Medical credentialing has always been one of healthcare’s most time-consuming administrative tasks. For decades, healthcare providers have dealt with mountains of paperwork, endless verification calls, and months-long waiting periods just to get approved to see patients and receive insurance reimbursements. Artificial intelligence is now changing credentialing in ways that seemed impossible just a few years ago.
The Traditional Credentialing Headache
 Anyone who has worked in healthcare administration knows the credentialing process can be frustrating. When a new physician joins a practice or hospital, their credentials must be verified with multiple organizations. This means checking medical school diplomas, residency completion, board certifications, state licenses, DEA registrations, malpractice insurance, and work history. Each piece of information needs verification from its original source, which often means phone calls, faxes, and waiting for responses from institutions that might be slow to reply.
Anyone who has worked in healthcare administration knows the credentialing process can be frustrating. When a new physician joins a practice or hospital, their credentials must be verified with multiple organizations. This means checking medical school diplomas, residency completion, board certifications, state licenses, DEA registrations, malpractice insurance, and work history. Each piece of information needs verification from its original source, which often means phone calls, faxes, and waiting for responses from institutions that might be slow to reply.
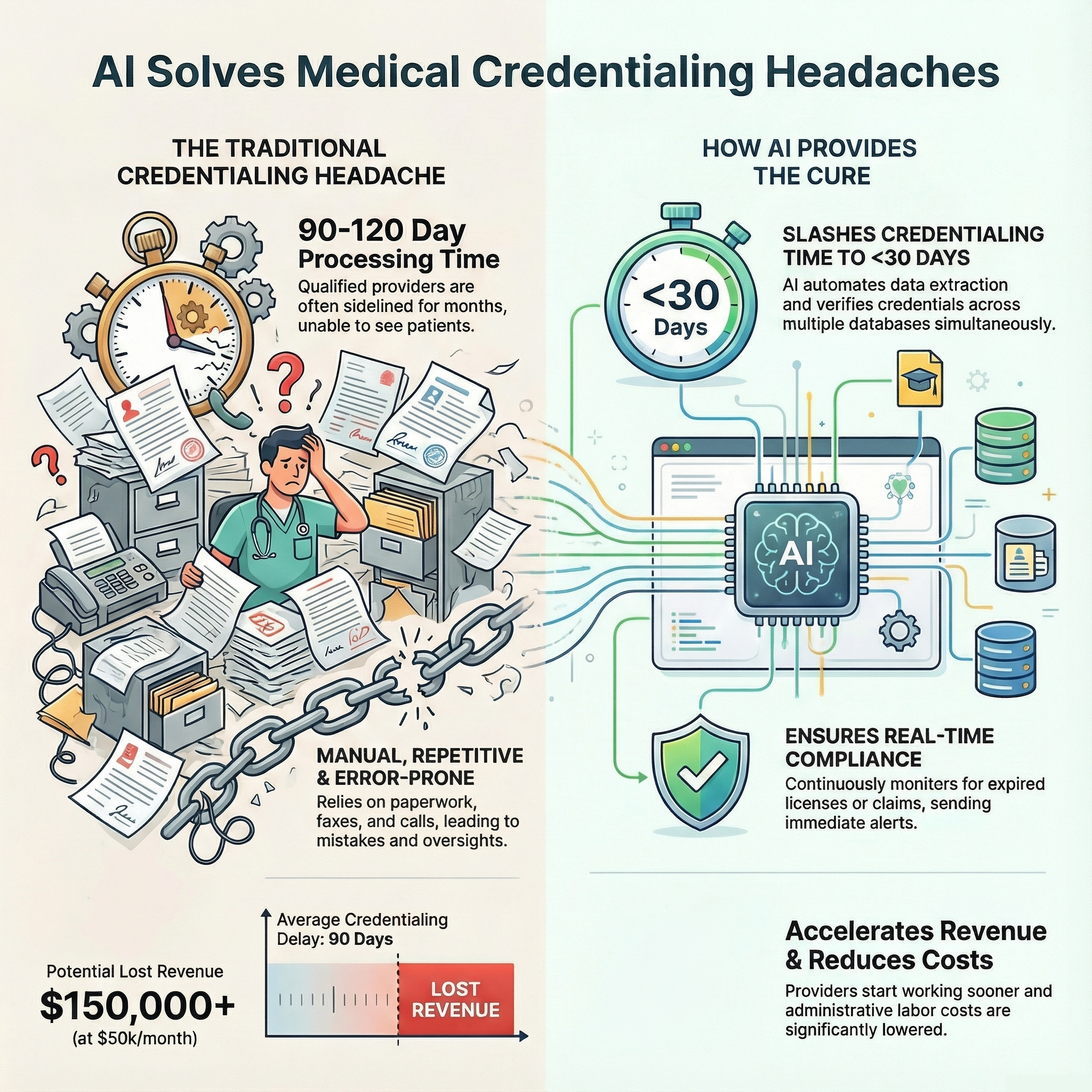
The process typically takes 90 to 120 days, sometimes longer. During this time, qualified physicians sit idle, unable to treat patients or generate revenue for their practice. Patients wait longer for appointments. Healthcare organizations lose money. Everyone involved feels the strain of an outdated system that relies heavily on manual labor and paper-based documentation.
