Medical practices are constantly looking for ways to improve efficiency and increase revenue. Yet many practices are still relying on manual, paper-based billing processes that are tedious, error-prone, and time-consuming. In today’s digital age, automated medical billing is a must for any practice that wants to streamline operations, get paid faster, reduce denied claims, and focus on patient care.

We explain what medical billing automation is, the benefits it provides, how to choose the right software, and tips for making the transition from manual to automated billing. You’ll understand why automating billing can revolutionize your practice and how to successfully implement an automated solution.
What is Medical Billing Automation?
Medical billing automation refers to software that handles the billing process electronically rather than on paper.
This includes:
- Electronically submitting insurance claims with the necessary codes and documentation directly from the medical billing software.
- Automated processes for checking claim status and following up on unpaid, underpaid, or denied claims.
- Built-in workflows that determine correct coding and insurance eligibility.
- Automated patient statements, insurance appeals, and secondary claims.
- Analytics dashboards that provide insights into revenue cycles, top procedures, common denial reasons, and other key metrics.
Automated solutions can completely eliminate paper claim submissions. Billing staff use the software to enter patient encounter details, diagnoses, procedures performed, charges, and required codes. The software checks the data for accuracy, determines the correct forms and codes, and then electronically submits the claim to the appropriate payer.
This removes the need for staff to manually fill out claim forms, submit claims by paper or EDI, track status, and follow-up on rejected claims. The software handles these repetitive administrative tasks in the background according to configurable rules and workflows.
Key Benefits of Medical Billing Automation
Transitioning from manual to automated medical billing delivers significant benefits:
- Increased collections and revenue
Automation improves clean claim rates by reducing human errors in coding and form completion. Real-time claim edits and scrubbing find errors for correction before submission. This results in fewer denied claims and faster payments. Improved workflows also reduce billing delays. Automation ensures claims are submitted promptly after patient visits while follow-up is handled automatically. This increases collection rates and speeds up payment cycles. - Reduced claim submission costs
Manually preparing, printing, and mailing paper claims is eliminated. Staff no longer have to repeatedly submit corrections or resubmit denied claims. Electronic submission is faster and lowers the cost per claim. - Improved staff productivity
Automation handles repetitive administrative tasks like verifying eligibility, coding claims, researching payer requirements, and follow-up. This reduces manual data entry and paperwork, freeing up staff for more value-added tasks. - Better analytics and reporting
Automated systems capture extensive billing data and generate reports on metrics like collections, denials, delays, patient balances, and more. This provides transparency into the health of the revenue cycle and helps identify issues for correction. - Reduced claim errors and denials
Billing automation minimizes human error by auto-populating fields, determining correct codes and modifiers, and identifying missing information. This improves accuracy and completeness for cleaner claim submission. Errors are caught earlier and easily fixed. - Streamlined workflows
Automated rules and workflows standardize processes for staff. Back-end automation handles routine administrative tasks like claim submission, status checks, and follow up based on rules. This simplifies billing operations. - Improved regulatory compliance
Automation periodically and automatically checks for payer rule changes, new industry regulations, and updated code sets. This ensures submitted claims are compliant with the latest requirements. - Enhanced patient satisfaction
Accurate clean claims and faster reimbursements improve practice cash flow. This enables investments in better patient experiences and the latest medical equipment. Automated patient statements also clearly communicate balances owed.
How to Select the Right Medical Billing Automation Software
With the benefits clear, the next step is choosing the right automation solution for your practice.
Consider the following when evaluating medical billing software:
- Integrations – The system should integrate with your practice management and EHR software for seamless workflow and data sharing. APIs make integration easier.
- Cloud-based – Cloud-based systems enable access from any device or location. They also reduce IT overhead related to servers and maintenance.
- Automation capabilities – Ensure the software handles essential billing tasks like coding, submission, follow-up, denials, appeals, analytics, and reporting. The more it automates, the better.
- Rule-based workflows – Configurable rules and workflows simplify billing processes and ensure consistency. For example, automatically submit secondary claims after the primary payer reimburses.
- Claim scrubbing – Look for built-in scrubbing to catch and correct errors like invalid codes before claim submission. This improves clean claim rates.
- Payer specific rules – The system should automatically check for payer rule changes and update billing workflows accordingly. This reduces rejections.
