
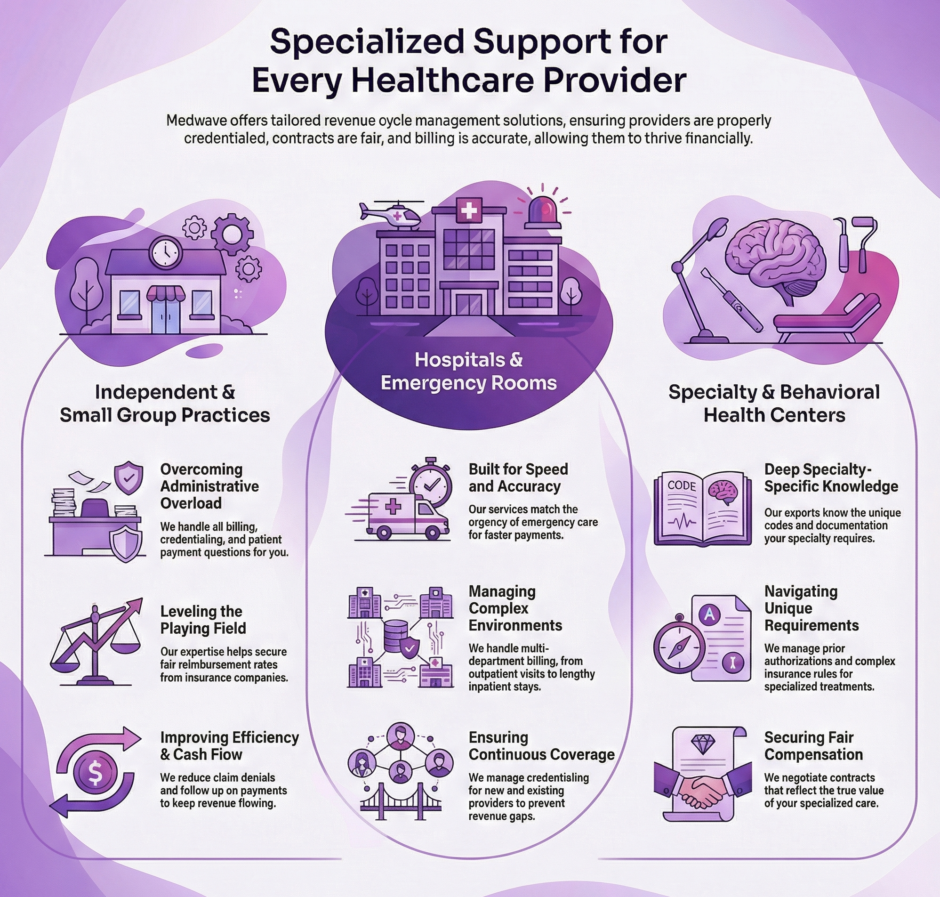
At Medwave, we know that healthcare providers come in all shapes and sizes. Our team specializes in providing services for a wide variety of healthcare settings. We’ve built our services to fit the specific needs of each type of provider, because we know that what works for a solo practitioner won’t necessarily work for a busy emergency room.
The truth is, medical billing involves careful attention to coding accuracy, staying current with insurance requirements, making sure your practice is properly credentialed with insurance networks, and negotiating fair contracts with payers. When these pieces don’t work together smoothly, providers lose money and waste time chasing down payments instead of focusing on patient care.
We’ve worked with thousands of healthcare providers across different specialties and practice sizes. Through that experience, we’ve learned what each type of provider needs to maintain healthy revenue cycles and strong relationships with insurance companies. Let’s take a closer look at the healthcare professionals and facilities we serve, and how our billing, credentialing, and payer contracting services make their lives easier.
Clinics: Building Strong Foundations for Patient Care
Clinics serve as the backbone of community healthcare. Whether you’re running a family medicine clinic, an urgent care center, or a specialty clinic, you’re juggling patient appointments, staff management, supply ordering, and countless other responsibilities. Medical billing shouldn’t be adding to your stress.
We support clinics with complete billing services that cover everything from claim submission to payment posting. Our credentialing services make sure your providers are enrolled with all the right insurance networks, opening the door to more patients. We also handle coding to ensure every service is documented correctly, which means fewer claim denials and faster reimbursements.
One of the biggest challenges clinics face is dealing with the constant changes in insurance policies and coding requirements. What was acceptable six months ago might get denied today. Our team stays on top of these changes so you don’t have to. We also work on payer contracting to secure fair reimbursement rates for your services, which directly impacts your clinic’s financial health.
Emergency Rooms: Speed and Accuracy When It Matters Most
Emergency rooms operate in a unique environment where every second counts. Patients arrive in crisis, treatment happens rapidly, and documentation must be thorough despite the pressure. The billing that follows needs to match that same level of urgency and precision.
