You’ve seen it before; you’re reviewing a provider application and something just doesn’t seem right. Maybe it’s an unexplained gap in work history, a malpractice case that wasn’t disclosed, or inconsistent information across different sections of the application. Your instincts are telling you to dig deeper, but how do you approach these red flags in a systematic way that’s both thorough and fair to the applicant?
 Provider credentialing isn’t just about checking boxes. It’s about protecting patient safety while also ensuring qualified providers can practice effectively. When red flags appear during the application process, credentialing specialists need a structured approach to evaluate and manage these concerns.
Provider credentialing isn’t just about checking boxes. It’s about protecting patient safety while also ensuring qualified providers can practice effectively. When red flags appear during the application process, credentialing specialists need a structured approach to evaluate and manage these concerns.
The below content is a risk-based framework for handling red flags in provider applications. We’ll look at how to identify different types of concerns, assess their severity, investigate appropriately, and make well-documented decisions. Most importantly, we’ll discuss how to do this while maintaining compliance with accreditation standards and regulatory requirements.
Understanding Red Flags: More Than Just Gut Instinct
While experienced credentialers often develop a “sixth sense” for problematic applications, relying purely on instinct isn’t enough. We need clear definitions and categories of red flags to ensure consistent evaluation across all applications.
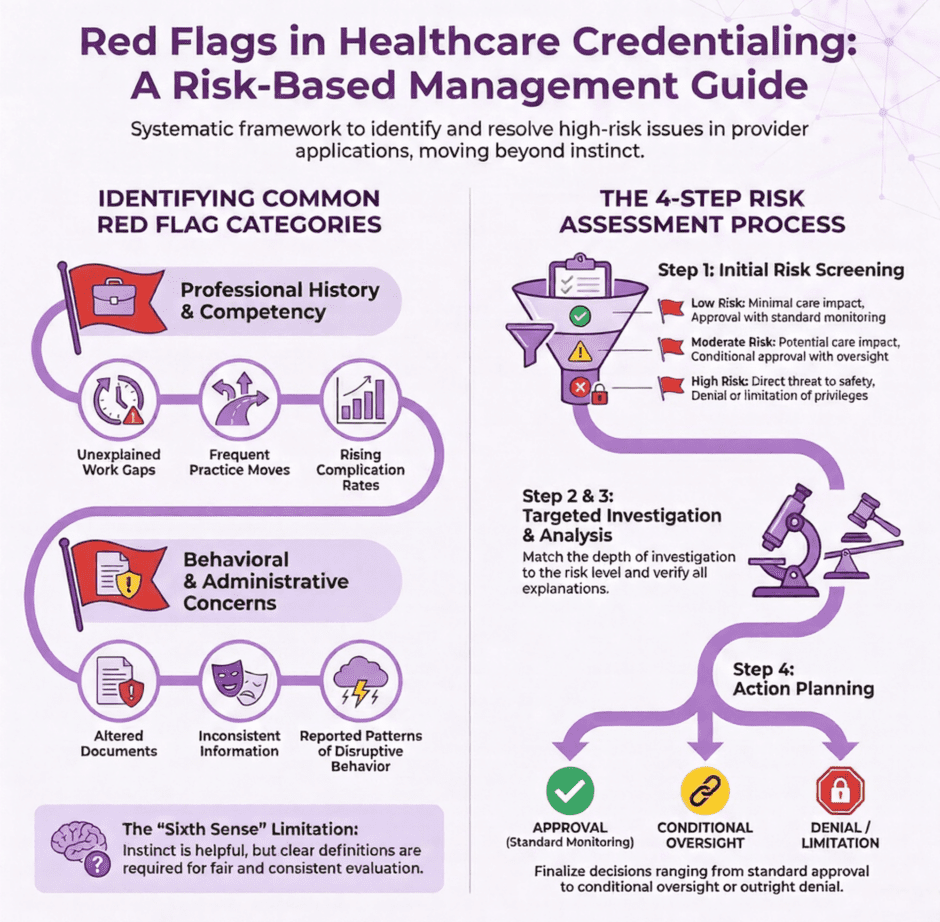
Common categories of red flags include:
Application Completeness and Accuracy Issues
- Missing or incomplete information
- Inconsistencies between different sections or sources
- Altered or potentially falsified documents
- Pattern of incomplete or late responses to information requests
Clinical Competency Concerns
- Unexplained gaps in clinical activity
- Limited or declining case volumes
- Higher than expected complication rates
- Pattern of adverse outcomes
- Negative peer references or concerning feedback
Professional History Red Flags
- Frequent moves between practices or facilities
- Unexplained gaps in work history
- Multiple malpractice cases or unusual settlement patterns
- Licensing board actions or investigations
- Criminal history or sanctions
Behavioral and Professionalism Issues
- Disruptive behavior reports
- Poor communication with staff or patients
- Non-compliance with policies and procedures
- Resistance to quality improvement initiatives
- Substance abuse concerns
The Risk-Based Assessment Framework
Rather than treating all red flags equally, a risk-based approach helps focus resources where they’re needed most.
