Allied health professionals form the backbone of modern healthcare delivery, yet their credentialing needs often get overlooked or mishandled. Physical therapists, occupational therapists, speech-language pathologists, dietitians, respiratory therapists, and dozens of other allied health providers face unique credentialing challenges that differ significantly from physician credentialing. Getting these professionals credentialed correctly and efficiently requires specialized knowledge of their specific requirements, licensing structures, and payer relationships.
At Medwave, we’ve credentialed many thousands of allied health professionals across every specialty. We know that while the basic credentialing process shares similarities with physician credentialing, the details matter enormously. Miss one specialty-specific requirement and your application sits in limbo for months. Use the wrong taxonomy code and claims get denied even though you’re technically credentialed. Fail to maintain specialty certifications and you lose network status without warning.
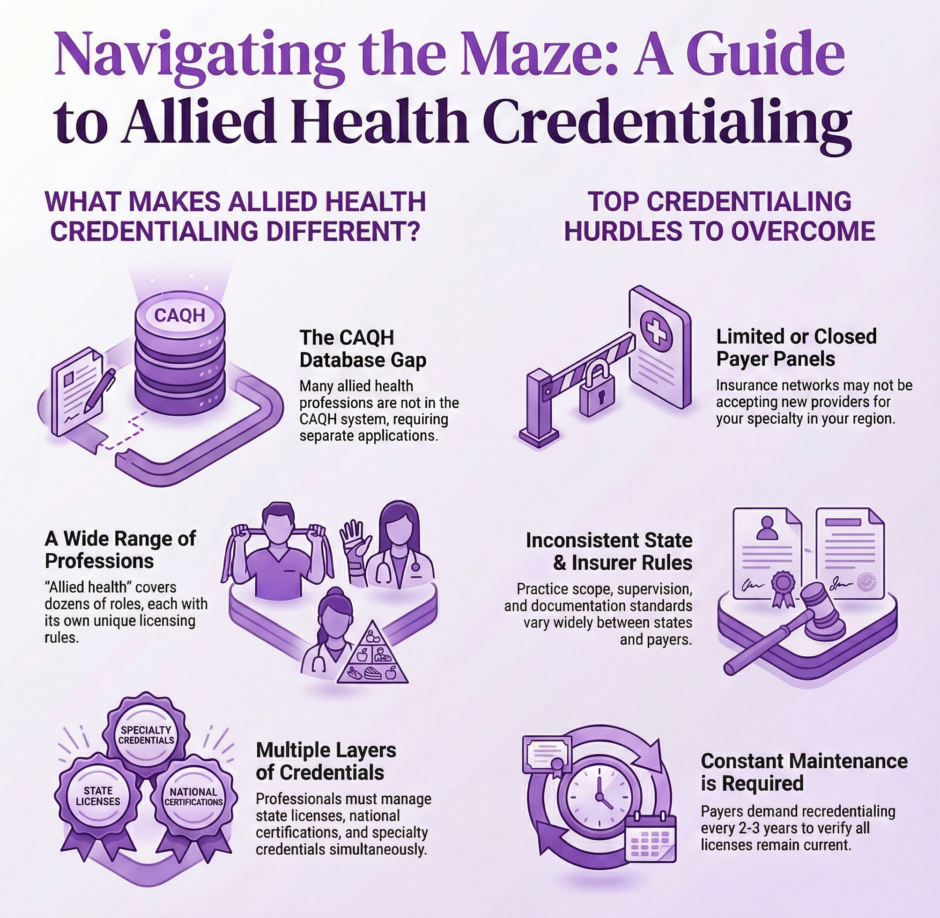
Let’s break down what makes allied health credentialing different and how to approach it correctly.
Who Counts as Allied Health?
 The term “allied health” covers a broad range of healthcare professionals who aren’t physicians, nurses, or dentists. These providers deliver essential clinical services that support patient diagnosis, treatment, and recovery. The category includes dozens of distinct professions, each with its own educational requirements, licensing structures, and scope of practice.
The term “allied health” covers a broad range of healthcare professionals who aren’t physicians, nurses, or dentists. These providers deliver essential clinical services that support patient diagnosis, treatment, and recovery. The category includes dozens of distinct professions, each with its own educational requirements, licensing structures, and scope of practice.
Common allied health professions include physical therapists (PT), occupational therapists (OT), speech-language pathologists (SLP), audiologists, dietitians and nutritionists, respiratory therapists, medical social workers, certified athletic trainers, radiologic technologists, and clinical laboratory scientists. Each profession requires different credentials and faces different payer credentialing requirements.
