Modifiers can make or break your practice’s revenue cycle. Among all the modifiers in the CPT coding system, Modifier 59 stands out as one of the most important and most frequently misused.
This two-digit code can mean the difference between getting paid for the services you provide and watching claims get denied or downcoded.
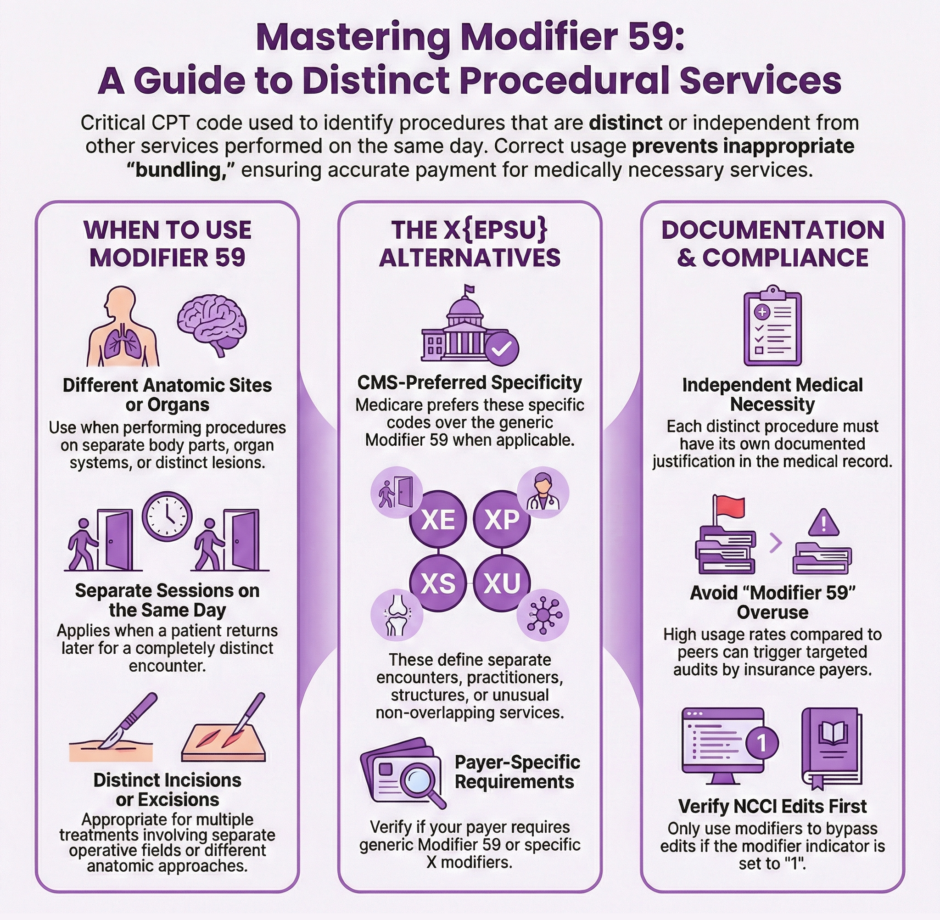
Modifier 59 tells payers that a procedure or service was distinct or independent from other services performed on the same day. It’s your way of saying “yes, we did these procedures on the same day, but they were separate and both medically necessary.” Without proper use of this modifier, payers will often bundle procedures together and pay you for only one service when you actually performed two or more.
The challenge is that Modifier 59 gets scrutinized heavily by insurance companies and auditors. Use it incorrectly, and you’re looking at claim denials, payment clawbacks, or even allegations of improper billing. Use it correctly, and you’re capturing legitimate revenue for the work you’re actually doing.
Below, everything you need to know about Modifier 59. When to use it, when not to use it, and how to document properly to support your coding decisions.
What Modifier 59 Actually Means
Modifier 59 is officially defined as “Distinct Procedural Service.” According to CPT guidelines, it identifies procedures that are not normally reported together but are appropriate under certain circumstances. The modifier indicates that a procedure or service was independent, separate, or distinct from other services performed on the same day.
The key word here is “distinct.” You’re telling the payer that even though these procedures might typically be bundled together or considered part of the same service, in this specific case they were separate and distinct procedures that both deserve separate payment.