This framework involves four key steps:
1. Initial Risk Screening
When a red flag is identified, the first step is to assess its potential risk level.
Consider:
- Severity: What’s the potential impact on patient safety?
- Pattern: Is this an isolated incident or part of a concerning pattern?
- Recency: When did the issues occur and are they ongoing?
- Relevance: How directly does this relate to clinical competence and patient care?
Based on these factors, categorize the risk level as:
Low Risk
- Technical or administrative issues
- Isolated incidents with clear resolution
- Older issues with evidence of improvement
- Minimal potential impact on patient care
Moderate Risk
- Clinical performance issues requiring monitoring
- Multiple minor incidents forming a pattern
- Recent but resolving concerns
- Potential for impact on patient care
High Risk
- Serious patient safety concerns
- Active investigations or sanctions
- Pattern of significant issues
- Direct threat to quality of care
2. Investigation and Documentation
The depth and scope of investigation should match the risk level.
Here’s how to approach each category:
Low Risk Investigations
- Request clarification or missing information
- Verify explanations with primary sources
- Document findings in credentialing file
- May proceed with normal processing if resolved
Moderate Risk Investigations
- Detailed review of all related documentation
- Direct communication with previous institutions
- Focused professional reference checks
- Consider peer review committee input
- Develop monitoring plan if approved
High Risk Investigations
- Extensive background investigation
- Multiple reference checks including peers
- Review of all available quality data
- Legal counsel consultation as needed
- Full credentials committee review
3. Analysis and Decision-Making
Once the investigation is complete, analyze the findings using these key questions:
- Is there a satisfactory explanation for the red flags?
- Has the applicant been forthcoming and cooperative?
- What evidence exists of rehabilitation or improvement?
- Are there appropriate safeguards available?
- How does this align with organizational risk tolerance?
Document your analysis clearly, including:
- Summary of findings
- Risk mitigation options considered
- Rationale for recommendations
- Supporting evidence and references
4. Action Planning and Follow-up
Based on the analysis, develop an appropriate action plan:
Approval with Standard Terms
- For resolved low-risk issues
- Normal monitoring and renewal cycle
- Document resolution in file
Conditional Approval
- For moderate risk situations
- Specific monitoring requirements
- Focused quality review
- Time-limited privileges
- Required improvement activities
Denial or Limitation
- For unresolved high-risk issues
- Clear documentation of reasons
- Fair hearing rights if applicable
- Reporting requirements if needed
Special Considerations and Best Practices
Maintaining Objectivity
It’s crucial to maintain objectivity throughout the process. Some tips:
- Use standardized assessment tools
- Get multiple perspectives on complex cases
- Document evidence rather than impressions
- Focus on patterns rather than isolated events
- Consider context and circumstances
- Avoid assumptions about intent
Legal and Regulatory Compliance
Remember to consider:
- State licensing requirements
- Federal reporting obligations
- Fair hearing and due process rights
- Discrimination concerns
- Documentation requirements
- Privacy and confidentiality rules
Communication Strategies
Effective communication is essential when managing red flags:
With Applicants:
- Be clear about concerns and requirements
- Maintain professional, non-accusatory tone
- Document all communications
- Set clear expectations and deadlines
- Provide opportunities for explanation
With Committees:
- Present objective findings
- Include relevant context
- Outline options considered
- Make clear recommendations
- Document discussions and decisions
Common Pitfalls to Avoid
Don’t fall into these common traps:
- Rushing to judgment without full investigation
- Failing to document reasoning and evidence
- Inconsistent handling of similar situations
- Ignoring patterns of minor issues
