*Imagine this: You’re running a successful physician practice, your patients are satisfied, and your clinical outcomes are stellar. But when you look at your financial statements, something doesn’t add up. Cash flow feels like a constant uphill battle, insurance denials seem to multiply overnight, and your administrative team is drowning in paperwork. Sound familiar?
Welcome to the modern healthcare landscape, where clinical excellence doesn’t automatically translate to financial success. Revenue cycle management (RCM) has become both a critical lifeline and a persistent headache. The good news? With the right strategies and approach, you can transform these challenges into opportunities for sustainable growth and operational excellence.
The Current State of Revenue Cycle Management

Healthcare is cruising at breakneck speed. Regulatory changes, shifting payer policies, increasing patient financial responsibility, and technological disruptions are reshaping how physician groups manage their revenue cycles. What worked five years ago might be actively hurting your bottom line today.
The stakes couldn’t be higher. Inefficient RCM processes don’t just impact your cash flow, they affect your ability to invest in better patient care, attract top talent, and grow your practice.
Meanwhile, administrative costs continue to climb, with some estimates suggesting that up to 30% of healthcare spending goes toward administrative expenses rather than patient care.
While these challenges are real and significant, they’re not insurmountable. The physician groups that are thriving in this environment aren’t necessarily the largest or best-funded, they’re the ones that have mastered the art and science of revenue cycle optimization.
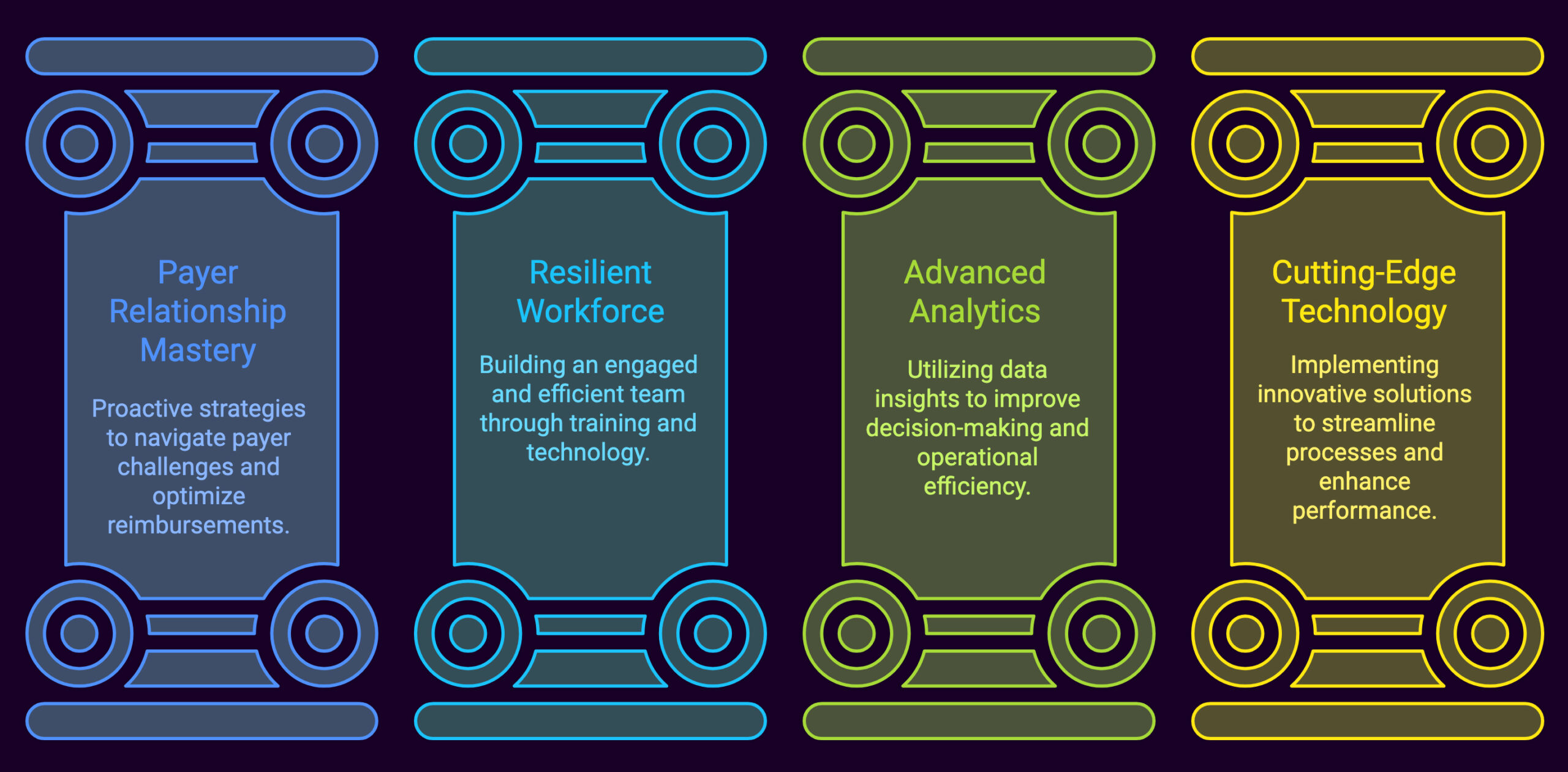
The Four Pillars of Revenue Cycle Excellence
1. Mastering the Payer Relationship Game
Let’s start with the elephant in the room, payer behavior. If you’ve been in healthcare for more than five minutes, you’ve experienced the frustration of excessive denials, delayed reimbursements, and constantly changing payer requirements. It’s enough to make anyone want to throw in the towel.