Our RCM services for emergency rooms are designed with speed in mind. We know that delayed billing means delayed payment, which can create cash flow problems for your facility. Our team processes claims quickly without sacrificing accuracy, because we recognize that emergency care involves detailed coding requirements and often requires extensive documentation to justify the level of service provided.
Emergency departments also deal with a high percentage of uninsured patients and cases that require charity care or payment assistance programs. We help identify which patients qualify for these programs and ensure the proper processes are followed. Our credentialing services keep your emergency physicians enrolled across multiple insurance networks, which is especially important in settings where patients don’t choose their provider.
The high-pressure nature of emergency medicine means your staff doesn’t have time to follow up on denied claims or track down missing information from insurance companies. That’s exactly the kind of work we handle, freeing your team to focus on saving lives rather than fighting with insurance paperwork.
Hospitals: Managing Multiple Moving Parts
Hospitals represent some of the most challenging billing environments in healthcare. You’re dealing with multiple departments, hundreds of procedures, various insurance plans, and patients who may be admitted, observed, or treated in outpatient settings. Each of these situations requires different billing approaches.
We provide custom billing solutions designed specifically for hospital environments. Our team knows how to handle everything from simple outpatient visits to lengthy inpatient stays with multiple procedures. We work with your existing systems to ensure smooth data flow and accurate claim submission.
Credentialing is particularly important for hospitals because you’re likely bringing on new providers regularly. We manage the entire credentialing process, which can take months if not handled properly. Our expertise helps speed up the timeline so new doctors can start seeing patients and generating revenue sooner.
Payer contracting is another critical area where we help hospitals. The rates you negotiate with insurance companies directly affect your bottom line. We bring experience and data to these negotiations, working to secure contracts that fairly compensate you for the services you provide.
Hospital billing also involves intricate charge capture processes, where services performed need to be accurately recorded and billed. Missing charges mean lost revenue. Our systems and processes help ensure that nothing falls through the cracks, from medications to procedures to ancillary services.
Solo Practitioners: Freedom to Focus on Medicine
Solo practitioners chose independence for a reason. You want to practice medicine your way, build personal relationships with patients, and maintain control over your practice. But running a business by yourself means wearing many hats, and medical billing is often the hat that fits most uncomfortably.
We help independent practitioners by taking complete ownership of their billing needs. From the moment a patient checks in until the payment is posted to your account, we handle every step. This includes verifying insurance eligibility, submitting claims, following up on denials, posting payments, and managing patient billing questions.
For solo practitioners, credentialing can be particularly challenging because you don’t have administrative staff to manage the paperwork. Insurance companies require extensive documentation, and keeping track of renewal dates and requirements for multiple networks quickly becomes overwhelming. We manage all of this for you, ensuring your credentials never lapse and you maintain access to all your insurance panels.
Payer contracting is another area where solo practitioners often struggle. Insurance companies know that individual doctors have less negotiating power than large groups. We help level the playing field by bringing expertise to contract negotiations and helping you secure fair rates for your services.
Many solo practitioners tell us that our services feel like having a complete billing department without the overhead costs of hiring full-time staff. You get expertise, technology, and dedicated support without the expense of salaries, benefits, and office space.
Private Practices: Improving Efficiency and Cash Flow
Private practices sit in a sweet spot between solo practitioners and large group practices. You might have a few partners, several employed providers, and a small administrative staff. You’re large enough to have some infrastructure but small enough that efficiency really matters.
We offer tailored billing and coding solutions that fit the size and needs of private practices. Our services scale with your practice, so as you add providers or expand services, your billing support grows accordingly. We focus on two key areas that make the biggest difference for private practices: efficiency and cash flow.
Efficiency means getting claims submitted quickly and correctly the first time. Every claim that gets denied or requires additional information costs time and money to fix. Our coding expertise and quality checks reduce the number of problematic claims, which means faster payment and less rework.
Cash flow is the lifeblood of any private practice. You have payroll to meet, rent to pay, and supplies to order. When insurance payments are delayed or denied, it creates financial stress. Our team works diligently to keep money flowing into your practice by submitting clean claims, following up promptly on outstanding payments, and managing patient balances.
We also handle credentialing for all your providers, which is particularly important when you’re adding new doctors or physician assistants. Having someone dedicated to managing this process means your new providers can start seeing insured patients much faster.
Group Practices: Coordination Across Multiple Providers
Group practices bring together multiple physicians, often across different specialties. This creates excellent patient care opportunities but also creates billing challenges. How do you manage billing for several providers, each with their own patient panels, schedules, and documentation styles?
