In the not-so-distant past, medical credentialing conjured images of harried administrators drowning in seas of paperwork, frantically faxing documents, and playing phone tag with insurance companies. The process was about as exciting as watching paint dry, and often took just as long. Yet, much like how your technologically challenged relative finally learned to use emojis, the world of medical credentialing has undergone a surprising digital glow-up. Today’s credentialing landscape is less “file cabinet labyrinth” and more “space-age efficiency system,” with a dash of blockchain and a sprinkle of artificial intelligence for good measure.
From Paperwork Purgatory to Digital Paradise
 Remember when verifying a doctor’s credentials meant sending what felt like formal requests to medical schools and waiting six months for a response? The traditional credentialing process was notorious for its glacial pace and tree-killing paper consumption. A typical application packet for a single physician could easily reach the thickness of a fantasy novel, without the dragons or plot twists, unfortunately.
Remember when verifying a doctor’s credentials meant sending what felt like formal requests to medical schools and waiting six months for a response? The traditional credentialing process was notorious for its glacial pace and tree-killing paper consumption. A typical application packet for a single physician could easily reach the thickness of a fantasy novel, without the dragons or plot twists, unfortunately.
Commence the digital revolution. What started with basic online applications has evolved into comprehensive credentialing management systems that make the old ways look positively medieval. Cloud-based platforms now allow providers to upload documents once and share them across multiple facilities and payers. It’s like the medical equivalent of updating your relationship status on social media, tell one platform, and suddenly everyone knows.
Industry reports indicate that credentialing specialists previously spent upwards of 70% of their work week just processing paperwork. Modern digital systems have cut processing time by more than half, allowing staff to focus on more complex tasks and maintain better work-life balance. Many institutions report that administrative staff can now complete their workday within standard business hours rather than staying late to process credentialing documents.
Blockchain: Not Just for Crypto Bros Anymore
If you thought blockchain was exclusively the domain of tech enthusiasts trying to explain why their digital money isn’t imaginary, think again. Blockchain technology has made its way into medical credentialing, bringing with it the promise of immutable record-keeping and enhanced security.
The concept is surprisingly straightforward: once a credential is verified and added to the blockchain, it becomes a permanent, tamper-proof record that can be accessed by authorized parties across different healthcare systems. No more contacting prestigious medical schools to verify that physicians really did graduate in the year listed on their application.
Several startups have leaped into this space, creating blockchain platforms specifically designed for healthcare credentialing. Companies in this niche are pioneering solutions that could reduce credentialing times from months to days.
Within healthcare technology circles, blockchain in credentialing is often described as having a security guard for medical credentials. Once the information is on the blockchain, it’s verified and nobody can question its authenticity. This builds trust across the healthcare ecosystem and streamlines verification processes.
Of course, blockchain implementation isn’t without its challenges. The technology requires significant buy-in from multiple stakeholders, and explaining blockchain to hospital administrators who may not be technologically savvy presents its own set of obstacles. The potential benefits: reduced fraud, faster verification, and seamless portability of credentials across institutions, make it a trend worth watching.
AI: The Credentialing Robot That (Probably) Won’t Take Over the World
Artificial intelligence has infiltrated nearly every aspect of healthcare, and credentialing is no exception. But before you envision a Terminator-style robot stamping “APPROVED” on medical licenses, understand that AI in credentialing is more subtle and much more helpful.

Today’s AI systems excel at tasks that once consumed human hours: checking for missing information in applications, verifying the status of licenses across multiple databases, flagging discrepancies for human review, and even predicting when renewals will be needed. Some systems can analyze patterns in credentialing data to identify potential red flags that might warrant further investigation.
According to healthcare technology surveys, AI assistants can process basic verifications in minutes that used to take teams days to complete. And unlike human workers, these systems can function 24/7 without breaks, vacations, or benefit packages.
AI has proven particularly valuable for primary source verification, the process of confirming credentials directly with the issuing organizations. Machine learning algorithms can navigate the wildly different formats and requirements of hundreds of medical schools, licensing boards, and certification bodies, extracting the necessary information without human intervention.
One unexpected benefit? Reduced bias in the credentialing process. When properly designed, AI systems evaluate credentials based solely on objective criteria, potentially eliminating unconscious biases that might affect human reviewers.
Telehealth’s Credentialing Conundrum
The pandemic-fueled telehealth boom created a credentialing crisis that nobody saw coming. Suddenly, providers needed to be credentialed across multiple states to treat patients remotely, and traditional state-by-state processes simply couldn’t keep up with demand.
This challenge spawned creative solutions, including the expansion of the Interstate Medical Licensure Compact (IMLC), which streamlines multistate licensing for physicians. As of 2024, over 40 states participate in the compact, allowing qualified physicians to practice across state lines without navigating separate credentialing processes for each jurisdiction.
Healthcare providers report that before compacts like the IMLC, expanding telehealth practice to another state was comparable to starting a completely new job. With these interstate agreements, the process has become more streamlined, still requiring some administrative work, but significantly reducing the bureaucratic burden.
