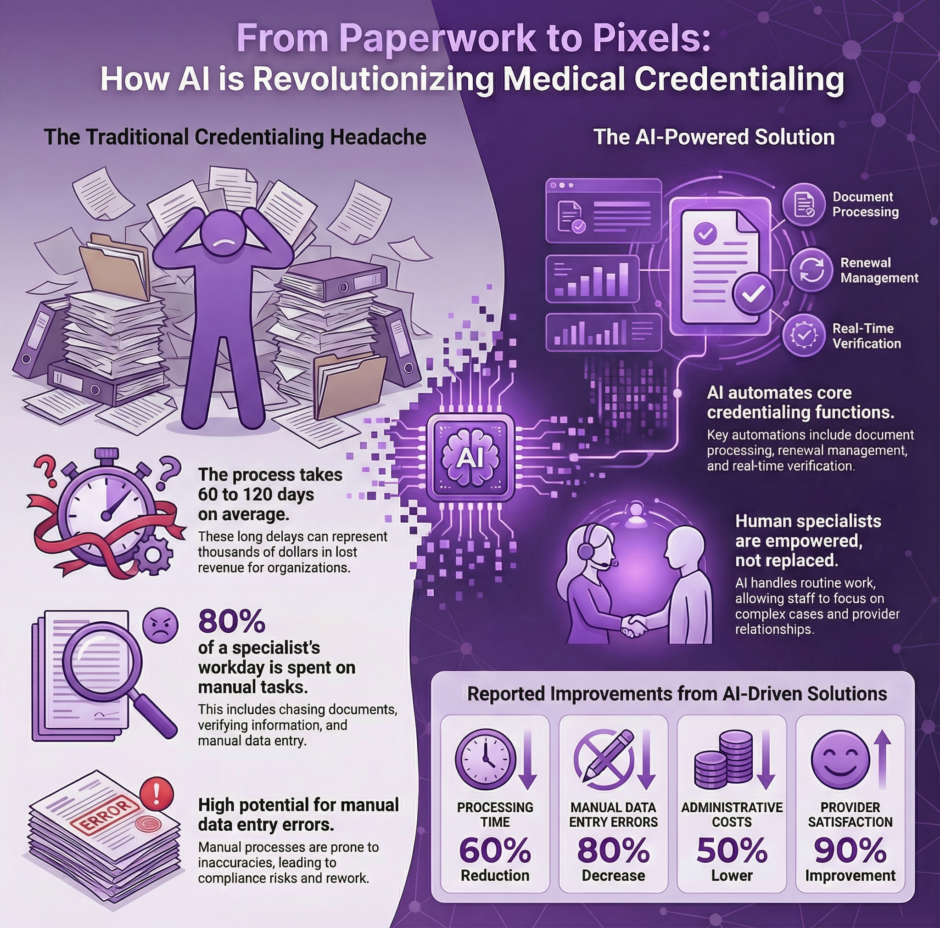
Medical credentialing has long been one of healthcare’s most time-intensive administrative processes. The traditional approach involves mountains of paperwork, manual verification of credentials, and weeks or months of waiting for approvals. Today, artificial intelligence is reshaping this landscape, bringing speed, accuracy, and efficiency to a process that affects every healthcare provider’s ability to practice and receive payment for their services.
The Current State of Medical Credentialing
Before diving into AI’s role, it’s worth examining what medical credentialing entails. This process verifies that healthcare providers have the proper qualifications, licenses, training, and background to deliver medical services. Insurance companies, hospitals, and healthcare systems require this verification before allowing providers to treat patients and submit claims for reimbursement.
 The traditional credentialing workflow typically includes verifying medical school graduation, residency completion, board certifications, malpractice history, and state licensing. Each step requires human reviewers to contact various institutions, cross-reference databases, and manually validate information. This labor-intensive process often takes 90 to 180 days, during which new providers cannot see patients or generate revenue.
The traditional credentialing workflow typically includes verifying medical school graduation, residency completion, board certifications, malpractice history, and state licensing. Each step requires human reviewers to contact various institutions, cross-reference databases, and manually validate information. This labor-intensive process often takes 90 to 180 days, during which new providers cannot see patients or generate revenue.
Healthcare organizations struggle with credentialing backlogs, especially given the current provider shortage. Every day a qualified physician or specialist waits for credentialing approval represents lost patient care opportunities and reduced organizational revenue. The manual nature of verification also introduces potential for human error, which can delay the process even further.
