The moment healthcare providers have been waiting for has arrived. After years of anticipation, CMS has officially launched PECOS 2.0, bringing a completely redesigned approach to Medicare enrollment and revalidation. This isn’t just a minor update to the old system, it’s a ground-up transformation that affects every aspect of how providers join and maintain their Medicare participation.
If your role involves managing Medicare enrollment, credentialing, or revenue cycle operations, the changes in PECOS 2.0 will directly impact your daily workflow. Whether you’re handling applications for a single practitioner or managing hundreds of providers across multiple states, mastering this new system is critical to avoiding payment interruptions and maintaining your ability to treat Medicare patients.
What Makes PECOS 2.0 Different?
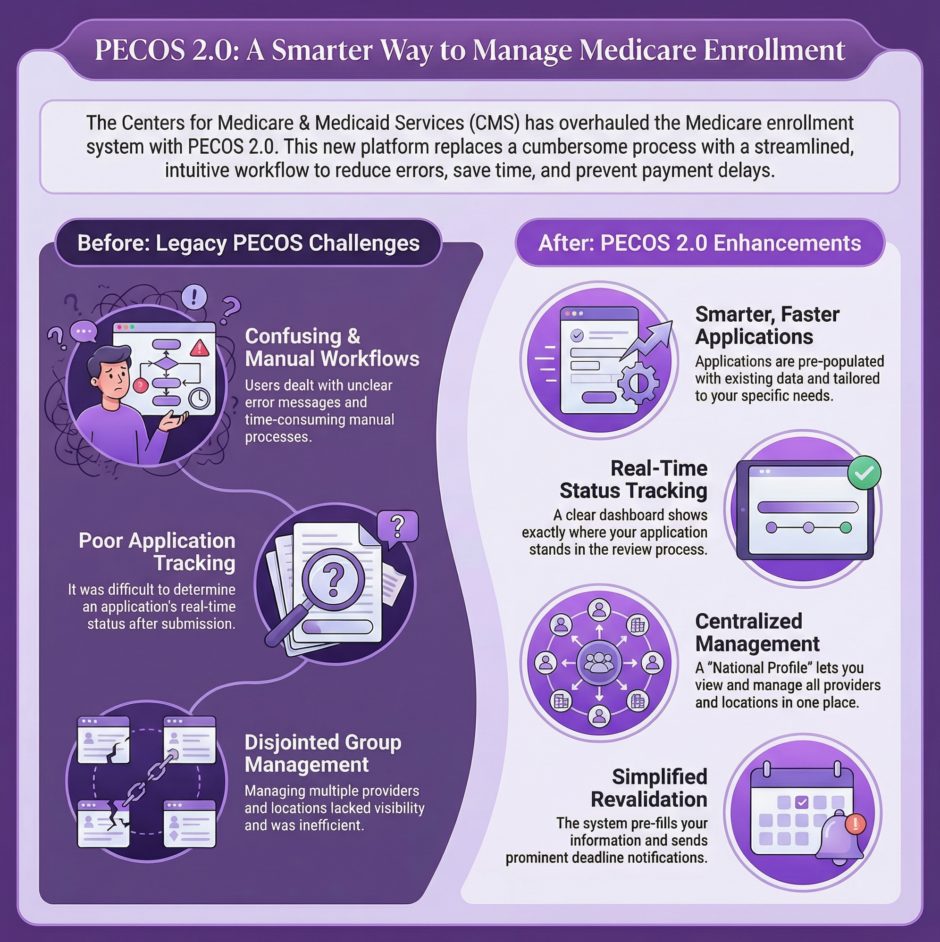
The original PECOS system served the healthcare community for many years, but it had significant limitations. Providers and credentialing specialists frequently dealt with confusing workflows, unclear error messages, and time-consuming manual processes. CMS recognized these pain points and built PECOS 2.0 from scratch with a focus on making the enrollment experience more intuitive and efficient.
The new platform features a modernized interface that guides users through each step of the application process. Gone are the days of wondering whether you’ve completed all required fields or submitted the right documentation. PECOS 2.0 provides clear prompts, better validation checks, and improved tracking capabilities so you always know exactly where your application stands.
For organizations managing multiple providers, the improvements are even more significant. The new system includes enhanced tools for authorized officials and delegated officials to oversee enrollment activities across their entire organization. This means better visibility, more control, and the ability to catch potential issues before they turn into denied applications or payment delays.