How AI Steps In
Artificial intelligence is now tackling these challenges head-on. AI systems can automate many of the repetitive tasks that credentialing specialists spend hours completing. Instead of manually entering data from multiple documents into different databases, AI can extract information from forms, applications, and certificates in seconds. Optical character recognition (OCR) technology paired with machine learning algorithms can read documents, identify relevant information, and input that data into the appropriate fields with remarkable accuracy.
But AI does more than just data entry. These systems can cross-reference information across multiple databases simultaneously. When verifying a physician’s medical school graduation, for instance, AI can check the National Student Clearinghouse, the American Medical Association’s database, and state medical board records all at once. This parallel processing cuts verification time from days or weeks down to minutes or hours.
Reducing Human Error
 One of the biggest advantages AI brings to medical credentialing is consistency. Human credentialing specialists, no matter how experienced or dedicated, can make mistakes. They might overlook a gap in employment history, miss an expired certification, or accidentally transpose numbers in a license. These errors can lead to compliance issues, denied insurance claims, or even legal problems.
One of the biggest advantages AI brings to medical credentialing is consistency. Human credentialing specialists, no matter how experienced or dedicated, can make mistakes. They might overlook a gap in employment history, miss an expired certification, or accidentally transpose numbers in a license. These errors can lead to compliance issues, denied insurance claims, or even legal problems.
AI systems, once properly programmed and trained, apply the same rigorous standards to every application they process. They flag inconsistencies, identify missing information, and catch potential red flags that might slip past a tired or overworked staff member. This doesn’t mean AI replaces human judgment entirely, but it serves as an excellent first line of defense against errors and oversights.
Real-Time Monitoring and Updates
Perhaps one of the most valuable features AI brings to credentialing is continuous monitoring. In the traditional system, once a provider is credentialed, their information sits in a file until it’s time for re-credentialing, typically every two or three years. But credentials can change at any time. A license might expire, a board certification could lapse, or a malpractice claim might be filed. These changes often go unnoticed until re-credentialing time, potentially creating compliance gaps.
AI systems can monitor credentials in real-time. They can check state licensing boards, the National Practitioner Data Bank, and other relevant databases on a daily or weekly basis. When something changes, the system immediately alerts the appropriate personnel. This proactive approach prevents compliance issues before they become serious problems and keeps provider information constantly up to date.
The Financial Impact
 The financial benefits of AI-powered credentialing are significant. Consider the cost of having qualified providers sitting idle for three to four months while their credentials are processed. For a physician who could generate $50,000 or more per month in revenue, a 90-day credentialing delay represents a substantial loss. Multiply this across multiple providers in a growing practice or hospital system, and the numbers become staggering.
The financial benefits of AI-powered credentialing are significant. Consider the cost of having qualified providers sitting idle for three to four months while their credentials are processed. For a physician who could generate $50,000 or more per month in revenue, a 90-day credentialing delay represents a substantial loss. Multiply this across multiple providers in a growing practice or hospital system, and the numbers become staggering.
AI dramatically shortens these timelines. Some organizations report reducing credentialing time from 90 days to 30 days or less. This means providers can start seeing patients sooner, generating revenue faster, and filling appointment slots that would otherwise remain empty. The return on investment for AI credentialing systems often pays for itself within the first year of implementation.
