Healthcare providers often find themselves navigating two critical but distinct processes when establishing relationships with insurance companies and healthcare networks: credentialing and contracting. While these terms are frequently used interchangeably, they represent separate phases in the provider enrollment journey, each with unique requirements, timelines, and outcomes.
 Knowing the difference between credentialing and contracting is essential for healthcare practitioners, practice administrators, and anyone involved in healthcare business operations. This knowledge can significantly impact revenue cycles, patient access, and overall practice success.
Knowing the difference between credentialing and contracting is essential for healthcare practitioners, practice administrators, and anyone involved in healthcare business operations. This knowledge can significantly impact revenue cycles, patient access, and overall practice success.
Medical Credentialing Essentials
Medical credentialing serves as the foundation of healthcare provider verification. This process involves thoroughly vetting a healthcare provider’s qualifications, background, and professional standing to ensure they meet specific standards for delivering patient care.
Primary Components of Credentialing
- Verification of medical education and training
- Confirmation of board certifications and licenses
- Review of malpractice insurance coverage
- Background checks including criminal history
- Verification of work history and references
- Hospital privileges and affiliations review
- Assessment of any sanctions or disciplinary actions
The credentialing process typically takes 90 to 180 days, though some cases may extend longer depending on the thoroughness of documentation and responsiveness of verifying organizations. During this period, credentialing organizations contact medical schools, residency programs, state licensing boards, and previous employers to confirm the accuracy of submitted information.
Healthcare facilities, insurance companies, and medical networks all maintain credentialing departments or work with third-party credentialing organizations to manage these verifications. The goal remains consistent across all entities: ensuring that only qualified, competent healthcare providers deliver patient care within their networks.
The Contracting Process Explained
Contracting represents the business relationship establishment between healthcare providers and payers or healthcare organizations. This process focuses on negotiating terms, conditions, and financial arrangements that will govern the professional relationship.
Key Elements of Healthcare Contracting
- Fee schedules and reimbursement rates
- Payment terms and timelines
- Covered services and procedures
- Geographic service areas
- Performance metrics and quality measures
- Termination clauses and renewal terms
- Administrative requirements and reporting obligations
 Contract negotiations can vary significantly in duration and intensity. Some standard network contracts may be accepted with minimal modification, while others require extensive back-and-forth discussions to reach mutually acceptable terms. The contracting process often involves legal review, risk assessment, and strategic decision-making regarding the financial viability of the proposed arrangement.
Contract negotiations can vary significantly in duration and intensity. Some standard network contracts may be accepted with minimal modification, while others require extensive back-and-forth discussions to reach mutually acceptable terms. The contracting process often involves legal review, risk assessment, and strategic decision-making regarding the financial viability of the proposed arrangement.
Unlike credentialing, which focuses on qualifications and competency, contracting centers on business terms and operational requirements. The contract becomes the legal framework that defines how the provider and payer will interact, including billing procedures, claim submission requirements, and dispute resolution mechanisms.
Timeline and Sequential Relationship
