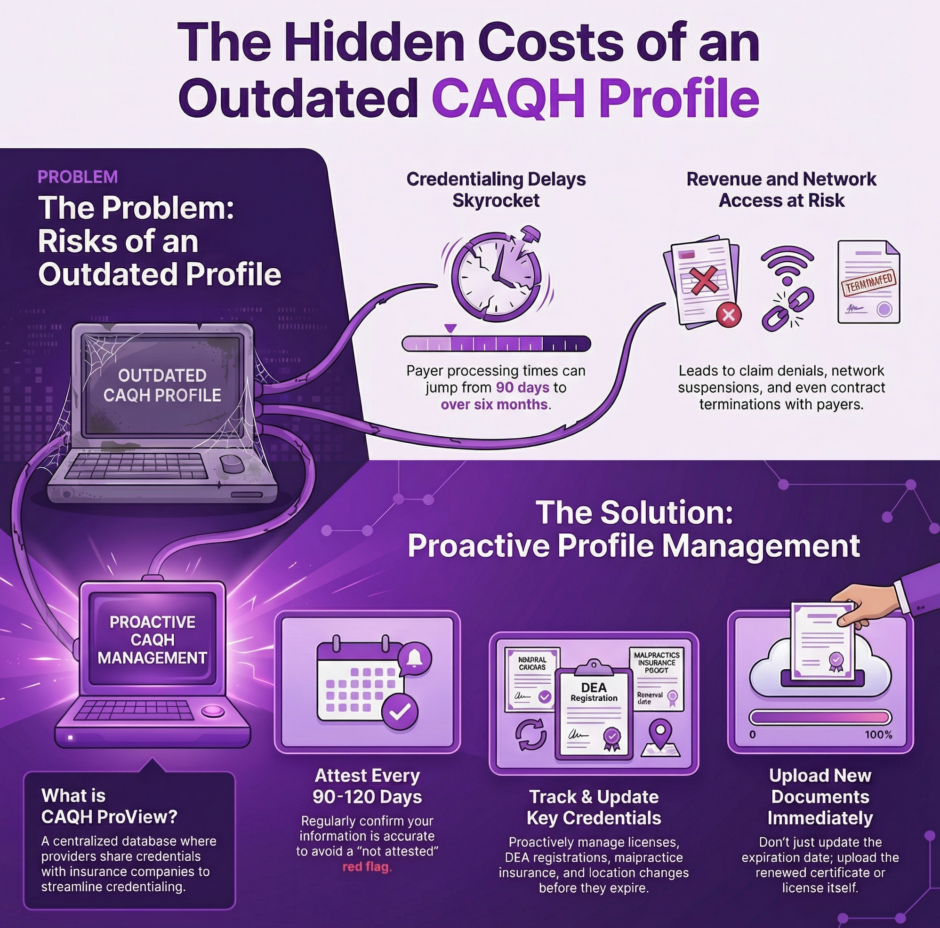
Healthcare providers face countless administrative tasks competing for their attention, and keeping a CAQH profile updated might seem like just another box to check. However, this database serves as the foundation for credentialing with insurance companies across the United States. An outdated CAQH profile can derail your credentialing status, delay payments, and even prevent you from seeing patients. Here’s why maintaining current information in your CAQH profile deserves priority attention.
What is CAQH ProView?
 The Council for Affordable Quality Healthcare (CAQH) operates ProView, a centralized database that healthcare providers use to share their professional credentials with insurance companies. Instead of filling out separate credentialing applications for each payer, providers enter their information once into CAQH ProView. Insurance companies then access this standardized data when credentialing providers or verifying their status.
The Council for Affordable Quality Healthcare (CAQH) operates ProView, a centralized database that healthcare providers use to share their professional credentials with insurance companies. Instead of filling out separate credentialing applications for each payer, providers enter their information once into CAQH ProView. Insurance companies then access this standardized data when credentialing providers or verifying their status.
More than 1,800 healthcare organizations use CAQH ProView, including most major insurance carriers, hospital systems, and managed care organizations. The database contains professional information like medical school education, residency training, board certifications, state licenses, DEA registrations, malpractice insurance, work history, and practice locations. This centralized system saves both providers and payers tremendous time and effort in the credentialing process.
