You’ve completed medical school, finished your residency, obtained your license, and you’re ready to practice medicine. But if you want to treat patients in a hospital setting, there’s one more crucial step, obtaining hospital privileges. This process determines exactly what you can and cannot do within a hospital’s walls, and it’s separate from both your medical license and your insurance credentialing.
 Hospital privileging affects every physician who wants to admit patients, perform procedures, or practice in a hospital environment. Whether you’re a surgeon planning to operate, an internist who wants to round on hospitalized patients, or a specialist providing consultations, you’ll need to go through the privileging process. Let’s break down what hospital privileging really means and how it works.
Hospital privileging affects every physician who wants to admit patients, perform procedures, or practice in a hospital environment. Whether you’re a surgeon planning to operate, an internist who wants to round on hospitalized patients, or a specialist providing consultations, you’ll need to go through the privileging process. Let’s break down what hospital privileging really means and how it works.
What Hospital Privileges Actually Are
Think of hospital privileges as your permission slip to practice medicine in a specific hospital. Your medical license says you’re qualified to practice medicine in your state. Hospital privileges say you’re approved to practice specific types of medicine within that particular hospital’s facility.
Privileges are not one-size-fits-all. They’re tailored to your training, experience, and specialty. A cardiologist receives different privileges than an orthopedic surgeon. An experienced physician who’s performed thousands of procedures gets broader privileges than someone fresh out of residency. The hospital grants you permission to perform only those procedures and services that you’re qualified to provide based on your documented training and experience.
Hospitals grant privileges for several important reasons. First and foremost, they’re legally responsible for the quality of care provided within their facilities. If they allow an unqualified or incompetent physician to practice, they face liability for any harm that results. Privileging helps hospitals ensure that only qualified professionals provide care to their patients.
Secondly, hospitals must meet accreditation standards from organizations like The Joint Commission. These accrediting bodies require hospitals to have rigorous credentialing and privileging processes. Without proper accreditation, hospitals lose their ability to receive Medicare payments and face other serious consequences.
Thirdly, privileging protects patients. It ensures that the surgeon operating on you has actually performed that type of surgery before. It verifies that the doctor admitting your elderly parent to the hospital has appropriate training in geriatric medicine. It confirms that the physician reading your imaging studies knows how to interpret those scans accurately.
The Difference Between Credentialing and Privileging
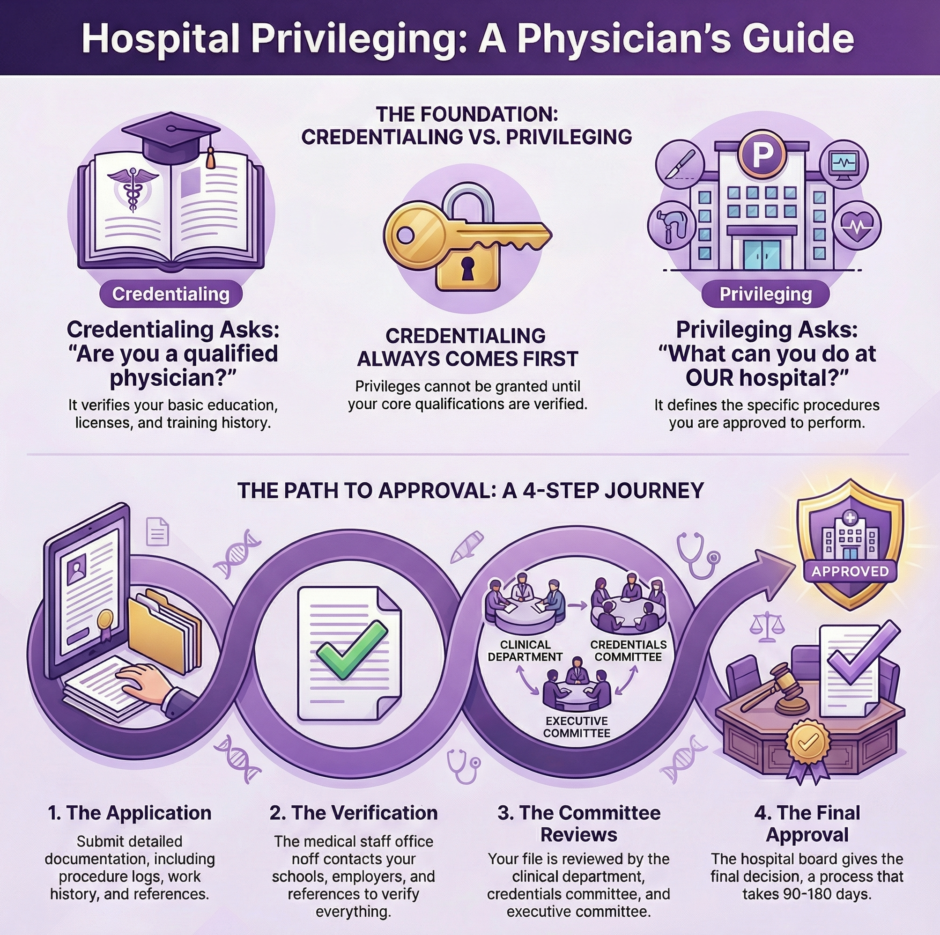
Many people confuse credentialing with privileging, but they’re distinct processes that serve different purposes. Credentialing verifies your basic qualifications. Your medical school education, your residency training, your board certifications, your licenses, and your professional history. It answers the question: “Is this person a qualified physician?”