Some allied health providers work independently in private practice settings. Others work within hospitals, clinics, or larger healthcare organizations. The practice setting affects credentialing requirements, as some payers credential individual allied health professionals while others only credential organizations that employ them.
Education and Licensing Requirements by Profession
Allied health professions have varying educational requirements that impact credentialing. Physical therapists now require a Doctor of Physical Therapy (DPT) degree, though some practicing PTs hold master’s degrees under previous requirements. Occupational therapists typically hold master’s degrees, with some newer practitioners earning occupational therapy doctorates. Speech-language pathologists need master’s degrees in speech-language pathology or communication disorders.
State licensing adds another layer of requirements. Most allied health professions require state licensure to practice, though specific requirements vary by state and profession. Physical therapists must pass the National Physical Therapy Examination (NPTE) and obtain state licensure. Occupational therapists take the National Board for Certification in Occupational Therapy (NBCOT) exam before applying for state licenses. Speech-language pathologists complete a Clinical Fellowship Year (CFY) under supervision before receiving full licensure.
Some professions use certification rather than licensure in certain states. Dietitians may be licensed, certified, or registered depending on the state. Athletic trainers face varying state requirements, with some states requiring licensure while others accept national certification. Knowing which credentials your state requires prevents delays during the credentialing process.
National certifications from professional organizations often complement or precede state licensure. These certifications verify that professionals have met standardized competency requirements across the country. Payers frequently require both state licensure and national certification for credentialing, making both credentials essential.
CAQH and Allied Health Professionals

CAQH (Council for Affordable Quality Healthcare) serves as the primary credentialing database for most commercial insurance companies. However, CAQH primarily focuses on physicians and some advanced practice providers. Many allied health professionals cannot create CAQH profiles because their professions aren’t included in the system.
This limitation creates extra work for allied health credentialing. Without CAQH profiles, each payer requires separate applications with complete documentation. You can’t just direct payers to pull information from CAQH like you would for physicians. Every credentialing application needs full documentation packages submitted individually.
Some larger allied health practices or organizations use credentialing verification organizations (CVOs) that specialize in non-physician providers. These CVOs perform primary source verification and maintain databases that some payers will accept. However, CVO usage is less standardized than CAQH for physician credentialing.
The absence of centralized databases means allied health credentialing requires more direct communication with payers. You’re calling credentialing departments, emailing documents, and following up individually with each insurance company. This takes more time and requires detailed tracking to ensure nothing falls through the cracks.
Payer Panels and Network Limitations
Not all insurance companies credential all types of allied health professionals. Some payers have open panels for physical therapists but closed or limited panels for occupational therapists. Others credential speech-language pathologists readily but rarely accept dietitians into their networks. Knowing which payers actively credential your profession saves time and prevents wasted effort.
Panel limitations vary by geographic region as well. A payer might have open physical therapy panels in urban areas but closed panels in suburban or rural regions where they already have sufficient provider coverage. Regional market saturation affects whether new providers can join networks regardless of their qualifications.
Some insurance companies only credential allied health professionals working within certain organizational structures. They might credential hospital-based therapists but not independent practitioners. Or they’ll credential group practices but not solo providers. These structural requirements affect how you approach credentialing and whether individual credentialing is even possible.
Medicare credentialing for allied health professionals follows different rules than commercial insurance. Physical therapists, occupational therapists, and speech-language pathologists can enroll in Medicare as individual practitioners. Other allied health professionals may need to bill through employing organizations or under physician supervision depending on Medicare’s coverage policies for their services.
Specialty Certifications and Advanced Credentials

Many allied health professions offer specialty certifications beyond basic licensure. Physical therapists can earn board certifications in orthopedics, sports, neurology, pediatrics, and other specialties. Occupational therapists have specialty certifications in hand therapy, low vision, driving rehabilitation, and gerontology. Speech-language pathologists can earn certificates of clinical competence in specific areas.
These specialty certifications can impact credentialing in multiple ways. Some payers offer better reimbursement rates for board-certified specialists. Others require specialty certification to provide certain services or use specific billing codes. Including specialty credentials in your credentialing applications documents your expertise and may expand your network participation options.