Key Benefits of AI in Medical Credentialing
The advantages of incorporating AI into the credentialing process extend across several areas:
- Speed: Processing times drop from months to weeks or even days, getting providers working faster
- Accuracy: Automated checks reduce human error and catch inconsistencies that might otherwise be missed
- Cost savings: Less manual labor means lower administrative costs and faster revenue generation
- Compliance: Real-time monitoring keeps credentials current and identifies issues immediately
- Scalability: AI systems can handle increased volume without requiring proportional increases in staff
- Documentation: Digital systems create clear audit trails and maintain organized records automatically
Challenges and Considerations
 While AI offers tremendous benefits, implementing these systems isn’t without challenges. Healthcare organizations need to invest in the right technology and ensure it integrates with their existing systems. Staff members require training to work effectively with AI tools, and there’s often an adjustment period as everyone learns new workflows.
While AI offers tremendous benefits, implementing these systems isn’t without challenges. Healthcare organizations need to invest in the right technology and ensure it integrates with their existing systems. Staff members require training to work effectively with AI tools, and there’s often an adjustment period as everyone learns new workflows.
Data security is another critical concern. Credentialing involves sensitive personal information, including Social Security numbers, addresses, and professional history. AI systems must meet strict HIPAA compliance standards and employ robust cybersecurity measures to protect this data from breaches or unauthorized access.
Some healthcare professionals initially resist AI implementation, worried that automation might replace their jobs. However, the reality is that AI works best as a tool to augment human capabilities rather than replace them. Credentialing still requires human judgment for nuanced decisions, relationship management with providers, and handling exceptions that fall outside standard parameters. AI simply eliminates the tedious, repetitive aspects of the job, allowing credentialing specialists to focus on more valuable, strategic work.
The Human Touch Still Matters
Despite all the technological advances, medical credentialing still benefits from human expertise. AI excels at processing data, identifying patterns, and flagging potential issues, but people are still needed to interpret context, make judgment calls, and build relationships with healthcare providers. The most effective credentialing operations use AI to handle the routine tasks while human specialists focus on the situations that require critical thinking and personal interaction.
For example, when a provider has an unusual career path or credentials from international institutions, AI might flag these items as anomalies. A human credentialing specialist can then review the situation, contact the provider for clarification, and make appropriate decisions based on the full context. This combination of AI efficiency and human judgment creates a credentialing process that’s both fast and thorough.
Looking Ahead
 The future of AI in medical credentialing looks promising. As machine learning algorithms continue to improve, they’ll become even better at recognizing patterns, predicting potential issues, and streamlining workflows. Integration with other healthcare systems will become more seamless, creating a more connected ecosystem where information flows easily between credentialing databases, electronic health records, billing systems, and insurance networks.
The future of AI in medical credentialing looks promising. As machine learning algorithms continue to improve, they’ll become even better at recognizing patterns, predicting potential issues, and streamlining workflows. Integration with other healthcare systems will become more seamless, creating a more connected ecosystem where information flows easily between credentialing databases, electronic health records, billing systems, and insurance networks.
We’re also likely to see increased standardization in credentialing requirements as AI makes it easier to maintain consistent standards across different organizations and states. Blockchain technology might eventually play a role in credentialing as well, creating immutable records of credentials that can be instantly verified by any authorized party.
Partnering with Experts
 For healthcare practices and organizations looking to improve their credentialing processes, partnering with experienced administrative service providers can make the transition smoother. At Medwave, we specialize in billing, credentialing, and payer contracting and are already incorporating AI tools into our workflows to deliver faster, more accurate results for their clients. These partnerships allow healthcare providers to benefit from cutting-edge technology without having to invest in and maintain these systems themselves.
For healthcare practices and organizations looking to improve their credentialing processes, partnering with experienced administrative service providers can make the transition smoother. At Medwave, we specialize in billing, credentialing, and payer contracting and are already incorporating AI tools into our workflows to deliver faster, more accurate results for their clients. These partnerships allow healthcare providers to benefit from cutting-edge technology without having to invest in and maintain these systems themselves.
The transformation of medical credentialing through AI represents a significant step forward for healthcare administration. Reducing the time, cost, and potential for error in the credentialing process, AI allows healthcare organizations to focus more of their energy and resources on more important areas. As these technologies continue to advance and become more widely adopted, the entire healthcare industry stands to benefit from more efficient, accurate, and responsive credentialing systems.