Privileging goes deeper and more specific. It examines exactly what procedures and services you’re trained and experienced to perform. It answers the question: “What is this physician qualified to do in our hospital?” You might be credentialed as a general surgeon, but your specific privileges determine whether you can perform gallbladder removals, hernia repairs, or trauma surgeries.
Credentialing typically happens first and forms the foundation for privileging decisions. A hospital can’t grant you privileges without first completing credentialing to verify you’re a legitimate, licensed healthcare provider. Once credentialing establishes your basic qualifications, privileging defines the scope of what you can actually do.
Types of Hospital Privileges
Hospitals grant several different categories of privileges, depending on your specialty, experience, and the hospital’s needs.
Active staff privileges represent the most common type. These allow you to admit patients, perform procedures, and practice within your specialty area. Physicians with active staff privileges typically have regular hospital duties and maintain a consistent presence at the facility.
Courtesy privileges provide limited access for physicians who primarily practice elsewhere but occasionally need hospital services for their patients. For example, a physician whose main practice is at Hospital A might have courtesy privileges at Hospital B to admit patients who live closer to that facility. Courtesy privileges usually come with fewer responsibilities and less voting power in hospital affairs.
Consulting privileges allow specialists to provide expert opinions and recommendations for hospitalized patients but not to admit patients independently. A cardiologist might have consulting privileges to evaluate patients’ heart conditions and advise the admitting physician on treatment plans.
Temporary privileges apply in emergency situations or when a hospital needs specialized expertise not available among current staff. These short-term privileges allow qualified physicians to practice for a limited time while full credentialing and privileging processes proceed.
Telehealth privileges have become increasingly important, allowing physicians to provide remote consultations, interpret imaging studies, or monitor patients from a distance. These privileges come with specific requirements about technology, communication, and documentation.
The Privileging Application Process
 Applying for hospital privileges involves extensive paperwork and verification, often more detailed than insurance credentialing. You’ll need to provide comprehensive documentation of your qualifications and experience.
Applying for hospital privileges involves extensive paperwork and verification, often more detailed than insurance credentialing. You’ll need to provide comprehensive documentation of your qualifications and experience.
The application typically requires your complete educational history, including undergraduate education, medical school, internship, residency, and any fellowship training. You’ll need to document every place you’ve trained and provide contact information so the hospital can verify your education directly with those institutions.
Your work history must be detailed and continuous. Any gaps in employment require explanation. The hospital wants to see where you’ve practiced, what procedures you’ve performed, and your volume of clinical activity. If you haven’t worked for six months due to personal reasons, you’ll need to explain that gap and possibly provide evidence of continued clinical competence.
Procedure logs become especially important for privileging. Unlike credentialing, which might accept general statements about your training, privileging requires specific numbers. How many appendectomies have you performed? How many colonoscopies? How many cardiac catheterizations? You’ll need to document your experience with actual case numbers, often separated by whether you performed the procedure independently or under supervision.
References carry significant weight in privileging decisions. You’ll typically need letters from physicians who have directly observed your clinical work. These references should speak to your technical skills, clinical judgment, communication abilities, and professional conduct. Generic letters of recommendation don’t help much, hospitals want specific observations about your practice patterns and competence.
Your professional liability history gets examined closely. Every malpractice claim, settlement, or judgment must be disclosed and explained. Even if a case was dismissed or settled without admission of fault, the hospital’s credentialing committee will want to know the details. Hiding malpractice history is grounds for automatic denial and can result in reports to the National Practitioner Data Bank.
The Review and Approval Process
Once you submit your application for hospital privileges, a thorough review process begins that operates largely behind the scenes. The hospital’s medical staff office takes the lead in collecting and verifying every piece of information you provided. This includes contacting your medical school to confirm graduation, checking with your residency program to verify completed training, calling your references to discuss your qualifications, and querying the National Practitioner Data Bank for any disciplinary actions or malpractice payments.