- Analytics – Robust reporting is crucial for gaining insights into your revenue cycle. Ensure the software delivers visual dashboards and custom reports on key metrics.
- Scalability – As your practice grows, the system should easily scale up in terms of workflows, features, and number of claims processed. Leverage the cloud.
- Implementation and support – Vendor offerings like set-up assistance, training, customer support, and consulting services ensure a smooth implementation and transition.
- Security compliance – The software should be HIPAA compliant to protect sensitive patient data through encryption, access controls, audits, backups, and other safeguards.
Following these criteria helps narrow down the medical billing automation solution that best fits your practice’s needs and budget.
Transitioning from Manual to Automated Billing
Once you’ve selected the right software platform, focus on ensuring a smooth transition from paper-based processes to digital workflows:
- Phase out paper – Set a cutover date after which staff must use the automated system rather than paper claim forms. This forces adoption of the new technology. Send out notifications to patients about the new digital processes.
- Configure workflows – Work with your vendor to configure rules, templates, automated follow ups, status checks, and other workflows that mirror your current manual processes. The software should adapt to your procedures rather than the other way around.
- Clean up existing claims – Before switching systems, ensure all outstanding and in-progress claims are entered or migrated into the automated system so nothing falls through the cracks.
- Validate integrations – If integrating with EHR or practice management software, thoroughly test the integrations. Confirm clean handoffs of demographic, treatment, coding, and billing data between systems.
- Train staff – Provide sufficient training and resources to help billing staff learn the new workflows. Make sure everyone is comfortable with the system before going live. Behavior change is crucial.
- Monitor adoption – Track how often staff use the automated system versus old paper processes after go-live. Quickly identify and address gaps in adoption.
- Refine workflows – Continuously gather staff feedback on how to streamline workflows. Work with your vendor to tweak rules and enhance automation. Optimization is ongoing.
- Watch metrics – As automation takes effect, closely monitor KPIs like first-pass claims acceptance, denial rates, days in A/R, and collections. Leverage built-in analytics.
Following best practices for the transition and maintaining open communication with staff ensures a smooth adoption of automated systems. Expect a period of adjustment as workflows are optimized.
Medical Billing Automation Tips and Tricks
Beyond software selection and implementation, follow these tips and tricks for getting the most from medical billing automation:
- Set rules to automatically submit secondary claims once the primary payer has paid. This efficiently captures maximum reimbursement.
- Use eligibility checks to reduce claim rejection rates and avoid unnecessary claim submissions that will be denied.
- Automate patient statements to go out at set intervals. This improves collections from patients responsible for a share of costs.
- Ensure systems are continually updated with the latest code changes and payer rules. Sign up for update alerts from payers or enable automated code updates.
- Develop a standard process for appealing denied claims with necessary documentation and follow-up built-in. Automated appeals save significant time.
- Download and scrutinize payer reimbursement reports to identify areas for workflow improvement. Every denied claim represents lost revenue.
- Use analytics reports to identify peak submission periods and error-prone claim types. Address them proactively to smooth out submission volume and boost acceptance rates.
- Route claims on hold or needing additional info to designated staff for faster turnaround. Automated reminders can prompt completion so claims get submitted faster.
- Integrate automated patient statements with the billing system. Customizable text and branding options project a professional image.
- Automate follow-ups like sending three claim status requests before marking a claim denied. Saves staff time on routine admin work.
Leveraging small optimizations like these maximizes the impact of billing automation. Consistently look for ways to improve workflows over time as reimbursement patterns evolve.