CAQH ProView requires providers to attest that their information is accurate and current at least every 120 days. This attestation period creates a regular cycle where providers must review and update their profiles. While four months might seem like a long time, credentials can change quickly. Licenses renew, certifications expire, insurance policies update, and practice locations shift. Missing these updates creates problems.
The Direct Impact on Credentialing
Insurance companies rely heavily on CAQH ProView data when processing credentialing applications and conducting routine verifications. When your CAQH profile shows outdated information, it creates red flags that slow down or stop the credentialing process entirely.
Imagine you recently renewed your state medical license, but your CAQH profile still shows the old expiration date. When a payer checks your credentials, they see what appears to be an expired license. This triggers additional verification steps, delays in processing, and questions about your current eligibility. The payer might send requests for updated documentation or even put your application on hold until the discrepancy gets resolved. What should have been a routine verification turns into a time-consuming problem.
Similarly, if you’ve moved to a new practice location but haven’t updated your CAQH profile, insurance companies might be sending important correspondence to the wrong address. Contract documents, reimbursement checks, and credentialing updates could go to your old office, creating gaps in communication and potential compliance issues. These problems compound over time and become harder to fix the longer they persist.
Problems Caused by Outdated CAQH Information
An outdated CAQH profile creates multiple issues that directly affect your practice operations and revenue:
- Credentialing delays: Payers put applications on hold when they find discrepancies between your CAQH data and other verification sources, extending processing times from 90 days to six months or more
- Claim denials: Insurance companies flag claims when provider information doesn’t match their records, resulting in denied or held payments that hurt cash flow
- Network suspensions: Payers may temporarily suspend your network status if your CAQH profile shows expired credentials, preventing you from seeing patients until the issue resolves
- Contract terminations: Some insurance companies will terminate provider agreements if credentials cannot be verified during recredentialing due to outdated CAQH information
- Lost correspondence: Important documents like contract updates, payment checks, and credentialing notices go to wrong addresses when you don’t update location changes
- Compliance violations: Regulatory audits may flag outdated credential information as a compliance issue, potentially triggering additional scrutiny of your practice
Each of these problems costs time, money, and professional reputation. The administrative burden of fixing CAQH-related issues diverts staff attention from patient care and revenue-generating activities.
Recredentialing and Ongoing Verification
 Most insurance contracts require periodic recredentialing, typically every two to three years. During recredentialing, payers conduct thorough reviews of provider credentials to ensure continued network participation. They pull data from CAQH ProView as a primary source for this verification.
Most insurance contracts require periodic recredentialing, typically every two to three years. During recredentialing, payers conduct thorough reviews of provider credentials to ensure continued network participation. They pull data from CAQH ProView as a primary source for this verification.
If your CAQH profile is outdated during a recredentialing cycle, the process hits immediate roadblocks. Payers may request additional documentation, extend the review timeline, or even terminate your contract if they cannot verify current credentials. Being removed from an insurance network due to outdated CAQH information is entirely preventable but remarkably damaging. You lose the ability to see those patients, and getting reinstated requires going through the entire credentialing process again, which typically takes 90 to 120 days.
Beyond scheduled recredentialing, many payers conduct ongoing verification of provider credentials. They might check CAQH profiles monthly or quarterly to ensure their network providers maintain current licenses, certifications, and insurance coverage. An expired credential in your CAQH profile could trigger an immediate review of your network status, potentially leading to suspension until you update the information and the payer completes their verification.
Credentials That Need Regular Updates
Several types of credentials require frequent attention in your CAQH profile.