Continuing education requirements for maintaining certifications vary by profession and specialty. Physical therapy board certifications require ongoing continuing education specific to the specialty area. Occupational therapy certifications have renewal requirements that include professional development activities. Speech-language pathology maintains continuing education requirements for maintaining the Certificate of Clinical Competence (CCC).
Keeping specialty certifications current is crucial for maintaining credentialing status. Let a certification lapse and some payers will suspend your network participation until you provide proof of renewal. Track certification expiration dates carefully and renew well before deadlines to avoid any interruption in network status.
Documentation Requirements for Allied Health Credentialing
Allied health credentialing applications require extensive documentation similar to physician credentialing but with profession-specific additions. You’ll need copies of professional degrees showing completion of required educational programs. State license documentation for every state where you’ll practice is essential. National certification documents from organizations like NBCOT, NPTE, or ASHA must be current and clearly legible.
Professional liability insurance requires special attention for allied health providers. Coverage amounts vary by profession and payer requirements. Physical therapists typically need $1 million per occurrence and $3 million aggregate coverage. Occupational therapists face similar requirements. Some payers accept lower limits for certain allied health professions, but confirm requirements before purchasing coverage.
Work history documentation needs to cover the past five to ten years depending on payer requirements. This includes all practice locations, employment dates, supervisors, and clinical activities. Gaps in work history require explanation, whether for continuing education, family leave, or other reasons. Unexplained gaps raise questions that delay credentialing.
Professional references from colleagues who can speak to your clinical competence are typically required. Most payers want three to five references from other healthcare professionals familiar with your work. Choose references who will respond promptly to verification requests, as slow reference responses frequently delay credentialing approvals.
Supervision requirements for certain allied health professions add documentation layers. Speech-language pathologists must document completion of their Clinical Fellowship Year under appropriate supervision. Clinical laboratory scientists may need supervision documentation depending on their specialty and state requirements. Athletic trainers working in certain settings need physician supervision agreements documented.
The Primary Source Verification Process
 Insurance companies verify allied health credentials through primary source verification, contacting original issuing organizations directly rather than accepting copies at face value. They contact universities to verify degree completion and graduation dates. They check with state licensing boards to confirm licenses are active and in good standing. They reach out to certification organizations to validate certifications.
Insurance companies verify allied health credentials through primary source verification, contacting original issuing organizations directly rather than accepting copies at face value. They contact universities to verify degree completion and graduation dates. They check with state licensing boards to confirm licenses are active and in good standing. They reach out to certification organizations to validate certifications.
This verification process takes time because each organization has its own response timelines. Universities might take two to three weeks to respond to verification requests. State licensing boards vary from quick online verification to month-long waits for written confirmations. National certification organizations typically respond within a few weeks but can take longer during busy periods.
International credentials require extra verification steps. Allied health professionals trained outside the United States need their degrees evaluated by credential evaluation services. Foreign licenses need validation that they meet U.S. equivalency standards. Some professions have specific requirements for international graduates, like additional testing or supervised practice periods.
Previous malpractice claims require disclosure and explanation during credentialing. Even if claims were dismissed or settled without admitting fault, you must report them. Payers review claims carefully and may request detailed information about circumstances and outcomes. Being transparent about claims and providing thorough explanations prevents more serious issues than the claims themselves.
Common Credentialing Challenges for Allied Health
Allied health professionals face specific credentialing obstacles that physicians don’t typically encounter. Limited payer panels create barriers to network participation that have nothing to do with qualifications. You might be an excellent physical therapist with strong credentials, but if the payer’s PT panel is closed in your area, you’re not getting credentialed regardless of your qualifications.
Varying state practice acts create confusion about scope of practice and licensure requirements. What physical therapists can do independently in one state might require physician supervision in another. These variations affect credentialing requirements and how services get billed. You need to know your state’s specific practice act and document that your practice operates within legal boundaries.
Reimbursement rates for allied health services are often lower than for physician services, making some payers less attractive for participation. A payer might credential you but offer rates so low that accepting their insurance loses money on every patient visit. Evaluate payer rates before investing time in credentialing applications to ensure network participation makes financial sense.
Documentation standards vary widely across payers. Some accept electronically submitted documents while others require original paper documents mailed to specific addresses. Application formats differ, with some payers using online portals and others using paper forms. Tracking what each payer needs and in what format requires detailed organization.
Medicare Enrollment for Allied Health Professionals
 Medicare enrollment follows specific rules for different allied health professions. Physical therapists, occupational therapists, and speech-language pathologists enroll as individual practitioners through PECOS (Provider Enrollment, Chain and Ownership System). They receive their own Provider Transaction Access Numbers (PTANs) and can bill Medicare directly for covered services.
