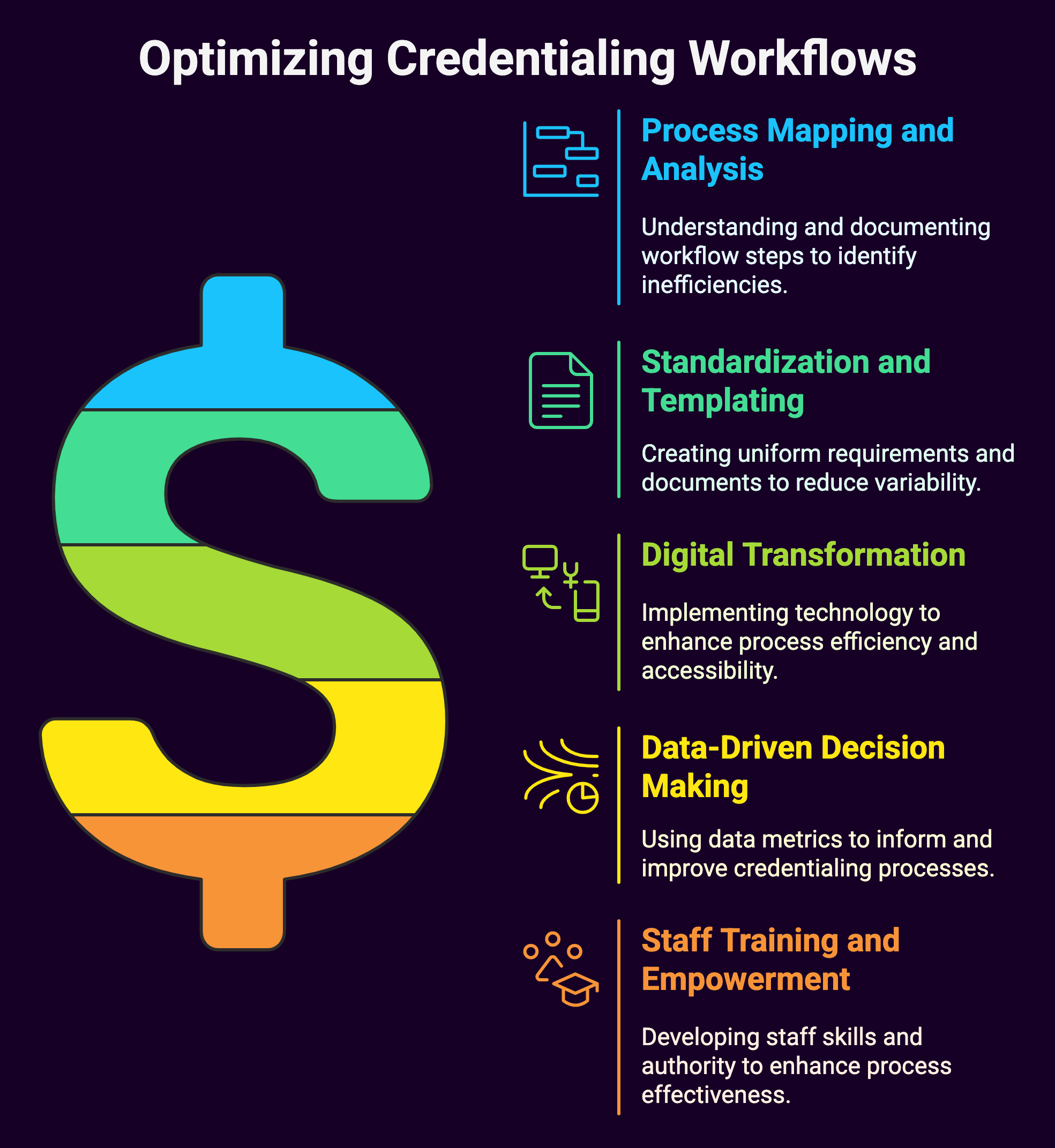
It requires a complete approach that addresses every aspect of the credentialing lifecycle:
1. Process Mapping and Analysis
The foundation of any optimization effort is a clear understanding of the current state. Process mapping involves documenting each step in the credentialing workflow, identifying decision points, handoffs, and dependencies. This exercise often reveals surprising insights about unnecessary steps, redundant approvals, or procedural relics that no longer serve their original purpose.
Key questions during this phase include:
- What triggers the credentialing process?
- What information is collected, and when?
- How many touch points exist throughout the workflow?
- Where do bottlenecks typically occur?
- Which steps add value, and which don’t?
Process analysis should also incorporate time measurements, allowing organizations to identify the longest-duration activities and prioritize them for improvement.
2. Standardization and Templating
Variation is the enemy of efficiency. Organizations should strive to standardize their credentialing requirements and documentation as much as possible, creating clear templates and checklists for different professional categories. This standardization makes the process more predictable for all parties and eliminates unnecessary confusion about expectations.