The Updated Enrollment Process: Step by Step
 Starting a new Medicare enrollment in PECOS 2.0 follows a more logical flow than the previous system. When you first log in, you’ll notice the dashboard presents information in a clearer, more organized manner. Your active applications, pending revalidations, and completed enrollments all appear in distinct sections, making it easy to prioritize your work.
Starting a new Medicare enrollment in PECOS 2.0 follows a more logical flow than the previous system. When you first log in, you’ll notice the dashboard presents information in a clearer, more organized manner. Your active applications, pending revalidations, and completed enrollments all appear in distinct sections, making it easy to prioritize your work.
The application itself walks you through provider information, practice locations, specialty designations, and supporting documentation in a sequential manner. Each section must be completed before moving forward, which helps prevent the common mistake of submitting incomplete applications. The system also performs real-time validation checks, alerting you immediately if information doesn’t match CMS records or if required fields are missing.
One of the most practical improvements involves how the system handles supporting documentation. Instead of uploading files and hoping they’re in the correct format, PECOS 2.0 tells you exactly what it needs, what file types are acceptable, and the maximum file sizes allowed. This eliminates much of the guesswork that previously led to application delays.
Managing Group Members and Multiple Locations
For practices with multiple providers or locations, PECOS 2.0 introduces new capabilities that were sorely lacking in the original system. Authorized officials can now manage their entire organization’s enrollment activities through a centralized dashboard. This includes adding new providers, reassigning providers to different locations, and monitoring the status of all pending applications.
The process for adding locations has been streamlined, particularly for sole proprietors expanding their practice footprint. Rather than starting from scratch each time you add a location, the system allows you to copy information from existing locations and modify only what’s different. This saves considerable time and reduces the risk of data entry errors.
Large healthcare organizations operating across multiple states will appreciate the improved state-specific guidance built into PECOS 2.0. The system recognizes which states your organization operates in and automatically presents the relevant requirements and documentation needs for each jurisdiction. This is particularly valuable for multi-state practices that previously had to track different state requirements manually.
Board members and practice managers gain better oversight capabilities through the new system. Delegated officials can be assigned specific permissions, allowing them to handle certain aspects of enrollment while restricting access to sensitive organizational information. This role-based access improves both security and efficiency.
The New Revalidation Process
 Revalidation, the process of confirming and updating your Medicare enrollment information periodically, has received significant attention in PECOS 2.0. CMS has simplified the revalidation workflow while maintaining the necessary oversight to prevent fraud and ensure accurate provider information.
Revalidation, the process of confirming and updating your Medicare enrollment information periodically, has received significant attention in PECOS 2.0. CMS has simplified the revalidation workflow while maintaining the necessary oversight to prevent fraud and ensure accurate provider information.
The system now sends more prominent notifications when revalidation deadlines approach. These alerts appear both within the PECOS 2.0 portal and via email to designated contacts. This multi-channel notification approach helps prevent the scenario where busy healthcare professionals miss critical revalidation deadlines.
When you begin a revalidation, PECOS 2.0 pre-populates all your existing information, allowing you to review and update only what has changed. This is a massive time-saver compared to the old system, where you often had to re-enter information that hadn’t changed. The system also clearly marks fields that require verification or updating, directing your attention to exactly what needs review.
Critical Timelines and Deadlines
Timing matters tremendously when it comes to Medicare enrollment. PECOS 2.0 provides better visibility into processing times and deadlines, but providers still need to plan accordingly. Initial enrollment applications typically take 30 to 90 days to process, depending on application completeness and whether any issues arise during review.
Revalidation cycles remain on their established schedule, typically occurring every five years for most provider types. However, CMS may require revalidation more frequently under certain circumstances, such as changes in ownership, practice location moves, or if there are concerns about billing patterns.
Missing a revalidation deadline carries serious consequences. Your Medicare billing privileges can be deactivated, which means claim denials and revenue interruption until the revalidation is completed and approved. PECOS 2.0 helps you avoid this scenario through its improved notification system, but the ultimate responsibility still rests with the provider and their administrative team to respond promptly.
For new providers trying to join a practice, timing their enrollment correctly ensures they can begin seeing Medicare patients without delay. Starting the enrollment process 90 to 120 days before the intended start date provides a comfortable buffer for processing time and addressing any issues that might arise.
Tracking Your Applications
 One of the most frustrating aspects of the original PECOS was the difficulty in determining application status. PECOS 2.0 addresses this with a robust tracking system that provides real-time updates on where your application stands in the review process.