Medicare enrollment follows specific rules for different allied health professions. Physical therapists, occupational therapists, and speech-language pathologists enroll as individual practitioners through PECOS (Provider Enrollment, Chain and Ownership System). They receive their own Provider Transaction Access Numbers (PTANs) and can bill Medicare directly for covered services.
Other allied health professionals may need to enroll differently depending on Medicare coverage policies for their services. Dietitians enrolled in Medicare as registered dietitian nutritionists can provide medical nutrition therapy services. Respiratory therapists typically work for organizations that enroll in Medicare rather than enrolling individually. Clinical social workers can enroll individually if they meet Medicare’s requirements.
Medicare enrollment requires detailed information about practice locations, business structures, and ownership. You’ll need to provide your National Provider Identifier (NPI), tax identification information, and documentation of your professional credentials. The application asks about any past sanctions, exclusions, or program violations.
Processing times for Medicare enrollment typically run 60-90 days for clean applications. Errors or missing information extend this timeline considerably. Medicare has strict deadlines for responding to requests for additional information, and missing these deadlines results in application denials requiring you to start over.
Medicaid Credentialing Variations
State Medicaid programs each have separate enrollment processes for allied health professionals. Some states credential a wide range of allied health providers while others limit which professions can participate. Coverage policies for allied health services vary dramatically from state to state, affecting which professionals Medicaid will even consider credentialing.
Application complexity varies by state. Some states have streamlined online enrollment systems that make the process relatively quick. Others use paper applications that take months to process. A few states outsource Medicaid enrollment to managed care organizations, adding another layer of variation in requirements and timelines.
Payment rates for allied health services through Medicaid are often lower than commercial insurance or Medicare. Some states reimburse physical therapy and occupational therapy at reasonable rates while others pay so little that practices lose money serving Medicaid patients. Research your state’s Medicaid payment schedules before investing time in enrollment.
Maintaining Credentials and Recredentialing
Allied health credentialing isn’t a one-time event. Most payers require recredentialing every two to three years to verify that credentials remain current and no issues have developed. Recredentialing involves updating all your information and going through review processes again.
License renewals need to happen on schedule to prevent credentialing problems. Most states require allied health professionals to renew licenses every one to two years. These renewals include continuing education requirements that vary by profession and state. Track renewal dates carefully and complete continuing education well before deadlines.
Certification renewals from national organizations follow their own schedules. The Certificate of Clinical Competence for speech-language pathologists requires renewal every three years. Physical therapy board certifications need renewal every ten years. Occupational therapy specialty certifications have varying renewal cycles depending on the specific credential.
Updating payer files with renewed credentials must happen promptly. When you renew your state license or national certification, submit updated documentation to all payers within 30 days. Some payers pull updates automatically from online databases, but others require direct notification. Don’t assume payers will discover your renewals on their own.
Practice location changes trigger credentialing updates with most payers. Moving to a new office requires notifying all payers and potentially going through new site approvals. Adding additional practice locations means credentialing at those new sites. Keep payers informed of any address or location changes to prevent claim denials.
How Medwave Handles Allied Health Credentialing
 At Medwave, we specialize in billing, credentialing, and payer contracting for all types of healthcare providers, including allied health professionals across every specialty. Our team knows the specific requirements for physical therapists, occupational therapists, speech-language pathologists, dietitians, and other allied health professions.
At Medwave, we specialize in billing, credentialing, and payer contracting for all types of healthcare providers, including allied health professionals across every specialty. Our team knows the specific requirements for physical therapists, occupational therapists, speech-language pathologists, dietitians, and other allied health professions.
We handle the entire credentialing process from gathering initial documentation through final payer approvals and ongoing recredentialing. Our specialists track the unique requirements for each profession, monitor application timelines across multiple payers, and follow up consistently to keep things moving forward.
We know which payers actively credential which allied health professions in different regions. This knowledge prevents wasted time applying to payers with closed panels or limited coverage for your services. We also help you prioritize payer applications based on your patient population and potential revenue impact.
For allied health practices trying to handle credentialing internally, the time and expertise required often overwhelms administrative staff. Outsourcing to Medwave gives you access to specialists who credential allied health professionals daily and know how to avoid the pitfalls that cause delays. We become your credentialing department, handling all the details while you focus on patient care.