Our streamlined RCM services for group practices handle multiple providers while ensuring smooth operations. We work with your practice management system to capture charges from all your providers, code them correctly, and submit claims efficiently. We also track productivity and revenue by provider, giving you the data you need to make informed business decisions.
Credentialing becomes more demanding in group settings because you need to track credentials for every provider across multiple insurance networks. We maintain a complete credential tracking system, monitoring expiration dates and renewal requirements so nothing slips through the cracks.
Group practices often have more leverage in payer contract negotiations than solo practitioners, but you still need expertise to maximize that leverage. We bring data and negotiating experience to help your practice secure favorable contract terms with insurance companies.
Another advantage we offer group practices is consistency. When you handle billing internally with multiple staff members, you often end up with inconsistent processes and uneven results. Our standardized approach ensures every claim is handled the same way, regardless of which provider saw the patient.
Specialty Centers: Expert Knowledge for Specialized Care
Specialty centers focus on specific areas of medicine like pain management, neurology, cardiology, orthopedics, or gastroenterology. Each specialty has unique billing requirements, specific codes, and particular documentation needs that general billing knowledge doesn’t cover.
We bring expertise in billing for specialty centers across various medical fields. Our team includes specialists who know the specific codes, modifiers, and documentation requirements for your area of medicine. This expertise translates directly into higher clean claim rates and better reimbursement.
Pain management, for example, involves specific documentation requirements for procedures and ongoing justification for certain treatments. Neurology billing requires knowledge of diagnostic testing codes and chronic disease management. Cardiology involves everything from office consultations to invasive procedures, each with distinct billing rules.
We also recognize that specialty centers often use specific equipment and provide procedures that require prior authorization from insurance companies. We manage the prior authorization process, tracking requirements and submitting necessary documentation to secure approval before services are provided.
Credentialing for specialty centers requires documentation of board certifications, specialized training, and facility privileges. We manage all these requirements, working with both insurance companies and facilities to maintain your providers’ credentials.
Payer contracting for specialty services requires particular attention because reimbursement rates can vary widely between different insurance companies and different procedures. We help negotiate contracts that fairly compensate you for the specialized care you provide.
Behavioral Health Facilities: Meeting Unique Requirements
Behavioral health facilities provide critical services for mental health and substance abuse treatment. These facilities face unique billing challenges that require specialized knowledge and careful attention to detail.
Mental health parity laws require insurance companies to cover mental health and substance abuse services similarly to physical health services, but making sure these laws are properly applied often requires persistence and expertise. We help behavioral health facilities get the reimbursement they deserve for the vital services they provide.
Coding for behavioral health services involves specific procedure codes and diagnosis codes that differ from other medical specialties. Our team knows these codes and the documentation required to support them. We also manage the authorization requirements that many insurance companies impose for behavioral health services.
Credentialing for behavioral health providers involves verifying licenses, certifications, and sometimes facility accreditations. We handle all aspects of this process, ensuring your counselors, therapists, psychologists, and psychiatrists are properly enrolled with insurance networks.
Many behavioral health services require ongoing authorization as treatment continues. We track these authorization periods and submit renewal requests before current authorizations expire, preventing gaps in coverage that could interrupt patient care or delay payment.
Substance abuse treatment, in particular, often involves working through specific insurance requirements and benefit limits. We work with insurance companies to maximize covered benefits for your patients while ensuring your facility receives appropriate payment for services provided.
Summary: Who Benefits from Our Credentialing, Contracting, and Billing Services?
 At Medwave, we’ve built our business around one simple idea: healthcare providers should spend their time caring for patients, not fighting with insurance companies. Whether you’re a solo practitioner seeing patients in a small office or part of a large medical facility, our services are designed to make your life easier and your practice more profitable.
At Medwave, we’ve built our business around one simple idea: healthcare providers should spend their time caring for patients, not fighting with insurance companies. Whether you’re a solo practitioner seeing patients in a small office or part of a large medical facility, our services are designed to make your life easier and your practice more profitable.
We’ve seen firsthand how proper credentialing, payer contracting, and billing can transform a struggling practice into a thriving one. When claims are submitted correctly, payments arrive faster. When providers are credentialed with the right networks, more patients have access to care. When payer contracts are negotiated fairly, practices earn what they deserve for their services.
Every healthcare provider faces unique challenges based on their specialty, practice size, and patient population. That’s why we don’t offer a one-size-fits-all solution. Instead, we take time to learn about your specific situation and customize our services to meet your needs. Whether you need complete revenue cycle management or support in specific areas like credentialing or payer contracting, we’re here to help.
If you’re tired of dealing with claim denials, frustrated with slow payments, or simply overwhelmed by the administrative burden of running a practice, we’d love to talk with you. Our team has helped hundreds of providers improve their revenue cycles and reduce stress.