Telehealth companies have also developed specialized credentialing services designed specifically for virtual providers. These services handle the complexity of multi-state requirements, ensuring that telehealth physicians remain compliant while practicing across geographic boundaries.
Some forward-thinking telehealth platforms have even created their own credentialing databases, verifying providers once and then maintaining their eligibility across all states where the platform operates. It’s a bit like having a universal passport for medical practice. Though unfortunately, it doesn’t come with those cool passport stamps.
Credentialing-as-a-Service (CaaS): Yes, That’s Actually a Thing
In the start-up world, adding “-as-a-Service” to anything instantly makes it sound innovative. Surprisingly, when applied to credentialing, the concept actually delivers on its promise. Credentialing-as-a-Service (CaaS) providers offer complete outsourcing of the credentialing process, handling everything from application submission to payer enrollment.
These specialized services combine technology platforms with human expertise, offering healthcare organizations a way to offload the entire credentialing burden. For small practices and rural hospitals with limited administrative resources, CaaS can be a game-changer.
Healthcare administrators report that switching to CaaS providers can eliminate credentialing backlogs within months. New specialists can be fully credentialed with all major payers within six weeks of contract signing, a dramatic improvement over traditional timelines that often stretched beyond a year.
The CaaS market has exploded in recent years, with providers ranging from healthcare-focused tech startups to established medical service companies adding credentialing to their offerings. Many boast success rates of over 95% for first-time applications and average turnaround times under 60 days. A dramatic improvement over traditional in-house processing.
Continuous Monitoring: Because Credentials Can Change
Traditional credentialing was a point-in-time verification—once approved, providers weren’t typically re-evaluated until their renewal date, often two or three years later. That’s a lot of time for things to change, from license suspensions to malpractice claims.
Modern credentialing systems increasingly incorporate continuous monitoring, automatically checking provider credentials against primary sources at regular intervals. If a license expires, a board takes disciplinary action, or another significant event occurs, the system alerts the appropriate administrators immediately.
This approach supports patient safety while reducing institutional risk. Rather than discovering a problem during a routine renewal or, worse, after a patient complaint, organizations can address issues proactively. It’s like having a security system for your provider network—constant vigilance without the paranoia.
Many hospitals have implemented “exception-based” monitoring, where administrators only receive alerts when something requires attention. This approach prevents alert fatigue while ensuring that legitimate concerns receive prompt review.
The Rise of Digital Credentials
Physical certificates and wallet cards are going the way of the dinosaur as more certifying bodies move to digital credentials. These secure digital versions of traditional credentials can be verified instantly online and often include QR codes that patients or administrators can scan to confirm authenticity.
Digital credentials typically include tamper-evident features that make them more secure than their paper counterparts. If someone attempts to alter the information, the verification will fail, preventing credential fraud.
Medical boards, specialty certifications, and even medical schools are increasingly issuing digital credentials that can be directly incorporated into credentialing systems. This eliminates the need for providers to maintain physical copies or request duplicates when originals are lost.
The convenience extends to patients as well. Many healthcare facilities now display digital credential verification on their websites, allowing patients to confirm their provider’s qualifications with a simple click. Transparency builds trust, and digital credentials make that transparency possible at scale.
Standardization: The Boring Revolution We Needed
Perhaps the least flashy but most impactful trend in medical credentialing is the movement toward standardization. Organizations like CAQH (Council for Affordable Quality Healthcare) have developed standard application forms and data sets that eliminate the need for providers to complete unique applications for each hospital or payer.
The CAQH ProView system, for example, allows providers to enter their information once and share it with multiple organizations. Over 1.4 million providers and more than 1,000 participating organizations now use this system, drastically reducing duplicate effort.
Standardization extends beyond forms to the credentialing process itself. The National Committee for Quality Assurance (NCQA) has established Credentialing Verification Organization (CVO) certification, creating consistent quality standards for how credentials are verified. This standardization has made delegated credentialing more reliable and trustworthy.
Industry data suggests that standardized credentialing processes can reduce administrative costs by up to 80% compared to traditional methods. When every organization uses the same format and accepts the same verification standards, everyone wins, except maybe the makers of filing cabinets.