Case Studies: Successful Medical Billing Automation
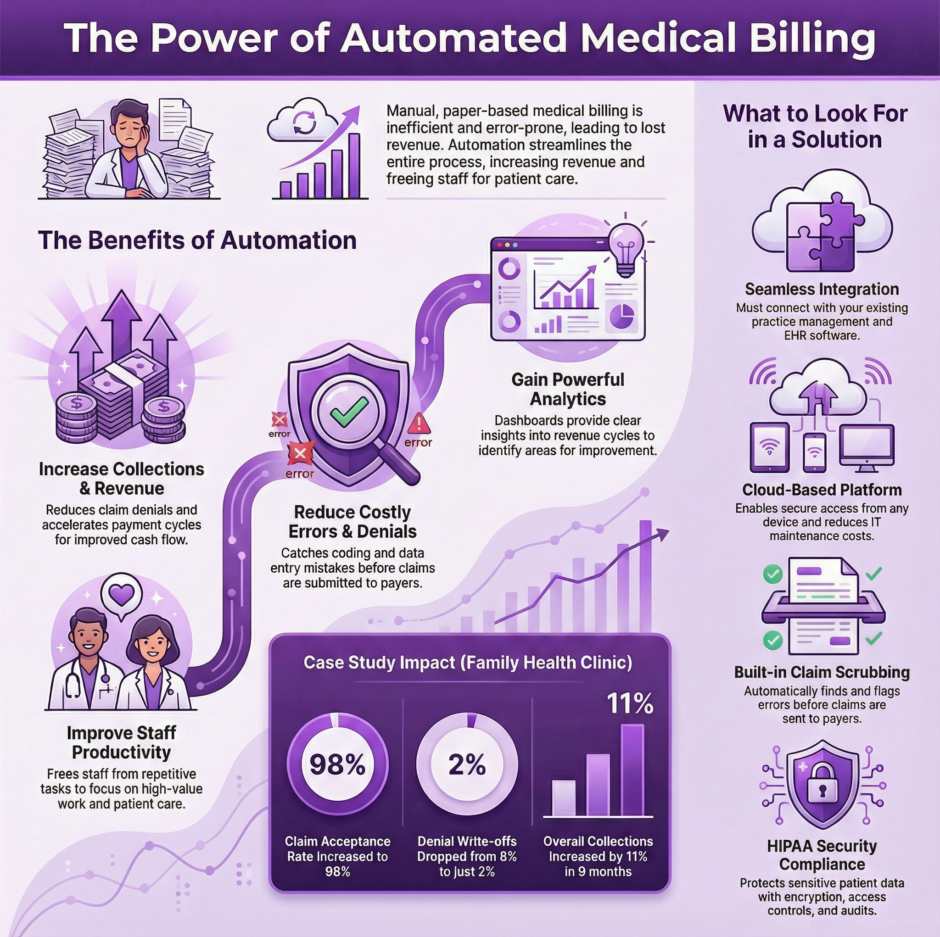
Many practices have already embraced automated solutions and seen tremendous results.
Here are a few examples:
Family Health Clinic
This 7-provider primary care clinic still used a paper-based process for billing their 12,000 patients. Denials were frequent, follow-up was lax, and payments could take 3-4 months to arrive.
By implementing an integrated EHR and billing automation system, they were able to completely remove paper claims. Eligibility verification, coding, rule-based submission, and automated follow-ups handled routine administrative work, freeing up 2.5 full-time staff for more value-added tasks.
Claim acceptance increased to 98% while denial write-offs fell from 8% to just 2% of claims. Days in accounts receivable dropped from 96 to 72. Overall, collections increased by 11% within 9 months after going live on the new system.
Orthopedic Surgical Center
This single-specialty practice struggled with a crippling denial rate of 18% that stemmed from improper coding and frequent submission errors. Their manual process couldn’t keep up.
After automated systems were implemented, denials decreased to 5% within 3 months. Coders were more efficiently utilized to tackle complex cases while managers had transparency into revenue cycles. Cleaner claims combined with automated secondary payer billing increased collections by 7% year-over-year.
Neurology Associates
As the practice rapidly expanded to 9 providers at 3 locations, their paper-based billing process began breaking down. Claims took too long to submit and get paid, patient statements were often delayed, and staff became overwhelmed.
By optimizing their use of automation tools already integrated with their EHR system, policy and demographic eligibility checks were added, standardized follow-ups were configured, and analytics tracked denial reasons. This supported growth without additional headcount while reducing DSO by 8 days.
Summary: Automation in Billing is Here to Stay
The benefits of transitioning from manual medical billing processes to automated systems are clear: faster payment cycles, reduced denied claims, improved staff productivity, and higher revenue.
Cloud-based automation handles repetitive administrative tasks in the background while giving practices transparency into the health of the revenue cycle. Integrations with EHR and practice management systems create seamless end-to-end workflows.
Careful software selection, staff training, configuration of rules-based workflows, and ongoing performance monitoring are crucial to a successful implementation. Over time, processes can be further optimized through analytics insights and automation.
Manual medical billing costs valuable time and money. Taking the right steps to automate billing and revenue cycle management enables practices to reduce administrative burden, improve payments, and focus where it matters most, delivering better patient care.