The traditional approach, submit claims and hope for the best, is a recipe for disaster in today’s environment. Instead, successful physician groups are taking a proactive stance. They’re implementing sophisticated denial management tools that include rules engines specifically aligned with individual payer requirements. Think of it as having a personal translator for each insurance company’s unique language.
Pre-bill edits are game-changers here. By catching errors before claims ever leave your office, you’re not just reducing rework, you’re fundamentally changing the economics of your revenue cycle. Clean claims get processed faster, paid more quickly, and require less administrative overhead. It’s like the difference between proofreading an important email before sending it versus dealing with the embarrassment and confusion of clarifying what you meant to say later.
But payer challenges extend beyond just claim processing. The rise of high-deductible health plans has shifted significant financial responsibility to patients, creating a whole new set of collection challenges. Patients who used to pay $20 copays are now facing $2,000 deductibles, fundamentally changing their relationship with healthcare costs.
Smart physician groups are adapting by implementing patient-friendly payment solutions. Online bill pay, text-to-pay options, and automated reminders aren’t just convenient, they’re essential tools for maintaining healthy cash flow in an era of increased patient responsibility. These technologies meet patients where they are, making it easier for them to fulfill their financial obligations while reducing your administrative burden.
Don’t overlook the power of strategic contract negotiation either. Your clinical quality, patient volume, and specialized services are valuable commodities. Physician groups that leverage these strengths in payer negotiations often achieve better reimbursement rates and more favorable contract terms. It’s about shifting from a reactive to a proactive stance in your payer relationships.
2. Building a Resilient and Efficient Workforce
 The healthcare workforce crisis is real, and it’s particularly acute in revenue cycle management roles. High turnover, skill gaps, and burnout are creating perfect storms that can devastate your financial performance. But the solution isn’t just about hiring more people, it’s about creating a more effective, engaged, and sustainable workforce.
The healthcare workforce crisis is real, and it’s particularly acute in revenue cycle management roles. High turnover, skill gaps, and burnout are creating perfect storms that can devastate your financial performance. But the solution isn’t just about hiring more people, it’s about creating a more effective, engaged, and sustainable workforce.
The most successful physician groups are taking a holistic approach to workforce optimization. They’re investing in comprehensive training programs that go beyond the “what” to focus on the “why.” When your team understands not just which buttons to click but why each step matters, they become more engaged, make fewer errors, and feel more connected to the organization’s mission.
Technology plays a crucial role here, but not in the way you might expect. Rather than replacing human workers, the smartest applications of technology amplify human capabilities. Automated claim status checks, denial appeal generation, and eligibility verification free up your staff to focus on complex problem-solving and relationship-building activities that actually require human judgment and creativity.
This approach creates a virtuous cycle. Staff feel more engaged because they’re doing meaningful work, job satisfaction increases, turnover decreases, and overall efficiency improves. Meanwhile, patients benefit from more personalized service, and your practice benefits from improved financial performance.
Cross-training is another underutilized strategy. When team members can handle multiple aspects of the revenue cycle, you create flexibility and resilience. Staff absences don’t create bottlenecks, and you can adjust workloads based on seasonal variations or unexpected challenges.
3. Harnessing the Power of Advanced Analytics
Here’s where many physician groups are leaving money on the table. In our data-rich environment, the ability to analyze and act on information isn’t just nice to have, it’s essential for survival. Yet many practices are still making decisions based on gut feelings or outdated reports rather than real-time insights.
Modern analytics go far beyond basic reporting. They provide targeted insights into payer behavior patterns, staff performance trends, and operational inefficiencies that might not be visible from traditional metrics. For example, analytics might reveal that a particular payer consistently denies claims for a specific procedure code on Tuesdays, suggesting a pattern in their review process that you can work around.
The key is making analytics actionable and accessible. Custom dashboards that track critical metrics like cash flow, accounts receivable days, and denial rates should present information in formats that busy healthcare professionals can quickly understand and act upon. The goal isn’t to turn physicians into data scientists, it’s to put powerful insights at their fingertips.