Staying ahead of these updates prevents last-minute scrambles when attestation deadlines approach:
- State Medical Licenses: Renew every 1-3 years depending on your state; update CAQH immediately upon receiving renewal confirmation
- Board Certifications: Expire every 7-10 years based on specialty board requirements; some require ongoing maintenance of certification activities
- DEA Registrations: Renew every 3 years; critical for prescribing authority and insurance credentialing
- Malpractice Insurance: Typically renews annually; update policy numbers, coverage amounts, and expiration dates with each renewal
- Professional Liability Coverage: Upload new declarations pages and certificates when changing carriers or renewing policies
- Work History: Add new positions, end dates for previous employment, and any gaps in practice
- Practice Locations: Update when opening new offices, closing locations, or changing addresses
- Contact Information: Keep phone numbers, email addresses, and billing addresses current for payer communications
- Hospital Privileges: Update when gaining or losing privileges at medical facilities
- Professional References: Ensure contact information for references remains accurate and current
Missing updates to any of these credentials can trigger credentialing delays or complications. Set reminders 60 to 90 days before expiration dates to allow time for renewals and CAQH updates before anything lapses.
The 120-Day Attestation Requirement
 CAQH ProView requires providers to attest to the accuracy of their information every 120 days. This attestation serves multiple purposes. It ensures that providers regularly review their information, confirms that the data remains accurate, and demonstrates ongoing engagement with the credentialing process.
CAQH ProView requires providers to attest to the accuracy of their information every 120 days. This attestation serves multiple purposes. It ensures that providers regularly review their information, confirms that the data remains accurate, and demonstrates ongoing engagement with the credentialing process.
Missing an attestation deadline can have immediate consequences. Your CAQH profile status changes to “not attested” or “re-attestation required,” which signals to insurance companies that your information may not be current. Many payers will not process credentialing applications or complete recredentialing reviews until you attest to your profile. Some payers may even suspend your network participation if your CAQH status shows as not attested for an extended period.
Setting up reminders to attest every 90 days, rather than waiting the full 120 days, provides a buffer against missed deadlines. This approach also creates natural opportunities to review your information for any needed updates. Many providers find it helpful to tie their CAQH review to other regular administrative tasks, such as quarterly financial reviews or license renewal tracking.
Document Management in CAQH
CAQH ProView allows providers to upload supporting documents like licenses, certificates, and insurance policies. These documents provide verification for the information entered in your profile. Keeping these documents current is just as important as updating the data fields themselves.
Many credentials require you to upload actual copies of certificates or licenses. When these credentials renew, you need to upload the new documents to CAQH. Don’t assume that updating the expiration date is sufficient. Credentialing specialists often need to see the actual renewed document to complete their verification process. Missing documents can delay credentialing just as much as outdated information.
Pay attention to document expiration dates. CAQH flags documents that are approaching expiration or have already expired. Upload renewed documents as soon as you receive them, rather than waiting until the old documents expire. This proactive approach keeps your profile in good standing and prevents gaps in documentation.
The Financial Cost of Neglecting Your CAQH Profile
 Healthcare providers sometimes underestimate the financial impact of an outdated CAQH profile. The costs accumulate in multiple ways, creating a significant burden on practice revenue and operations.
Healthcare providers sometimes underestimate the financial impact of an outdated CAQH profile. The costs accumulate in multiple ways, creating a significant burden on practice revenue and operations.
Lost patient volume represents the most obvious cost. If your credentialing gets delayed or suspended due to CAQH issues, you cannot see patients covered by that insurance plan. Depending on the payer’s market share in your area, this could mean turning away dozens or hundreds of patients. Each missed appointment represents lost revenue that you cannot recover.
Claim denials due to credentialing issues also drain practice resources. Your billing team must identify the problem, contact the payer, resolve the credentialing issue, correct the claim, and resubmit. This process takes significant staff time and often results in delayed payment. Some claims may be denied completely if they fall outside the payer’s timely filing limits before the credentialing issue gets resolved.
Administrative costs increase when dealing with CAQH-related problems. Staff members spend hours researching issues, gathering updated documentation, contacting payers, and following up on applications. These hours could be spent on more productive activities like patient care, practice development, or revenue cycle improvement.
How Professional Services Can Help
Many healthcare providers find CAQH maintenance challenging to fit into their busy schedules. Between patient care, clinical documentation, continuing education, and practice management, finding time to review and update CAQH profiles often falls to the bottom of the priority list. This is where professional credentialing services provide substantial value.