- Over-relying on explanations without verification
- Missing reporting requirements
- Failing to follow up on monitoring plans
Implementing a Risk-Based Framework
To successfully implement this approach in your organization:
1. Develop Clear Policies
Create written policies that:
- Define categories of red flags
- Establish investigation procedures
- Set decision-making criteria
- Specify documentation requirements
- Outline monitoring processes
- Address fair hearing rights
2. Train Your Team
Provide complete training on:
- Red flag identification
- Investigation techniques
- Documentation requirements
- Communication strategies
- Legal/regulatory requirements
- Decision-making processes
3. Create Supporting Tools
Develop standardized tools like:
- Risk assessment matrices
- Investigation checklists
- Documentation templates
- Monitoring plans
- Communication scripts
- Quality metrics
4. Establish Review Processes
Implement regular reviews of:
- Risk assessment accuracy
- Investigation quality
- Decision consistency
- Monitoring effectiveness
- Documentation completeness
- Outcome measures
Special Scenarios and Case Studies
Let’s look at some common scenarios and how to handle them:
Scenario 1: The Moving Provider
A surgeon applies with a history of practicing at five facilities in three years.
Red Flags:
- Frequent moves
- Incomplete work history
- Vague references
Investigation:
- Detailed employment verification
- Focused reference checks
- Review of case logs
- Peer references from each facility
Potential Outcomes:
- Approval with monitoring if moves explained
- Conditional approval with oversight
- Denial if pattern concerning
Scenario 2: The Aging Provider
An experienced provider shows declining clinical activity and increasing complications.
Red Flags:
- Rising complication rates
- Decreasing volume
- Peer concerns
Investigation:
- Focused professional evaluation
- Cognitive assessment if indicated
- Detailed case review
- Peer references
Potential Outcomes:
- Modified privileges
- Required proctoring
- Focused monitoring
- Voluntary retirement plan
Scenario 3: The Disruptive Provider
A highly skilled provider has multiple behavioral complaints.
Red Flags:
- Staff complaints
- Patient grievances
- Policy violations
Investigation:
- Detailed incident review
- Staff interviews
- Behavioral evaluation
- Performance data review
Potential Outcomes:
- Behavioral contract
- Required coaching
- Conditional privileges
- Progressive discipline
Building a Culture of Safety and Quality
Managing red flags isn’t just about individual cases; it’s about creating a culture of safety and quality.
This includes:
Continuous Improvement
- Regular policy review and updates
- Team training and development
- Process refinement
- Outcome tracking
- Best practice sharing
Transparent Communication
- Clear expectations
- Regular updates
- Open dialogue
- Feedback loops
- Shared learning
Supportive Environment
- Focus on improvement
- Fair evaluation
- Professional development
- Peer support
- Resource availability
Looking to the Future
The field of provider credentialing continues to develop.
Stay ahead by:
Embracing Technology
- Digital verification tools
- Automated monitoring
- Data analytics
- Risk prediction models
- Integration capabilities
Enhancing Processes
- Streamlined workflows
- Real-time monitoring
- Proactive intervention
- Continuous assessment
- Quality metrics
Building Partnerships
- Professional organizations
- Technology vendors
- Legal resources
- Educational institutions
- Quality organizations
Summary: Managing Red Flags in Credentialing Apps
Managing red flags in provider applications requires a balanced approach that protects patient safety while treating providers fairly.
By implementing a risk-based credentialing framework, organizations can:
- Identify concerns early
- Investigate appropriately
- Make consistent decisions
- Document effectively
- Monitor outcomes
- Improve continuously
The goal isn’t just to screen out problems; it’s to support provider success while ensuring safe, high-quality patient care. With clear processes, proper training, and consistent application, healthcare organizations can effectively manage red flags while maintaining a positive professional environment.