Effective standardization might include:
- Uniform application packets with clear instructions
- Standardized verification procedures and requirements
- Consistent approval pathways and decision criteria
- Templated communication for common scenarios
The goal isn’t rigid conformity but rather the elimination of unnecessary variation that adds complication without adding value.
3. Digital Transformation
While digitization alone isn’t sufficient, it’s certainly necessary.
Modern credentialing solutions offer functionality that paper-based processes simply cannot match:
- Online Applications: Self-service portals allow professionals to submit information and documentation electronically, often with guided workflows that ensure completeness.
- Document Management: Digital storage eliminates physical filing requirements and enables instant access to credentials from any location.
- Workflow Automation: Rules-based routing can move applications through appropriate approval channels without manual intervention.
- Integration Capabilities: API connections with primary source verification databases can automatically validate licenses, certifications, and educational credentials.
- Notification Systems: Automated alerts can notify staff and applicants about pending deadlines, missing information, or completed verifications.
The most effective digital transformations don’t simply replicate paper processes electronically – they reimagine the workflow to take advantage of digital capabilities.
4. Data-Driven Decision Making
Optimized credentialing workflows generate valuable data that can inform continuous improvement efforts:
- Processing Metrics: Tracking time-to-credential, bottleneck frequency, and application completeness rates provides insight into process effectiveness.
- Predictive Analytics: Historical data can help forecast credentialing workloads, allowing organizations to allocate resources proactively.
- Quality Indicators: Monitoring error rates, exception frequencies, and rework requirements helps identify areas for process refinement.
- Satisfaction Measures: Feedback from both credentialing staff and applicants provides qualitative insight that complements quantitative metrics.
Organizations should establish key performance indicators (KPIs) for their credentialing function and regularly review these metrics to guide optimization efforts.
5. Staff Training and Empowerment
Technology alone can’t optimize credentialing, people remain central to the process.
Organizations should invest in:
- Skill Development: Ensuring staff understand not just how to execute processes but why specific requirements exist and how to troubleshoot common issues.
- Decision Authority: Empowering credentialing specialists to make appropriate decisions without unnecessary escalations.
- Continuous Learning: Creating mechanisms for staff to share best practices and collaborate on process improvements.
- Change Management: Providing support during transition periods as new workflows and technologies are implemented.
Thriving organizations view their credentialing staff not as paper processors but as skilled professionals who add significant value through their expertise and judgment.
Advanced Optimization Strategies
Once the fundamentals are in place, organizations can explore more sophisticated approaches to credentialing workflow optimization:
 Parallel Processing
Parallel Processing
Traditional credentialing often follows a linear path, with each step waiting for the previous one to complete. Advanced approaches implement parallel processing, allowing multiple verification activities to occur simultaneously. For example, while education verification is underway, the same application might be going through reference checks or licensing validation in parallel.
Parallel processing can dramatically reduce overall credentialing timeframes. However, it requires careful coordination and clear visibility into which elements of the process are active at any given time.
Continuous Verification Models
Rather than treating credentialing as a point-in-time activity, forward-thinking organizations are moving toward continuous verification models. These approaches establish ongoing monitoring of credentials, with automated alerts when licenses expire, disciplinary actions occur, or new requirements emerge.
Continuous verification shifts the paradigm from periodic re-credentialing to exception-based management, focusing attention only on credentials that require intervention.
Centralized Service Centers
Larger organizations with multiple locations or divisions can benefit from centralized credentialing service centers that standardize processes, leverage specialized expertise, and achieve economies of scale.
These centers typically feature:
- Specialized staff who focus exclusively on credentialing
- Standardized workflows across the organization
- Consistent application of policies and requirements
- Shared technology platforms and resources
Centralization can be particularly effective for handling routine credentialing activities, while still allowing for appropriate customization to accommodate local requirements.
Delegated Credentialing
In some industries, organizations can establish delegated credentialing arrangements, where a trusted partner (often a larger entity with robust processes) performs credentialing activities that are then accepted by other organizations. This approach can significantly reduce duplication of effort and accelerate credentialing timeframes.
Healthcare organizations, for example, often participate in delegated credentialing networks where a health plan accepts the credentialing determinations of participating hospitals or medical groups, eliminating the need for providers to undergo multiple credentialing processes.
Blockchain and Distributed Verification
Emerging technologies offer new possibilities for credentialing optimization. Blockchain-based credential verification systems create tamper-proof records of professional qualifications that can be securely shared across organizations.
These systems enable:
- Self-sovereign credentials that professionals can control and share
- Immutable verification records that eliminate redundant checking
- Timestamped credential histories that show the full lifecycle of qualifications
- Reduced reliance on intermediaries for verification
While still developing, these technologies hold significant promise for transforming how credentials are verified and shared across organizational boundaries.
Implementation Considerations
Optimizing credentialing workflows requires careful planning and execution.