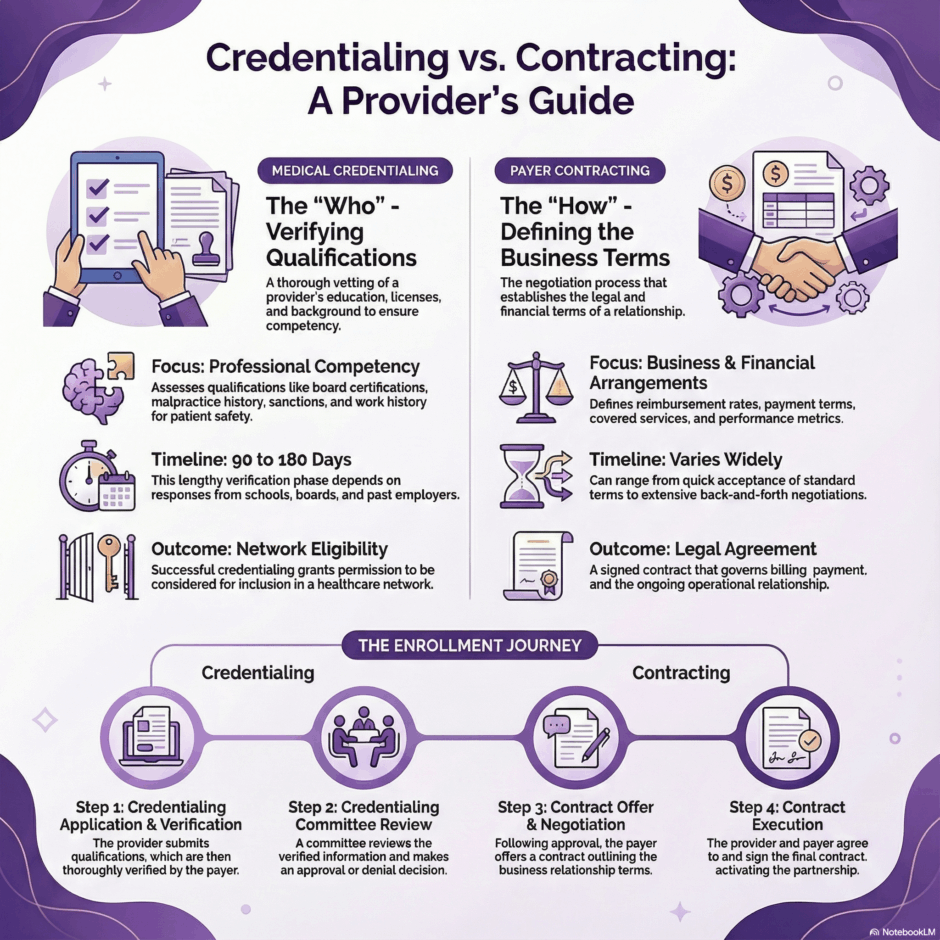
One of the most important distinctions between credentialing and contracting lies in their sequential nature and timing. Credentialing almost always precedes contracting, as insurance companies and healthcare networks require verified provider credentials before entering into business relationships.
The typical sequence follows this pattern:
- Phase 1: Initial Application
Healthcare providers submit credentialing applications containing detailed professional information, supporting documentation, and required attestations. This marks the beginning of the credentialing timeline. - Phase 2: Verification Process
Credentialing staff or organizations begin the systematic verification of submitted information. This phase often represents the longest portion of the overall timeline, as it depends on responses from multiple external verification sources. - Phase 3: Committee Review
Once verifications are complete, credentialing committees review the assembled information to make acceptance or denial decisions. These committees typically include healthcare professionals who evaluate peers based on established criteria. - Phase 4: Contract Offer
Following successful credentialing approval, the contracting phase begins. Contract specialists present proposed agreements outlining business terms and operational requirements. - Phase 5: Contract Negotiation and Execution
Providers review proposed contracts, negotiate terms when possible, and execute final agreements. This phase can range from simple acceptance to extended negotiation periods.
Documentation Requirements Differ Significantly
The documentation requirements for credentialing and contracting processes differ substantially in both scope and purpose. Credentialing documentation focuses on professional qualifications and competency verification.
Essential Credentialing Documents
- Medical school diplomas and transcripts
- Residency and fellowship completion certificates
- Current medical licenses and DEA registrations
- Board certification documents
- Malpractice insurance certificates
- Hospital privilege letters
- Professional references and peer recommendations
- Work history with employment verification
Contracting documentation, by contrast, emphasizes business operations and legal considerations. These documents establish the framework for ongoing business relationships rather than verifying past achievements or qualifications.
Typical Contracting Documents
- Business license and tax identification numbers
- Professional liability insurance policies
- Facility accreditation certificates
- HIPAA compliance attestations
- Electronic health record system information
- Billing and claims processing capabilities
- Quality reporting system documentation
Financial Implications and Considerations
 The financial implications of credentialing and contracting processes differ markedly in their impact on healthcare practices. Credentialing represents an investment in market access, while contracting directly affects ongoing revenue streams and operational costs.
The financial implications of credentialing and contracting processes differ markedly in their impact on healthcare practices. Credentialing represents an investment in market access, while contracting directly affects ongoing revenue streams and operational costs.
Credentialing costs typically include application fees, document preparation expenses, and administrative time investments. These represent one-time or periodic expenses that enable market participation but don’t directly generate revenue. However, successful credentialing opens doors to patient populations and revenue opportunities that would otherwise remain inaccessible.
Contracting decisions have immediate and ongoing financial implications. Fee schedules negotiated during contracting directly impact per-service revenue, while payment terms affect cash flow timing. Administrative requirements specified in contracts can increase operational costs through additional reporting, quality measurement, or technology investments.