How AI Transforms Credentialing Workflows
Artificial intelligence addresses these challenges by automating many verification steps and accelerating the entire process. Modern AI systems can instantly access multiple databases, cross-reference information, and flag discrepancies that require human attention. This automation doesn’t replace human oversight but rather handles routine verification tasks, allowing credentialing specialists to focus on exception cases and quality assurance.
AI-powered credentialing platforms can verify medical licenses across all 50 states simultaneously, rather than checking each jurisdiction individually. The technology connects to primary sources like state medical boards, educational institutions, and certification bodies, pulling real-time data instead of relying on potentially outdated documents submitted by providers.
Machine learning algorithms can also identify patterns that might indicate fraudulent credentials or red flags in a provider’s background. These systems learn from historical data to recognize anomalies that human reviewers might miss, adding an extra layer of security to the credentialing process.
Primary Source Verification Gets Smarter
 One of AI’s most significant contributions to medical credentialing lies in primary source verification (PSV). This requirement mandates that credentialing organizations verify information directly with the original issuing source rather than accepting copies of documents. Traditionally, this meant phone calls, faxes, and emails to medical schools, residency programs, and licensing boards, a process that could take weeks for each verification.
One of AI’s most significant contributions to medical credentialing lies in primary source verification (PSV). This requirement mandates that credentialing organizations verify information directly with the original issuing source rather than accepting copies of documents. Traditionally, this meant phone calls, faxes, and emails to medical schools, residency programs, and licensing boards, a process that could take weeks for each verification.
AI systems now interface directly with these primary sources through APIs and secure data connections. When a provider submits their medical school information, the AI system can instantly verify graduation dates, degrees earned, and academic standing with the institution’s registrar office. This real-time verification eliminates waiting periods and reduces the chance of accepting falsified documents.
The technology also maintains updated databases of contact information for thousands of educational and certification organizations worldwide. As institutions change their verification processes or contact details, AI systems can automatically update their records, ensuring verification requests reach the right departments without delays.
Automated Document Processing and Analysis
Healthcare providers must submit extensive documentation during credentialing, including curriculum vitae, certificates, licenses, and attestation forms. AI-powered optical character recognition (OCR) and natural language processing (NLP) technologies can automatically extract relevant information from these documents, eliminating manual data entry.
These systems can read various document formats, from scanned PDFs to digital certificates, and populate credentialing databases with extracted information. AI algorithms can also cross-reference data across multiple documents to identify inconsistencies. For example, if a provider’s CV lists a residency completion date that doesn’t match their residency certificate, the system flags this discrepancy for human review.
Document analysis extends beyond simple data extraction. AI can verify document authenticity by checking security features, watermarks, and formatting against known templates from issuing institutions. This capability helps prevent credential fraud and ensures only legitimate qualifications are accepted.
Continuous Monitoring and Recredentialing
 Medical credentialing isn’t a one-time event. Healthcare organizations must continuously monitor their providers’ credentials and conduct periodic re-credentialing, typically every two to three years. AI systems excel at this ongoing monitoring by automatically checking for license renewals, board certification updates, and any disciplinary actions.
Medical credentialing isn’t a one-time event. Healthcare organizations must continuously monitor their providers’ credentials and conduct periodic re-credentialing, typically every two to three years. AI systems excel at this ongoing monitoring by automatically checking for license renewals, board certification updates, and any disciplinary actions.
These monitoring systems can track hundreds or thousands of providers simultaneously, sending alerts when credentials are due for renewal or when negative actions appear in regulatory databases. This proactive approach prevents situations where providers’ credentials lapse without the organization’s knowledge, which could result in compliance violations or interrupted patient care.
AI-powered monitoring also extends to insurance panel participation. The technology can track which providers are credentialed with which insurance plans and alert organizations when new opportunities arise or when existing contracts require attention.
Data Integration and Interoperability
Modern healthcare operates across multiple systems and platforms, each maintaining its own provider databases. AI facilitates better integration between these systems, allowing credentialing data to flow seamlessly between electronic health records, billing systems, and practice management platforms.
This integration eliminates duplicate data entry and ensures all systems maintain current provider information. When a provider’s board certification is renewed, for example, AI systems can automatically update this information across all relevant platforms, maintaining data consistency and accuracy.