Your verified application then moves through several layers of review within the hospital’s organizational structure. The relevant clinical department examines your qualifications in detail. For example, if you’re applying for surgical privileges, the surgery department will conduct this review. The department chair and senior physicians analyze your training and experience to determine what specific privileges you should receive. Many hospitals use a privilege delineation list, which serves as a detailed checklist of specific procedures and services within each specialty. You request the privileges you want, and the department evaluates whether your training and experience support each request. It’s important to understand that you might receive approval for some requested privileges but not others, depending on your documented experience.
The credentials committee adds another critical layer of oversight. This multi-disciplinary committee examines applications from all specialties and ensures consistent standards are applied across the hospital. They actively look for red flags such as unexplained gaps in work history, concerning patterns in malpractice claims, or previous disciplinary actions. After this review, your application advances to the hospital’s medical executive committee and ultimately to the hospital board of directors for final approval. Even highly qualified physicians can face denial at this stage based on institutional needs, if the hospital already has sufficient specialists in your area, they might decline your application regardless of your impressive qualifications.
Key Points to Remember:
- The entire privileging process typically takes 90 to 180 days, though it can extend longer if verification problems arise or committee meetings experience delays.
- During this waiting period, you cannot practice at the hospital even if you hold a valid medical license and have been credentialed with insurance companies.
- The process involves multiple verification steps including medical school confirmation, residency program verification, reference checks, and National Practitioner Data Bank queries.
- Your application undergoes review at multiple levels: the relevant clinical department, the credentials committee, the medical executive committee, and finally the board of directors.
- Privilege approval is not all-or-nothing, you may receive some requested privileges while being denied others based on your specific experience and training documentation.
- Final approval can be influenced by factors beyond your qualifications, including the hospital’s current staffing needs and strategic priorities.
Maintaining and Renewing Privileges
 Receiving privileges isn’t the end of the story. Hospitals continuously monitor physicians’ performance and require periodic renewal, typically every two years.
Receiving privileges isn’t the end of the story. Hospitals continuously monitor physicians’ performance and require periodic renewal, typically every two years.
Ongoing Professional Practice Evaluation (OPPE) means the hospital tracks your clinical activities, outcomes, and any quality issues. They monitor metrics like infection rates after your surgeries, complication rates, patient satisfaction scores, and how well you document in medical records. If patterns of concern emerge, the hospital may investigate further or modify your privileges.
Focused Professional Practice Evaluation (FPPE) occurs when you first join the medical staff, when you request new privileges, or when quality concerns arise. During FPPE, the hospital closely monitors specific aspects of your practice, often requiring another physician to review your cases and observe your work.
When your privileges come up for renewal, you’ll need to reapply and provide updated information about your continued practice. You’ll document the procedures you’ve performed since your last approval, any new training or certifications you’ve obtained, and updates to your professional liability history. You’ll also need to show completion of required continuing medical education.
Many hospitals require minimum volume thresholds to maintain certain privileges. If you requested privileges to perform coronary angioplasty but you’ve only done two cases in the past two years, the hospital might remove that privilege due to lack of current experience. The logic is simple: skills deteriorate without regular practice, so privileges should reflect your current activity level, not just past training.
Common Privileging Challenges
Physicians face various obstacles during the privileging process. New graduates often struggle to obtain full privileges because they lack extensive independent experience. Many of their cases during residency were performed under supervision, which hospitals might not count fully toward required case numbers. Some hospitals offer proctored privileges where new physicians practice under observation until they demonstrate competence.
Physicians changing locations face barriers when they’ve been away from certain procedures. If you spent five years in an administrative role and now want to return to clinical practice, hospitals will question whether your skills remain current. You might need to complete additional training or accept limited privileges initially.
Gaps in malpractice insurance create significant problems. If your insurance lapsed at any point, even briefly, hospitals may have concerns. Some states require you to report any period without coverage, and hospitals may view gaps as red flags about your practice history.
Out-of-state physicians seeking privileges in new locations must navigate different state requirements. Your privileges from a hospital in California don’t automatically transfer to a hospital in Texas. You’ll go through the entire process again, though your previous privileging history should support your new application.
Telemedicine privileges present unique challenges because you might be licensed in one state but providing care to patients in another. Hospitals must determine how to credential and privilege physicians who never physically enter their building but still provide care to their patients.
Special Situations and Considerations
 Some medical specialties face unique privileging considerations. Surgeons must document specific procedures they can perform, with privileges often divided into categories like general surgery, minimally invasive surgery, trauma surgery, or surgical oncology. A general surgeon might not automatically receive privileges for advanced laparoscopic procedures without specific training.
Some medical specialties face unique privileging considerations. Surgeons must document specific procedures they can perform, with privileges often divided into categories like general surgery, minimally invasive surgery, trauma surgery, or surgical oncology. A general surgeon might not automatically receive privileges for advanced laparoscopic procedures without specific training.
