Healthcare organizations face an increasingly complex challenge: ensuring their medical staff are properly qualified, licensed, and safe to practice while managing an ever-growing mountain of documentation and regulatory requirements. Medical staff credentialing, once a purely paper-based process, has evolved into a sophisticated ecosystem of digital solutions that promise to streamline verification workflows, reduce errors, and maintain the highest standards of patient care. The undermentioned content discusses the world of medical staff credentialing solutions, from traditional methods to cutting-edge technologies that are reshaping how healthcare organizations manage their professional staff.
Understanding Medical Staff Credentialing
 Let’s start with the basics: medical staff credentialing is the systematic process of verifying the qualifications of healthcare providers, including their education, training, licensure, certifications, and professional background. It’s essentially a thorough background check that ensures healthcare providers are qualified to deliver safe, high-quality patient care.
Let’s start with the basics: medical staff credentialing is the systematic process of verifying the qualifications of healthcare providers, including their education, training, licensure, certifications, and professional background. It’s essentially a thorough background check that ensures healthcare providers are qualified to deliver safe, high-quality patient care.
The stakes couldn’t be higher. According to a 2023 report by the National Practitioner Data Bank (NPDB), over 400,000 adverse actions against healthcare practitioners were reported in the past decade, highlighting the critical importance of thorough credentialing processes. Moreover, studies have shown that inadequate credentialing can lead to significant financial penalties, with some malpractice cases resulting in settlements exceeding $10 million.
The Evolution of Credentialing Solutions
From Paper to Digital
Remember the days of massive filing cabinets stuffed with provider applications, certificates, and verification documents? Many healthcare organizations still haven’t fully escaped this reality.
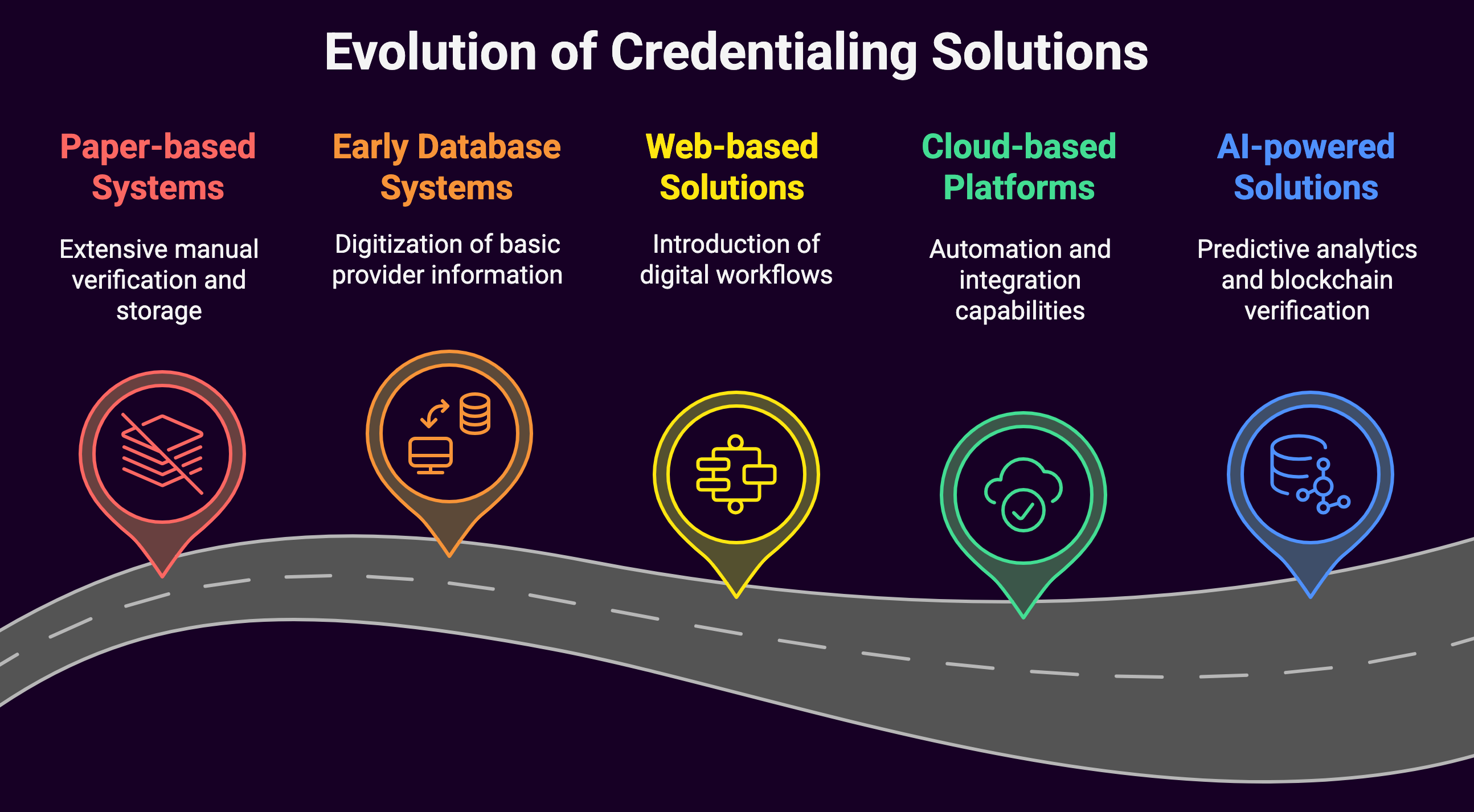
However, the industry has come a long way from purely manual processes:
- 1960s-1980s: Paper-based systems dominated, requiring extensive manual verification and physical storage
- 1990s: Early database systems began digitizing basic provider information
- 2000s: Web-based credentialing solutions emerged, offering basic digital workflows
- 2010s: Cloud-based platforms introduced automated verification and integration capabilities
- 2020s: AI-powered solutions with predictive analytics and blockchain verification are becoming mainstream
Current Market Landscape
The medical staff credentialing solutions market has experienced remarkable growth. According to recent market analyses, the global healthcare credentialing software market is expected to reach $2.9 billion by 2026, growing at a CAGR of 7.8% from 2021.
This growth is driven by:
- Increasing regulatory requirements
- Growing emphasis on patient safety
- Rising healthcare provider mobility
- Need for operational efficiency
- Shift toward value-based care models
Key Components of Modern Credentialing Solutions
Primary Source Verification (PSV)