CMS and other payers have specific criteria for when services are considered distinct. The procedure must meet one of these conditions: it was performed during a different session or patient encounter, it was performed on a different site or organ system, it involved a separate incision or excision, it addressed a separate injury or area of injury, or it was a procedure that’s not ordinarily encountered or performed on the same day but is appropriate under the circumstances.
Here’s what Modifier 59 is not. It’s not a way to get around legitimate bundling edits. It’s not a tool for unbundling procedures that should be reported together. It’s not something you add to every claim just to see if you can get extra payment. Improper use of Modifier 59 is considered a compliance issue and can trigger audits.
When to Use Modifier 59
Knowing when to apply Modifier 59 requires solid knowledge of both coding guidelines and the specific clinical circumstances of each case. Here are the situations where Modifier 59 is typically appropriate.
- Different Anatomic Sites: When you perform the same or similar procedures on different anatomic locations during the same session, Modifier 59 may be appropriate. For example, excising a lesion from the patient’s arm and another lesion from their leg during the same visit would warrant Modifier 59 on one of the procedures.
- Different Sessions on the Same Day: If a patient comes in for one procedure in the morning and returns later that day for a completely separate procedure, Modifier 59 indicates these were distinct encounters even though they occurred on the same calendar date.
- Different Procedures on Different Organs: Performing procedures on different organ systems or different areas that aren’t typically done together may require Modifier 59. For instance, a colonoscopy and an upper endoscopy performed during the same surgical session would need this modifier.
- Separate Injuries or Lesions: When treating multiple distinct injuries or addressing multiple separate lesions during one encounter, Modifier 59 tells the payer that each required individual attention and treatment.
The documentation in your medical record must clearly support the use of Modifier 59. You can’t just add the modifier and hope for the best. The clinical notes need to show exactly why the procedures were distinct, what made them separate, and why both were medically necessary.
The X{EPSU} Modifiers: More Specific Alternatives
CMS introduced a more specific set of modifiers to replace Modifier 59 in certain situations. These are called the X{EPSU} modifiers, and they provide more detailed information about why services were distinct. Many payers now prefer these more specific modifier codes over the generic Modifier 59.
The four X modifiers are:
- XE (Separate Encounter): Used when services were performed during separate encounters on the same day. This might apply when a patient is seen in the office in the morning and then returns to the emergency department that evening for an unrelated issue.
- XP (Separate Practitioner): Used when different practitioners perform distinct services on the same patient during the same day. This often comes up in hospital settings where multiple specialists are involved in a patient’s care.
- XS (Separate Structure): Applied when procedures are performed on separate organs or separate structures. This modifier works well for bilateral procedures or procedures on anatomically distinct areas.
- XU (Unusual Non-Overlapping Service): Reserved for situations where the use of a modifier is appropriate but none of the other X modifiers accurately describe the circumstance. This is essentially a more specific version of Modifier 59 for unusual cases.
CMS prefers these X modifiers because they provide more specific information about why procedures should be paid separately. Many Medicare Administrative Contractors (MACs) and other payers now require the X modifiers instead of Modifier 59 when applicable. However, some commercial payers still don’t recognize the X modifiers and require Modifier 59.
This creates a documentation challenge for practices. You need to know which payers accept which modifiers and code accordingly. Your billing system should be able to track payer preferences and apply the correct modifier based on the insurance company processing the claim.
Common Modifier 59 Mistakes to Avoid
Billing staff make several predictable errors with Modifier 59, and these mistakes lead to denied claims or compliance problems. Being aware of these common pitfalls helps you avoid them.
- Using Modifier 59 as a First Resort: The CPT guidelines are clear that Modifier 59 should only be used when no other modifier more appropriately describes the relationship between the procedures. If another modifier like 76 (repeat procedure), 77 (repeat procedure by another physician), or 78 (return to operating room) applies, use that modifier instead.
- Applying Modifier 59 to Procedures with Designated Modifiers: Some procedures have specific anatomic modifiers (like LT for left side, RT for right side, or finger/toe designators). When these anatomic modifiers appropriately describe the distinction between procedures, you don’t need to add Modifier 59.