Emergency medicine physicians typically receive broad privileges to treat any patient who arrives in the emergency department, but their privileges usually don’t extend to admitting patients or following them beyond the initial emergency evaluation.
Hospitalists have reshaped privileging in many facilities. These physicians specialize in caring for hospitalized patients, and they often receive broad internal medicine privileges to manage various conditions. Their privileges might include procedures like central line placement or lumbar punctures.
Advanced practice providers including nurse practitioners and physician assistants also require privileging, though the process differs from physician privileging. Many hospitals credential and privilege these professionals in collaboration with supervising physicians, with specific protocols defining their scope of practice.
The Legal Side of Privileging
Hospital privileging carries legal implications for both hospitals and physicians. Hospitals have substantial discretion in granting or denying privileges, and their decisions receive significant legal protection. Courts generally defer to hospitals’ medical staff decisions unless there’s evidence of discrimination or violation of due process.
However, hospitals must follow their own bylaws and provide fair procedures. If their rules require giving physicians notice before denying privileges, they must do so. If bylaws provide for an appeal process, hospitals must honor that right. Physicians who believe they were unfairly denied privileges can request a hearing, though these processes are lengthy and don’t guarantee success.
Discrimination laws protect physicians from privilege decisions based on race, gender, age, or disability. If a hospital denies your application and you believe discrimination played a role, you may have legal recourse. However, proving discrimination in privileging cases is difficult because hospitals have many legitimate reasons to deny or limit privileges.
Economic credentialing (denying privileges based on business considerations rather than quality concerns) remains controversial. If a hospital denies you privileges simply because you’d compete with existing physicians who generate revenue for the hospital, that raises ethical and potentially legal questions.
Making the Process Work for You

Given the substantial time and effort required for the privileging process, taking a strategic approach can significantly improve your chances of success. Before submitting applications, invest time in researching each hospital’s needs and assessing your competition. If a facility already has abundant coverage in your specialty, they may not need additional providers. Conversely, hospitals in underserved areas or those experiencing specialty shortages often welcome new applicants and may expedite the review process.
Thorough organization of your documentation before starting applications can streamline the entire process. Create a comprehensive file containing copies of all your diplomas, certificates, licenses, and training records. Maintain a detailed log of procedures you’ve performed, including dates, supervising physicians, and outcomes. Keeping this information current ensures it’s ready whenever you need to apply for privileges or handle renewals, preventing last-minute scrambling for documentation.
Building relationships with physicians already on staff at your target hospitals can substantially strengthen your application. Their support and willingness to serve as references carries considerable weight with decision-makers. You can develop these connections by attending hospital medical staff meetings as a guest, participating in continuing education offerings at the facility, or collaborating on patient care when opportunities arise.
Strategic Planning Checklist:
- Research hospital needs and assess specialty saturation before applying to avoid wasting time on applications unlikely to succeed.
- Target underserved areas or hospitals with documented shortages in your specialty for better acceptance odds.
- Organize all credentials, certificates, licenses, and training documentation in advance and keep them continuously updated.
- Maintain a detailed procedure log with dates, supervising physicians, and outcomes to demonstrate your experience clearly.
- Cultivate relationships with staff physicians at target hospitals through guest attendance at meetings, continuing education participation, or patient care collaboration.
- Always provide complete honesty in applications, as verification processes are thorough and dishonesty can permanently damage your career.
- If you have problematic background issues, address them proactively with clear explanations rather than attempting concealment.
Summary: Hospital Privileging for Healthcare Providers
 Hospital privileging determines what medical services you can provide within a specific facility. Unlike your medical license or insurance credentialing, privileges are specific to each hospital and tailored to your documented training and experience. The process involves extensive application, verification, and committee review, typically taking several months to complete.
Hospital privileging determines what medical services you can provide within a specific facility. Unlike your medical license or insurance credentialing, privileges are specific to each hospital and tailored to your documented training and experience. The process involves extensive application, verification, and committee review, typically taking several months to complete.
Privileges come in various types including active staff, courtesy, consulting, and temporary arrangements. The approval process examines your education, training, procedure experience, references, and professional history in detail. Once granted, privileges require ongoing monitoring and periodic renewal to ensure you maintain competence and appropriate activity levels.
For many healthcare providers, managing privileging alongside insurance credentialing and billing becomes overwhelming. At Medwave, we provide billing, credentialing, and payer contracting services that help healthcare providers manage these administrative requirements efficiently. While we focus primarily on insurance credentialing and billing optimization, we work with many providers who are also navigating the hospital privileging process, and we recognize how these different credentialing activities interconnect.
Hospital privileges open doors to practice in hospital settings, but obtaining and maintaining them requires careful attention to detail, thorough documentation, and patience with lengthy approval processes.