Organizations should consider the following implementation factors:
 Stakeholder Engagement
Stakeholder Engagement
Effective optimization requires buy-in from multiple stakeholders:
- Credentialing staff who will execute the new processes
- Department leaders whose teams will be affected by credentialing changes
- Technology partners who will support system implementations
- Compliance and legal teams who ensure regulatory requirements are met
- Executives who must approve resources for optimization initiatives
Early and ongoing engagement with these stakeholders increases the likelihood of successful implementation and sustainable change.
Phased Approach
Attempting to transform all aspects of credentialing simultaneously often leads to disruption and resistance.
A phased approach allows organizations to:
- Test concepts on a smaller scale before full implementation
- Build confidence through early wins
- Refine approaches based on initial results
- Manage change more effectively
- Distribute investment over time
A common phased approach might begin with standardization efforts, followed by technology implementation, process redesign, and finally advanced optimization strategies.
Technology Selection
For many organizations, selecting the right credentialing technology is a critical decision.
Key considerations include:
- Integration capabilities with existing systems
- Configurability to accommodate unique requirements
- User experience for both staff and applicants
- Mobile accessibility for on-the-go professionals
- Reporting and analytics functionality
- Security features and compliance certifications
- Vendor stability and support offerings
Organizations should develop clear requirements before evaluating technology options and involve end users in the selection process to ensure the chosen solution meets their needs.
Change Management
Perhaps the most overlooked aspect of credentialing optimization is change management. Even the best-designed processes and technologies will fail if people don’t adopt them.
Effective change management includes:
- Clear communication about why changes are necessary
- Transparency about how new processes will work
- Adequate training and support during transition periods
- Recognition of the challenges associated with change
- Celebration of successes and milestones
- Mechanisms for feedback and continuous improvement
Organizations that invest in change management typically see faster adoption of new approaches and greater return on their optimization investments.
Measuring Success
How do you know if your credentialing optimization efforts are working?
Extensive measurement includes both efficiency and effectiveness metrics:
Efficiency Metrics
- Average time to credential completion
- Staff hours per credential processed
- Cost per credentialing event
- Automation rate (percentage of steps requiring no manual intervention)
- First-pass yield (applications processed without rework)
Effectiveness Metrics
- Compliance rate with regulatory requirements
- Error detection and correction rates
- Professional satisfaction scores
- Staff satisfaction and retention
- Credentialing-related service delays or issues
Organizations should establish baseline measurements before optimization begins and track progress against these baselines over time.
Looking Ahead: The Future of Credentialing Workflows
As we look to the future, several trends are likely to shape credentialing workflow optimization:
- AI and Machine Learning: Intelligent systems will increasingly assist with document verification, anomaly detection, and predictive alerts.
- Interoperability Standards: Emerging standards will facilitate more seamless sharing of credential information across organizations and systems.
- Biometric Verification: Advanced identity verification technologies will strengthen the connection between credentials and the individuals who hold them.
- Skills-Based Credentialing: Traditional degree-based qualifications will increasingly be supplemented or replaced by more granular skills verification.
- Global Credential Portability: International standards and verification networks will facilitate professional mobility across geographic boundaries.
Organizations that stay attuned to these trends and incorporate emerging best practices will maintain their competitive advantage in credentialing efficiency.
Summary: Credentialing Workflow Optimization, Streamlining the Path to Professional Validation
Credentialing workflow optimization represents a significant and transformative opportunity for organizations across diverse industries to fundamentally improve operational efficiency, strengthen regulatory compliance frameworks, and create substantially better experiences for the professionals they serve. This transformation enables organizations to reduce processing times, minimize errors, enhance data accuracy, and ultimately convert what was once considered an administrative burden into a genuine strategic advantage that drives business.

The optimization journey requires a systematic and thorough approach that begins with conducting thorough assessments of current processes to identify bottlenecks, redundancies, and inefficiencies. Organizations must then focus on standardizing procedures where appropriate while maintaining necessary flexibility for unique circumstances, implementing robust digital capabilities that leverage modern credentialing technology, and empowering staff members with the right tools, training, and decision-making authority to execute processes effectively.
This foundational work involves mapping existing workflows, documenting current pain points, establishing clear performance metrics, and creating standardized templates and procedures that can be consistently applied across different departments and scenarios. The goal is to create a solid infrastructure that supports both current needs and future growth while ensuring that all stakeholders understand their roles and responsibilities within the optimized framework.
Advanced optimization strategies take the transformation to even higher levels of sophistication and effectiveness through the implementation of parallel processing capabilities that allow multiple credentialing steps to occur simultaneously, continuous verification systems that maintain real-time accuracy of professional credentials, and the integration of emerging technologies such as artificial intelligence, machine learning, and blockchain for enhanced security and efficiency. These cutting-edge approaches enable organizations to achieve unprecedented levels of speed, accuracy, and reliability in their credentialing processes.
Contact us to assist with all of your credentialing workflow needs and/or challenges.


 Parallel Processing
Parallel Processing Stakeholder Engagement
Stakeholder Engagement