- Ignoring NCCI Edits: The National Correct Coding Initiative (NCCI) publishes edits that identify procedure code pairs that shouldn’t typically be billed together. Some of these edits have a modifier indicator of “1,” which means you can use a modifier to bypass the edit if clinically appropriate. Others have a modifier indicator of “0,” meaning the edit cannot be bypassed with any modifier, including Modifier 59.
- Poor or Missing Documentation: Adding Modifier 59 without clear documentation to support it is asking for trouble. Auditors will look at your medical records, and if the documentation doesn’t clearly show why the procedures were distinct, they’ll deny the claim and potentially flag your practice for further review.
- Overusing the Modifier: If your practice is appending Modifier 59 to a high percentage of claims, payers will notice. Frequent use of this modifier without clear medical necessity raises red flags and can trigger targeted audits. Use it only when truly appropriate, not as a routine billing strategy.
Documentation Requirements for Modifier 59
 Your documentation must tell the complete story of why procedures performed on the same day were distinct and separate. Without proper documentation, even appropriate uses of Modifier 59 will get denied upon review.
Your documentation must tell the complete story of why procedures performed on the same day were distinct and separate. Without proper documentation, even appropriate uses of Modifier 59 will get denied upon review.
The medical record should clearly indicate the specific site, organ, or anatomic location for each procedure. If you’re using Modifier 59 based on different anatomic sites, the documentation needs to specify exactly where each procedure was performed. Vague descriptions like “multiple areas” don’t cut it.
Time documentation becomes important when you’re billing separate encounters on the same day. The notes should show what time each encounter occurred and what happened during each one. If there were separate and distinct sessions, your documentation should make that abundantly clear.
The medical necessity for each procedure needs independent documentation. Don’t just document one condition and assume it justifies multiple procedures. Each procedure should have its own medical necessity justification based on the patient’s condition, symptoms, or clinical findings.
For surgical procedures, operative reports should detail separate incisions, separate operative fields, or different anatomic approaches. If you made one incision and performed multiple procedures through that same incision, bundling rules likely apply and Modifier 59 probably isn’t appropriate.
Photos, diagrams, or anatomic drawings can strengthen your documentation for procedures involving different sites. These visual aids make it crystal clear to auditors that you worked on distinct anatomic locations.
Modifier 59 in Different Specialties
Different medical specialties encounter Modifier 59 in specialty-specific contexts. Understanding how the modifier applies in your particular field helps ensure correct usage.
- Dermatology frequently uses Modifier 59 for destruction or excision of multiple lesions in different anatomic locations. When removing skin cancers or treating actinic keratoses in multiple areas during one visit, dermatologists append Modifier 59 to indicate each lesion required separate treatment.
- Orthopedics applies Modifier 59 when performing procedures on different anatomic sites, like injecting one knee and one shoulder during the same visit, or treating separate fractures in different bones. The modifier indicates these weren’t component procedures of a single treatment.
- Gastroenterology uses Modifier 59 for multiple endoscopic procedures performed during the same session but in different areas of the digestive tract. However, many GI procedures have specific bundling rules, so coders need to verify NCCI edits carefully.
- Ophthalmology encounters Modifier 59 when performing procedures on both eyes during the same surgical session, though often the RT/LT modifiers are more appropriate. The modifier also applies when doing procedures on different structures of the eye.
- Radiology applies Modifier 59 when performing imaging studies on different anatomic areas during the same session. However, radiology has specific Multiple Procedure Payment Reduction (MPPR) rules that affect reimbursement regardless of modifier use.
Payer-Specific Rules and Preferences
 Not all insurance companies handle Modifier 59 the same way. Understanding payer-specific rules prevents surprises when claims get processed.
Not all insurance companies handle Modifier 59 the same way. Understanding payer-specific rules prevents surprises when claims get processed.
Medicare and Medicare Advantage plans generally prefer the X{EPSU} modifiers over Modifier 59 when the more specific modifiers apply. However, when none of the X modifiers fit the situation, Modifier 59 remains acceptable for Medicare claims.
Many commercial payers haven’t adopted the X{EPSU} modifiers and will reject claims if you use them. These payers still require Modifier 59. Your billing system needs to recognize which payer is processing the claim and apply the appropriate modifier.
Some payers have specific local coverage determinations (LCDs) or billing articles that provide guidance on Modifier 59 usage for certain procedures. Checking these resources before billing saves time and reduces denials.