The foundation of any credentialing solution is its ability to perform primary source verification.
Modern systems can automatically verify credentials with:
- Medical schools and training programs
- State licensing boards
- Specialty boards
- Previous employers
- Federal databases (NPDB, OIG, SAM)
- Malpractice insurers
The best solutions maintain direct interfaces with these primary sources, reducing verification time from weeks to days or even hours. Data shows that automated PSV can reduce credentialing costs by up to 60% compared to manual processes.
Workflow Automation
Modern credentialing solutions excel at automating complex workflows.
Key features include:
Application Processing
- Online application forms with smart validation
- Document upload capabilities
- Automatic data extraction from uploaded documents
- Real-time application status tracking
Verification Management
- Automated verification requests
- Response tracking and follow-up
- Exception handling for incomplete or questionable responses
- Digital signature integration
Committee Review
- Electronic committee packet preparation
- Online review and voting capabilities
- Meeting management tools
- Decision documentation
Research indicates that automated workflows can reduce credentialing cycle times by 25-50%, with some organizations reporting even greater improvements.
Compliance Management
Maintaining compliance with various regulatory bodies is a crucial function of credentialing solutions.
Modern platforms help organizations stay compliant with:
- Joint Commission standards
- NCQA requirements
- CMS regulations
- State-specific requirements
- Facility-specific bylaws
These systems typically include:
Monitoring and Alerts
- License expiration warnings
- Continuing education tracking
- Sanctions and disciplinary action alerts
- Insurance coverage monitoring
Reporting Capabilities
- Compliance dashboards
- Audit trail documentation
- Custom report generation
- Regulatory submission preparation
Integration Capabilities
Modern credentialing solutions don’t exist in isolation.
They need to integrate with various other healthcare systems:
Electronic Health Records (EHR)
- Provider demographics synchronization
- Privileges management
- Clinical quality data exchange
Human Resources Systems
- Employee information sharing
- Payroll system integration
- Benefits management coordination
Provider Enrollment Systems
- Payer enrollment automation
- CAQH integration
- Medicare/Medicaid enrollment support
Studies show that integrated systems can reduce data entry errors by up to 80% and save hundreds of staff hours annually.
Emerging Technologies in Credentialing Solutions
Artificial Intelligence and Machine Learning
AI is revolutionizing credentialing in several ways:
Document Processing
- Intelligent character recognition (ICR) for document digitization
- Natural language processing for content analysis
- Automated data validation and verification
Predictive Analytics
- Risk assessment of applications
- Expiration prediction and proactive renewal
- Workload forecasting and resource allocation
Process Optimization
- Workflow recommendations
- Automatic prioritization of tasks
- Pattern recognition for fraud detection
Early adopters of AI-powered credentialing solutions report up to 40% reduction in processing time and a 35% decrease in administrative costs.