Revenue Impact Factors in Contracting
- Reimbursement rates for specific services
- Payment timing and processing requirements
- Administrative burden and associated costs
- Volume commitments or performance incentives
- Risk-sharing arrangements and quality bonuses
Regulatory and Compliance Differences
Both credentialing and contracting operate within regulatory frameworks, but they address different compliance requirements and oversight mechanisms. Credentialing compliance focuses on professional standards and patient safety regulations.
The Joint Commission, National Committee for Quality Assurance, and Centers for Medicare & Medicaid Services all maintain credentialing standards that healthcare organizations must follow. These standards emphasize thorough verification processes, regular re-credentialing cycles, and ongoing monitoring of provider performance and standing.
Contracting compliance involves different regulatory considerations, including anti-kickback statutes, Stark Law provisions, and fair dealing requirements. Contracts must comply with federal and state regulations governing healthcare business relationships while avoiding arrangements that could be construed as improper referral incentives.
Technology and System Integration
Modern credentialing and contracting processes increasingly rely on technology platforms, but they utilize different systems and databases to accomplish their respective objectives. Credentialing software focuses on verification workflows and document management.
Credentialing Technology Features
- Primary source verification databases
- Document imaging and storage systems
- Workflow management and task tracking
- Automated status notifications and updates
- Integration with professional licensing boards
- Committee review and decision tracking
Contracting systems emphasize relationship management and ongoing performance monitoring. These platforms support contract lifecycle management from initial negotiation through renewal or termination.
Contracting System Capabilities
- Contract template libraries and modification tools
- Rate schedule management and updating
- Performance metric tracking and reporting
- Payment processing integration
- Renewal date monitoring and alerts
- Amendment and modification workflow
Recredentialing vs. Contract Renewal
 The ongoing maintenance of provider relationships involves both recredentialing and contract renewal processes, which operate on different cycles and focus on distinct evaluation criteria. Recredentialing typically occurs every two to three years and requires updated verification of professional qualifications and standing.
The ongoing maintenance of provider relationships involves both recredentialing and contract renewal processes, which operate on different cycles and focus on distinct evaluation criteria. Recredentialing typically occurs every two to three years and requires updated verification of professional qualifications and standing.
During recredentialing, providers must demonstrate continued competency, current licensure, and absence of disqualifying events or sanctions. The process resembles initial credentialing but may streamline certain verifications for providers with established performance records.
Contract renewals may occur on different timelines, ranging from annual reviews to multi-year terms. These renewals focus on business performance, market conditions, and mutual satisfaction with existing arrangements. Financial terms, service offerings, and administrative requirements may all be subject to modification during renewal negotiations.
Strategic Considerations for Healthcare Providers
Healthcare providers must approach credentialing and contracting as complementary but distinct strategic activities. Successful credentialing enables network participation, while effective contracting ensures sustainable business relationships.
Provider organizations should maintain organized credential files and documentation systems that facilitate both initial credentialing and ongoing recredentialing requirements. This preparation reduces processing delays and demonstrates professional organization to credentialing committees.
For contracting purposes, providers benefit from understanding their practice economics, competitive positioning, and negotiation priorities before entering into contract discussions. Market research regarding standard reimbursement rates and contract terms helps inform negotiation strategies and decision-making.
Common Challenges and Solutions
![]() Both credentialing and contracting present unique challenges that healthcare providers must navigate successfully. Credentialing delays often result from incomplete applications, slow verification responses, or missing documentation. Proactive application preparation and follow-up communication can minimize these delays.
Both credentialing and contracting present unique challenges that healthcare providers must navigate successfully. Credentialing delays often result from incomplete applications, slow verification responses, or missing documentation. Proactive application preparation and follow-up communication can minimize these delays.
Contracting challenges frequently involve rate negotiations, administrative requirements, and contract term conflicts. Providers can address these challenges through careful contract review, professional negotiation assistance when needed, and clear understanding of their practice requirements and limitations.
The distinction between credentialing and contracting represents more than administrative terminology. These processes serve different purposes, follow different timelines, and require different approaches to successful completion. Healthcare providers who understand these differences can better navigate both processes, optimize their network participation strategies, and build sustainable payer relationships that support long-term practice success.
Ultimately, this knowledge contributes to more efficient provider enrollment, better contract terms, and improved patient access to quality healthcare services.