Looking Ahead: The Future of Credentialing
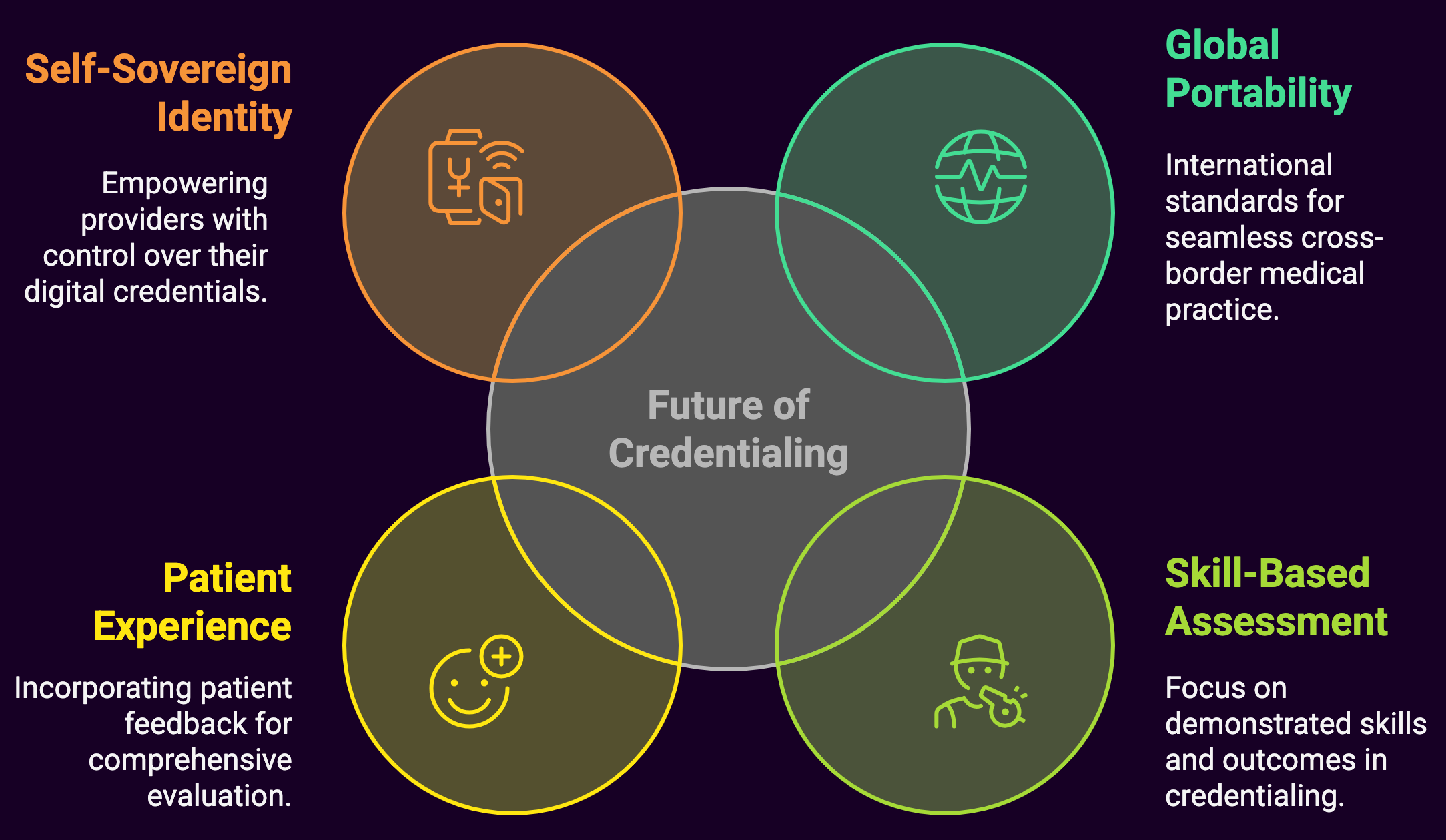
As we look toward the horizon, several emerging trends promise to further transform medical credentialing:
Global Credential Portability
With healthcare becoming increasingly global, efforts are underway to create international standards for credential verification and recognition. This could eventually allow physicians to practice across national boundaries with minimal administrative barriers.
Skill-Based Credentialing
Traditional credentialing focuses heavily on education and training rather than demonstrated skills and outcomes. Some organizations are beginning to incorporate skill assessments and outcome measures into their credentialing processes, particularly for procedural specialties.
Patient Experience Integration
Future credentialing systems may incorporate patient feedback and experience data alongside traditional credentials. While controversial, proponents argue that patient experience provides valuable insight into a provider’s communication skills and bedside manner. Factors that impact care quality, but aren’t reflected in board certifications.
Self-Sovereign Identity
The concept of self-sovereign identity, where individuals own and control their digital credentials, could revolutionize healthcare credentialing. Providers would maintain their own verified credential wallet, granting temporary access to organizations as needed rather than repeatedly submitting the same information.
Summary: The End of the Paper Chase
The transformation of medical credentialing from a paper-intensive bureaucratic nightmare to a streamlined digital process represents more than just technological progress. It’s a fundamental shift in how we establish trust in healthcare credentials.
Patients benefit from increased safety and faster access to care, as verification becomes faster and more reliable. Providers spend less time on administrative hurdles and more time treating patients. Healthcare organizations reduce costs while improving compliance and risk management.
The credentialing revolution may not make headlines like the latest medical breakthrough, but its impact on healthcare efficiency and accessibility is profound. Eliminating unnecessary delays and reducing administrative burden allows modern credentialing processes to ensure that the right providers can deliver care to the right patients at the right time, and that’s nothing to sneeze at, even if you’re fully credentialed to treat sneezing.