Blockchain Technology
Blockchain is emerging as a promising solution for credential verification:
Benefits
- Immutable record of credentials
- Reduced fraud risk
- Instant verification capability
- Decentralized storage
- Provider-owned credentials
Several pilot programs have demonstrated blockchain’s potential, with verification times reduced from days to seconds in some cases.
Mobile Solutions
Mobile accessibility has become essential for modern credentialing solutions:
Provider Features
- Application submission
- Document upload
- Status tracking
- Renewal notifications
Administrator Features
- Application review
- Approval workflows
- Emergency privileging
- Remote committee participation
Organizations report increased provider satisfaction and faster turnaround times when mobile access is available.
Implementation Considerations
Selecting the Right Solution
When choosing a credentialing solution, organizations should consider:
Technical Requirements
- Cloud vs. on-premise hosting
- Integration capabilities
- Scalability
- Security features
- Backup and disaster recovery
Functional Requirements
- Workflow customization
- Reporting capabilities
- User interface design
- Mobile accessibility
- Support for specific specialties
Vendor Considerations
- Industry experience
- Customer support
- Training programs
- Update frequency
- Financial stability
Implementation Best Practices
Successful implementation requires careful planning:
Project Planning
- Clear timeline and milestones
- Resource allocation
- Risk management strategy
- Change management plan
Data Migration
- Data cleaning and standardization
- Legacy system assessment
- Validation protocols
- Parallel processing period
Training and Support
- Role-based training programs
- Super-user development
- Help desk establishment
- Ongoing education plan
Organizations that follow structured implementation methodologies report 30% higher user adoption rates and 40% faster time to value.
Cost Considerations and ROI
Investment Components
The total cost of ownership includes:
Initial Costs
- Software licensing
- Implementation services
- Hardware/infrastructure
- Data migration
- Training
Ongoing Costs
- Maintenance fees
- Support services
- Updates and upgrades
- Additional user licenses
- Integration maintenance
Return on Investment
ROI calculation should consider:
Direct Cost Savings
- Reduced staff time
- Lower paper and storage costs
- Decreased verification fees
- Fewer costly errors
Indirect Benefits
- Improved provider satisfaction
- Better regulatory compliance
- Reduced legal risk
- Enhanced patient safety
Studies indicate that organizations typically achieve credentialing ROI within 18-24 months of implementation, with some reporting payback periods as short as 12 months.
Future Trends and Predictions
Technology Evolution
Several trends are shaping the future of credentialing solutions:
Artificial Intelligence
- Advanced pattern recognition
- Automated decision support
- Real-time fraud detection
- Predictive maintenance
Interoperability
- Universal provider identifiers
- Cross-organization credential sharing
- National credential databases
- Real-time verification networks
User Experience
- Voice-enabled interfaces
- Augmented reality training
- Personalized workflows
- Contextual assistance
Industry Changes
The credentialing landscape continues to evolve:
Regulatory Environment
- Increased standardization
- Stricter verification requirements
- Enhanced privacy protection
- International credential recognition
Market Dynamics
- Industry consolidation
- New market entrants
- Partnership ecosystems
- Value-based solutions
Summary: Medical Staff Credentialing Solutions
Medical staff credentialing solutions have come a long way from their paper-based origins. Today’s digital platforms offer unprecedented efficiency, accuracy, and compliance capabilities. As healthcare organizations face growing pressure to maintain quality while controlling costs, modern credentialing solutions provide a crucial foundation for success.
The future promises even more innovation, with AI, blockchain, and mobile technologies leading the way. Organizations that embrace these advances while maintaining focus on their core mission of ensuring qualified providers and safe patient care will be best positioned for success.
Additional Resources
For those looking to dive deeper into medical staff credentialing solutions, consider exploring:
- NAMSS (National Association Medical Staff Services) educational resources
- Joint Commission credentialing standards
- NCQA credentialing toolkit
- Healthcare compliance publications
- Industry conferences and webinars
Successful credentialing management isn’t just about technology. It’s about combining the right tools with effective processes and skilled professionals to create a comprehensive solution that serves both healthcare providers and patients.
The investment in modern credentialing solutions may seem substantial, but the return in terms of efficiency, accuracy, and risk management makes it essential for healthcare organizations committed to excellence in patient care and provider management.