Medicaid rules vary by state. Some state Medicaid programs follow Medicare guidelines and accept X modifiers, while others have their own modifier policies. Verify your state’s specific requirements.
Appealing Modifier 59 Denials
Even with appropriate use and strong documentation, Modifier 59 claims sometimes get denied. Knowing how to appeal effectively recovers revenue that’s rightfully yours.
Your appeal should include:
- A clear explanation of why the procedures were distinct and separate
- Copies of the relevant medical record documentation showing different sites, sessions, or circumstances
- References to CPT guidelines supporting your coding decision
- Citations of the specific criteria met for Modifier 59 or X modifier usage
- Any operative reports, procedure notes, or clinical documentation that demonstrates medical necessity
Start with a written appeal to the insurance company’s claims department. Include all supporting documentation and be specific about why the procedures warranted separate payment. Generic appeal letters rarely succeed.
If the first-level appeal is denied, escalate to a higher level of review. Most payers have multiple appeal levels, and persistence often pays off when you have solid documentation.
For repeated denials of appropriate Modifier 59 usage, consider requesting a peer-to-peer review where a physician from your practice can discuss the case directly with the payer’s medical director.
Training Your Staff on Modifier 59
 Everyone involved in your coding and billing process needs proper training on Modifier 59 usage. This includes physicians, advanced practice providers, medical coders, and billing staff.
Everyone involved in your coding and billing process needs proper training on Modifier 59 usage. This includes physicians, advanced practice providers, medical coders, and billing staff.
Providers need to document with enough specificity to support modifier usage. They should indicate anatomic locations clearly, note when procedures occur during separate sessions, and describe why multiple procedures were necessary.
Coders need training on CPT guidelines, NCCI edits, payer-specific rules, and appropriate modifier selection. They should know when Modifier 59 applies, when other modifiers are more appropriate, and when no modifier should be used.
Billing staff should verify modifier usage before claim submission and be prepared to respond to payer questions or denials. They need to know what documentation supports each modifier and how to appeal when appropriate.
Regular audits of Modifier 59 usage help identify patterns of incorrect application before they become major compliance issues. Review a sample of claims with this modifier quarterly to ensure your practice is using it correctly.
Compliance Considerations
The Office of Inspector General (OIG) has specifically identified Modifier 59 as an area of concern in multiple work plans. Improper use can result in overpayments that must be returned, civil monetary penalties, or exclusion from federal healthcare programs in extreme cases.
Practices with unusually high Modifier 59 usage compared to peers may face targeted audits. Payers compare your modifier usage to similar practices in your specialty and geographic area. Significant deviation from the norm raises red flags.
Internal compliance programs should include regular reviews of Modifier 59 claims. Look for patterns like always billing certain code combinations with this modifier, providers who use it much more frequently than their colleagues, or procedures that consistently get denied when the modifier is applied.
Documentation audits should verify that medical records support every instance of Modifier 59 usage. If your documentation wouldn’t convince an external auditor that procedures were distinct, the modifier shouldn’t be there.
How Medwave Handles Modifier 59 Correctly
 At Medwave, we specialize in billing, credentialing, and payer contracting for healthcare practices nationwide. Our expert coding team knows the intricacies of Modifier 59 and the X{EPSU} modifiers inside and out.
At Medwave, we specialize in billing, credentialing, and payer contracting for healthcare practices nationwide. Our expert coding team knows the intricacies of Modifier 59 and the X{EPSU} modifiers inside and out.
We verify NCCI edits before every claim submission, ensuring modifiers are only applied when clinically appropriate and properly documented. Our coders stay current on payer-specific rules, applying Modifier 59 for payers that require it and switching to X modifiers for Medicare and other payers that prefer the more specific alternatives.
When claims with Modifier 59 get denied, our denial management team appeals with strong clinical documentation and clear explanations of why separate payment is warranted. We track denial patterns across payers and procedures, identifying trends that help prevent future denials.
Our compliance monitoring includes regular audits of modifier usage across all our clients. We identify potential issues before they become problems and provide feedback to ensure documentation supports coding decisions.
Contact us today to learn how we can optimize your practice’s revenue cycle while maintaining strict compliance standards.