One of the most frustrating aspects of the original PECOS was the difficulty in determining application status. PECOS 2.0 addresses this with a robust tracking system that provides real-time updates on where your application stands in the review process.
The tracking dashboard shows each application’s current stage, whether it’s under review, pending additional documentation, or approved. If CMS needs additional information, the system clearly states what’s required and provides a mechanism for submitting the requested materials directly through the portal.
This improved transparency benefits everyone involved in the enrollment process. Credentialing specialists can provide accurate updates to providers and practice managers. Revenue cycle teams can better forecast when new providers will be able to start billing Medicare. And authorized officials can identify bottlenecks in their organization’s enrollment pipeline before they cause problems.
Practical Tips for Preventing Denials
Despite the improvements in PECOS 2.0, applications can still face denials if proper attention isn’t paid to accuracy and completeness. The most common reasons for denial include mismatched information between PECOS and other federal databases, incomplete documentation, and errors in practice location information.
Before submitting any application, verify that your National Provider Identifier (NPI) information matches exactly what’s in the National Plan and Provider Enumeration System (NPPES). Discrepancies between these systems cause immediate red flags and can lead to processing delays or denials.
Pay particular attention to practice location information. The address must match official records, and the location must meet Medicare’s requirements for where services are provided. For providers who work at multiple locations, ensuring each location is properly documented and approved is crucial for billing privileges at those sites.
Documentation requirements vary based on provider type and enrollment category. Taking time to review CMS guidance specific to your situation before starting your application helps ensure you gather all necessary documents upfront. PECOS 2.0 provides better guidance on what’s needed, but cross-referencing with official CMS resources adds an extra layer of certainty.
Who Needs to Master PECOS 2.0?
 The reach of PECOS 2.0 extends across the healthcare industry. Obviously, credentialing specialists and enrollment specialists need deep familiarity with the system, it’s the primary tool they use daily. But the impact goes far beyond these roles.
The reach of PECOS 2.0 extends across the healthcare industry. Obviously, credentialing specialists and enrollment specialists need deep familiarity with the system, it’s the primary tool they use daily. But the impact goes far beyond these roles.
Revenue cycle managers and directors must grasp how PECOS 2.0 affects cash flow timelines and provider activation. Billing teams need to know when new providers are approved and active so they can begin submitting claims. Practice and clinic owners should stay informed about their organization’s enrollment status and any issues that arise.
Hospital leadership, authorized officials, and delegated officials bear responsibility for ensuring their organization maintains proper Medicare enrollment status. This includes overseeing the enrollment of employed physicians, managing location updates, and keeping track of revalidation deadlines across potentially hundreds of providers.
Front desk staff, scheduling teams, and authorization personnel also benefit from basic PECOS 2.0 knowledge. They often field questions from patients about provider participation in Medicare, and they need to know whether a provider is fully enrolled and active before scheduling Medicare patients.
Even professionals who aren’t directly involved in enrollment, like medical assistants, certified nursing assistants, and healthcare attorneys, gain value from awareness of how PECOS 2.0 works, as enrollment status affects their work environment and the patients they serve.
Why Partner with Experts?
 Given the stakes involved, payment delays, loss of Medicare participation, revenue interruption, many healthcare organizations choose to partner with specialists who live and breathe Medicare enrollment daily. This is where companies like Medwave come in. With expertise in medical billing, credentialing, and payer contracting, Medwave helps healthcare providers maintain smooth enrollment processes while freeing up internal staff to focus on patient care.
Given the stakes involved, payment delays, loss of Medicare participation, revenue interruption, many healthcare organizations choose to partner with specialists who live and breathe Medicare enrollment daily. This is where companies like Medwave come in. With expertise in medical billing, credentialing, and payer contracting, Medwave helps healthcare providers maintain smooth enrollment processes while freeing up internal staff to focus on patient care.
The transition to PECOS 2.0 represents both a challenge and an opportunity. Organizations that master the new system will experience smoother enrollments, fewer denials, and better oversight of their Medicare participation. Those that struggle with the changes risk payment interruptions and administrative headaches.
Taking time now to learn PECOS 2.0 thoroughly, establish clear internal processes, and consider expert support when needed will pay dividends in maintaining uninterrupted Medicare participation and revenue flow. The system is here to stay, and becoming proficient with it is no longer optional, it’s a necessity for every healthcare organization that serves Medicare beneficiaries.