The technology also enables better data sharing between healthcare organizations. When providers move between health systems or join additional practices, their credentialing data can transfer more efficiently, reducing the time needed for re-credentialing at new organizations.
Key Benefits of AI-Assisted Credentialing
The advantages of implementing AI in medical credentialing extend far beyond simple time savings:
- Speed: AI reduces credentialing timeframes from months to days or weeks
- Accuracy: Automated verification reduces human error and ensures data consistency
- Cost reduction: Less manual labor translates to lower administrative costs
- Provider satisfaction: Faster credentialing means providers can begin practicing sooner
- Compliance: Automated monitoring helps maintain regulatory compliance
- Scalability: AI systems can handle increasing credentialing volumes without proportional staff increases
Implementation Challenges and Considerations
 While AI offers significant benefits for medical credentialing, organizations must address several challenges when implementing these technologies. Data security remains paramount, given the sensitive nature of provider information. AI systems must comply with healthcare privacy regulations like HIPAA and ensure all data transmission and storage meet industry security standards.
While AI offers significant benefits for medical credentialing, organizations must address several challenges when implementing these technologies. Data security remains paramount, given the sensitive nature of provider information. AI systems must comply with healthcare privacy regulations like HIPAA and ensure all data transmission and storage meet industry security standards.
Integration with existing systems can also present challenges. Many healthcare organizations operate legacy credentialing systems that may not easily interface with modern AI platforms. Planning for data migration and system integration requires careful coordination and potential temporary workflow adjustments.
Staff training represents another consideration. While AI automates many tasks, credentialing professionals need to learn how to work with these new systems effectively. This includes recognizing when AI recommendations require human review and maintaining oversight of automated processes.
The Role of Human Oversight
Despite AI’s capabilities, human expertise remains crucial in medical credentialing. AI systems excel at routine verification tasks and pattern recognition, but complex cases often require human judgment. Unusual credential situations, international qualifications, or providers with complicated backgrounds may need manual review and decision-making.
The most effective AI implementations combine automation with human oversight. Credentialing specialists can focus on exception cases, quality assurance, and relationship management while AI handles standard verification tasks. This approach maximizes efficiency while maintaining the human touch necessary for complex credentialing decisions.
Medical Credentialing AI of Tomorrow
 The future of AI in medical credentialing holds even more promise. Blockchain technology may eventually provide immutable credential verification, while advanced machine learning could predict credentialing outcomes and identify potential issues before they occur.
The future of AI in medical credentialing holds even more promise. Blockchain technology may eventually provide immutable credential verification, while advanced machine learning could predict credentialing outcomes and identify potential issues before they occur.
Real-time credential verification may become the standard, where providers’ qualifications are continuously validated against primary sources. This would eliminate the need for periodic re-credentialing cycles and ensure credentials remain current at all times.
Integration with telemedicine platforms and multi-state licensing initiatives will also drive AI development in credentialing. As healthcare delivery becomes more geographically distributed, AI systems will need to handle increasingly varied regulatory requirements and verification processes.
Summary: How AI Helps the Ugly Credentialing Process
 Artificial intelligence is fundamentally changing medical credentialing from a slow, manual process to a fast, automated system that benefits providers, healthcare organizations, and ultimately patients. By handling routine verification tasks, monitoring credentials continuously, and integrating data across systems, AI addresses many of the longstanding challenges in credentialing.
Artificial intelligence is fundamentally changing medical credentialing from a slow, manual process to a fast, automated system that benefits providers, healthcare organizations, and ultimately patients. By handling routine verification tasks, monitoring credentials continuously, and integrating data across systems, AI addresses many of the longstanding challenges in credentialing.
The technology doesn’t replace human expertise but rather amplifies it, allowing credentialing professionals to focus on high-value activities while AI manages routine tasks. As healthcare continues to face provider shortages and increasing regulatory requirements, AI-assisted credentialing becomes not just beneficial but essential for maintaining efficient operations.
For healthcare organizations considering AI implementation, the question isn’t whether to adopt these technologies, but how quickly they can integrate them into their workflows. Companies like Medwave, which specialize in billing, credentialing, and payer contracting services, are already leveraging AI to deliver faster, more accurate credentialing services to their healthcare clients. The future of medical credentialing is here, and it’s powered by artificial intelligence.

