Embarking on the Molina Healthcare credentialing journey? You’ve come to the right place. As a managed care organization with a strong focus on Medicaid and Medicare populations, Molina’s credentialing process has its own unique characteristics and requirements. Whether you’re a new provider looking to join their network or a practice manager handling multiple applications, we’ll walk you through everything you need to know to successfully navigate Molina’s credentialing terrain.
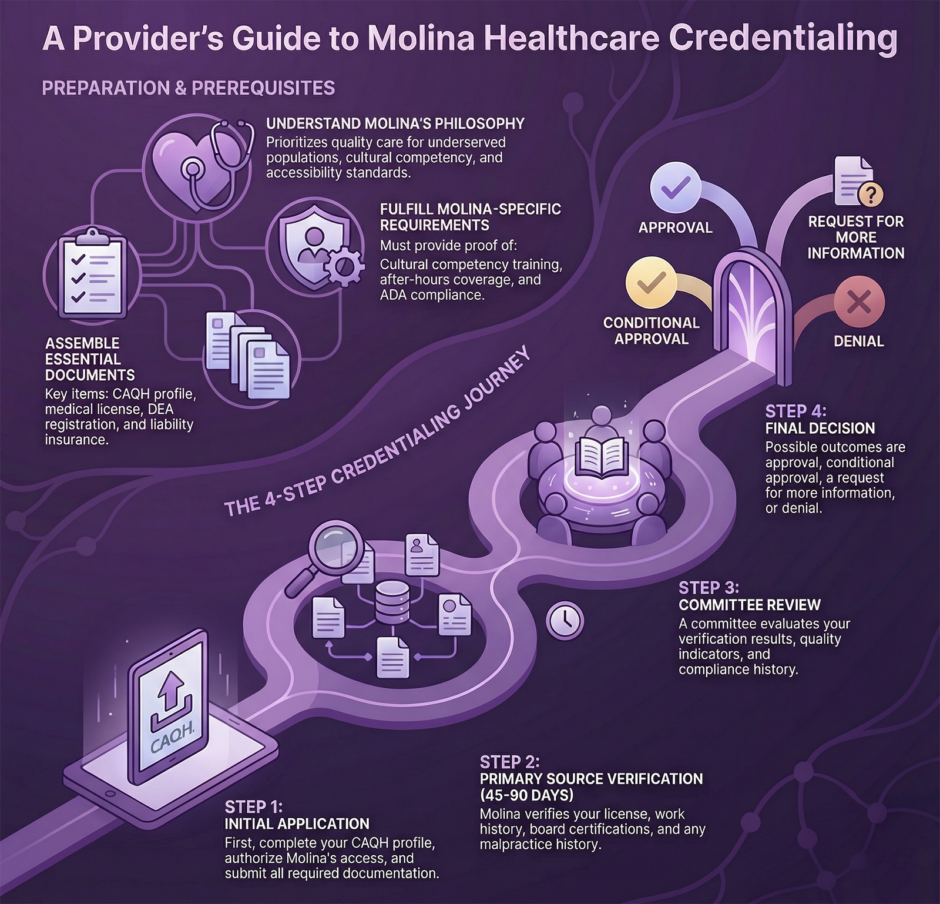
Molina’s Credentialing Philosophy
Molina Healthcare emphasizes:
- Quality care for underserved populations
- Cultural competency
- Accessibility standards
- Compliance with state Medicaid requirements
- Medicare Advantage program standards
Essential Prerequisites
Required Documentation
 Current state medical license(s)
Current state medical license(s)- DEA registration
- Board certification(s)
- Professional liability insurance
- Work history (5 years, no gaps)
- Education and training verification
- Government-issued photo ID
- CAQH ProView profile
- National Provider Identifier (NPI)
- Medicare/Medicaid numbers
- Cultural competency training certificates
- State-specific requirements
Molina-Specific Requirements
- Cultural competency training completion
- After-hours coverage arrangements
- Language capabilities documentation
- ADA compliance verification
- State-specific Medicaid requirements
The Molina Provider Portal
Getting Started
- Register on Molina’s Provider Portal
- Complete the provider profile
- Access credentialing applications
- Upload required documentation
Portal Features
- Application tracking
- Document submission
- Status updates
- Provider demographics management
- Communication tools
The Credentialing Process: Step by Step
Step 1: Initial Application
 Complete CAQH profile
Complete CAQH profile- Authorize Molina access
- Submit Molina-specific forms
- Provide supporting documentation
Step 2: Primary Source Verification
Molina verifies:
- License validity
- Education history
- Work experience
- Malpractice history
- Sanctions/exclusions
- Board certifications
- Hospital privileges
Timeline: 45-90 days typical
Step 3: Committee Review
Evaluation criteria:
- Verification results
- Quality indicators
- Compliance history
- Cultural competency
- Accessibility standards
Step 4: Final Decision
Possible outcomes:
- Approval
- Conditional approval
- Request for information
- Denial with appeal rights
Special Considerations for Molina Providers
Medicaid Requirements
 State-specific regulations
State-specific regulations- Special population needs
- Cultural competency standards
- Access requirements
- Quality measures
Medicare Advantage Participation
- Medicare enrollment verification
- Special needs population experience
- Quality reporting requirements
- Compliance training
Best Practices for Success
Documentation Management
- Digital file organization
- Expiration date tracking
- Consistent naming conventions
- Separate files by requirement
- Backup documentation
Communication Strategy
- Maintain primary contact
- Document all interactions
- Use official channels
- Regular follow-up
- Keep communication logs