Companies like Medwave specialize in billing, credentialing, and payer contracting. These services include CAQH profile management as a core offering. Professional credentialing specialists monitor attestation deadlines, track credential expiration dates, update profile information as changes occur, and upload supporting documents. They handle the administrative details so providers can focus on patient care.
Working with credentialing partners also reduces the risk of errors or missed updates. These specialists know exactly what information payers need, how to format documentation correctly, and when updates must be completed. Their expertise prevents the common mistakes that can delay credentialing or trigger payer audits.
Best Practices for CAQH Profile Management
Maintaining an accurate, current CAQH profile requires establishing good habits and systems.
Here are the key practices that keep your profile current and your credentialing status secure:
Establish a Regular Review Schedule
- Review your CAQH profile monthly or quarterly rather than waiting for attestation deadlines
- Check for any information that has changed since your last review
- Verify that all expiration dates reflect current credentials
- Look for outdated contact information or practice locations
Track All Credential Expiration Dates
- Maintain a calendar or spreadsheet listing when licenses, certifications, and insurance policies expire
- Set reminders 60 to 90 days before expiration dates
- Allow time to complete renewals and update CAQH before credentials lapse
- Include both primary expiration dates and any interim requirements
Upload Documents Immediately
- Add renewed licenses to CAQH as soon as you receive them
- Upload updated insurance certificates when policies renew
- Include new certifications the day you complete them
- Don’t let credential documents pile up on your desk
Verify Information During Attestation
- Actually read each section instead of clicking through quickly
- Check for outdated addresses, phone numbers, or email addresses
- Review coverage amounts on malpractice insurance
- Confirm that all practice locations remain accurate
Communicate Changes Promptly
- Update CAQH immediately when moving to a new practice
- Change contact information when phone numbers or emails update
- Add new office locations as soon as they open
- Remove closed locations to prevent confusion
Maintain Personal Backup Records
- Keep copies of all licenses, certifications, and insurance policies in your own files
- Store documents in an organized system for easy retrieval
- Use these records to quickly upload documents to CAQH when needed
- Have backup documentation available if questions arise about credentials
Warning Signs Your CAQH Profile Needs Attention
Several indicators suggest your CAQH profile requires immediate attention:
- You haven’t attested to your profile in the past 90 days
- Your CAQH status shows as “re-attestation required” or “incomplete”
- Any of your credentials have expired or will expire within 30 days
- You’ve received notification from a payer about credentialing issues
- Claims are being denied due to provider eligibility problems
- You’ve changed practice locations but haven’t updated your address
- Your malpractice insurance has renewed but the old policy shows in CAQH
- Payers are sending correspondence to incorrect addresses
- You’ve completed new board certification but it’s not reflected in your profile
- Your state license has renewed but CAQH shows the old expiration date
If any of these situations apply to you, log into your CAQH profile immediately and make the necessary updates. Addressing these issues quickly prevents them from growing into larger problems that affect your credentialing status and practice revenue.
Summary: Keeping Your CAQH Profile Up to Date is Crucial
 Your CAQH profile functions as the central hub for your professional credentials in the healthcare industry. Keeping it current is not optional or a mere suggestion. It’s a vital requirement that directly affects your ability to participate in insurance networks, receive timely payment for your services, and maintain professional standing in the healthcare community.
Your CAQH profile functions as the central hub for your professional credentials in the healthcare industry. Keeping it current is not optional or a mere suggestion. It’s a vital requirement that directly affects your ability to participate in insurance networks, receive timely payment for your services, and maintain professional standing in the healthcare community.
The time invested in regular CAQH maintenance pays significant returns through smoother credentialing processes, fewer claim denials, better payer relationships, and uninterrupted patient care. Whether you manage your CAQH profile internally or partner with professional credentialing services, making this task a priority protects your practice from preventable administrative problems and financial losses.
Think of CAQH profile maintenance as preventive medicine for your practice. A small investment of time on a regular basis prevents major headaches down the road. Set up your systems, establish your routines, and commit to keeping your CAQH profile current. Your practice, your staff, and your patients will all benefit from this attention to an often-overlooked but critically important administrative responsibility.