Real-time, exception-based business intelligence takes this a step further. Instead of waiting for monthly reports, these systems proactively alert the right people when metrics fall outside acceptable ranges. It’s like having a financial early warning system that helps you address problems before they become crises.
Consider the impact of predictive analytics on denial management. Analyzing historical patterns allows you to identify claims that are likely to be denied before they’re submitted. This allows you to proactively address issues, reducing both the administrative burden of appeals and the cash flow impact of delayed payments.
4. Embracing Cutting-Edge Technology Solutions
 Technology isn’t just changing healthcare, it’s revolutionizing it. From artificial intelligence to automation, the tools available to physician groups today can dramatically improve efficiency, reduce errors, and enhance financial performance. But the key is thoughtful implementation rather than technology for technology’s sake.
Technology isn’t just changing healthcare, it’s revolutionizing it. From artificial intelligence to automation, the tools available to physician groups today can dramatically improve efficiency, reduce errors, and enhance financial performance. But the key is thoughtful implementation rather than technology for technology’s sake.
AI applications in revenue cycle management are particularly promising. Machine learning algorithms can predict denial likelihood with remarkable accuracy, generate appeal letters that address specific denial reasons, and even automate the retrieval of medical records needed for appeals. These aren’t futuristic concepts, they’re available today and being successfully implemented by forward-thinking physician groups.
Automation excels at handling repetitive, rule-based tasks that consume significant staff time. Eligibility verification, claim status checks, and payment posting are perfect candidates for automation. When these routine tasks are handled automatically, your staff can focus on exception handling and relationship building.
Unified data platforms deserve special attention. Many physician groups struggle with fragmented systems that don’t communicate effectively with each other. A unified platform that integrates practice management, electronic health records, and billing systems creates a single source of truth and eliminates many inefficiencies caused by data silos.
The most advanced platforms combine AI, intelligent automation, and deep data analytics to turn complex healthcare data into actionable insights. These systems learn from patterns, identify opportunities, and recommend actions that can improve financial and operational performance.
Real-World Success: The Power of Strategic Implementation

The theoretical benefits of these strategies are compelling, but what do they look like in practice? Consider a recent case study involving a physician group that was struggling with excessive denials and cash flow challenges. Through a collaborative approach focusing on analytics, technology, and process optimization, they achieved remarkable results over five years.
The numbers tell the story: an 80% increase in net revenue, 73% increase in gross revenue, and 21% reduction in accounts receivable days. But perhaps more importantly, they also improved patient experiences and built a more sustainable operation that weathered the COVID-19 pandemic better than many of their peers.
This transformation didn’t happen overnight. It required strategic thinking, careful implementation, and ongoing optimization. Yet, the results demonstrate what’s possible when physician groups take an all-inclusive approach to revenue cycle management.
Immediate Actions for Accelerated Results
Ready to start your own transformation?
Here are concrete steps you can take immediately:
- Conduct a comprehensive denial audit. Don’t just look at denial rates, dig into the reasons behind denials. Are there patterns by payer, procedure code, or time of month? Use this information to implement targeted pre-bill edits and training programs.
- Invest in meaningful staff training. Move beyond procedural training to help your team understand the broader context of their work. When staff understand how their individual tasks connect to patient care and practice success, engagement and performance improve dramatically.
- Start small with automation. You don’t need to automate everything at once. Begin with high-volume, routine tasks like claim status checks or basic denial scrubbing. Build confidence and expertise before tackling more complex processes.
- Implement actionable analytics. Begin with dashboards that track key performance indicators relevant to your specific challenges. Focus on metrics that you can actually influence and that connect directly to financial outcomes.
- Evaluate your technology stack. Are your current systems helping or hindering your efficiency? Look for opportunities to consolidate platforms, eliminate redundancies, and improve integration between systems.
Seizing Opportunities for Growth
![]() The healthcare landscape will continue to evolve, but the principles of effective revenue cycle management remain consistent: proactive payer relationship management, strategic workforce optimization, data-driven decision making, and thoughtful technology implementation.
The healthcare landscape will continue to evolve, but the principles of effective revenue cycle management remain consistent: proactive payer relationship management, strategic workforce optimization, data-driven decision making, and thoughtful technology implementation.
Physician groups that master these elements don’t just survive in today’s challenging environment, they thrive. They’re able to focus more time and resources on patient care, attract and retain top talent, and build sustainable growth platforms for the future.
The question isn’t whether you should optimize your revenue cycle, it’s how quickly you can begin the transformation. Every day you delay is another day of lost revenue, frustrated staff, and missed opportunities. But with the right approach and support, you can turn your revenue cycle from a source of stress into a competitive advantage.
Contact us today to speak with someone on how we can be an affordable revenue cycle asset to you and your healthcare group’s future.