Maintaining Your Credentials
Ongoing Requirements
- Regular CAQH attestation
- License renewals
- Insurance updates
- Cultural competency updates
- Quality metric reporting
Practice Updates
Report promptly:
- Location changes
- Staff changes
- Coverage arrangements
- Contact information
- Service modifications
Common Challenges and Solutions
Application Delays

If experiencing delays:
- Check portal status
- Verify CAQH attestation
- Contact provider services
- Submit missing information
- Document communication
Information Discrepancies
Resolution steps:
- Review submissions
- Update CAQH
- Submit corrections
- Follow up
- Document changes
Quality and Compliance
Quality Programs
- HEDIS measures
- Patient satisfaction
- Access standards
- Cultural competency
- Quality improvement activities
Compliance Requirements
- Medicaid/Medicare regulations
- State requirements
- Cultural competency
- Accessibility standards
- Reporting obligations
Resources and Support
Key Contacts
- Provider Services
- Credentialing Department
- Network Management
- Cultural Competency Team
- State Representatives
Online Resources
- Molina Provider Portal
- CAQH ProView
- State Medicaid websites
- Cultural competency resources
- Medicare resources
Expert Tips for Long-term Success
Time Management
- Start early (90-120 days)
- Create timeline
- Set reminders
- Plan for delays
- Regular updates
Relationship Building
- Know your provider rep
- Attend Molina workshops
- Participate in provider forums
- Stay informed of updates
- Engage in quality initiatives
Special Population Considerations
Cultural Competency
- Required training
- Language capabilities
- Cultural sensitivity
- Population needs
- Community engagement
Accessibility Standards
- Physical access
- Language access
- After-hours coverage
- Appointment availability
- Emergency protocols
Recredentialing Process
Preparation (Start 6 Months Prior)
- Document updates
- CAQH attestation
- Quality metrics review
- Compliance verification
- Training updates
Common Requirements
- Updated documentation
- Performance review
- Quality measures
- Patient satisfaction
- Compliance history
Summary: Getting Credentialed with Molina
Success with Molina Healthcare credentialing requires:
 Attention to cultural competency
Attention to cultural competency- Strong documentation
- Regular communication
- Quality focus
- Compliance adherence
Remember that serving Molina’s diverse population requires additional considerations beyond standard credentialing.
Stay focused on:
- Cultural sensitivity
- Population needs
- Access requirements
- Quality measures
- Community engagement
Keep this guide as your reference through both initial credentialing and ongoing participation in Molina’s network. Always verify current requirements through official Molina channels, as standards may change, particularly regarding state-specific Medicaid requirements.
Contact us to handle all of your Molina credentialing needs and/or challenges.


 Current state medical license(s)
Current state medical license(s) Complete CAQH profile
Complete CAQH profile State-specific regulations
State-specific regulations Attention to cultural competency
Attention to cultural competency