Medical credentialing stands as one of the most complete and rigorous examples of professional credentialing in any industry. This systematic process ensures that healthcare providers possess the necessary qualifications, training, and competencies to deliver safe, effective patient care. Knowing the essentials of medical credentialing provides valuable insight into how credentialing works, why it matters, and what makes it so essential for protecting public health and safety.
The Foundation of Medical Credentialing
Medical credentialing is a formal process used by healthcare organizations, hospitals, insurance companies, and regulatory bodies to verify that healthcare providers have the proper qualifications to practice medicine. This process goes far beyond simply checking that someone has a medical degree. It involves an all-encompassing evaluation of a physician’s educational background, training history, professional experience, competency, and ongoing ability to provide quality patient care.
 The credentialing process serves multiple critical functions within the healthcare system. It protects patients by ensuring that only qualified providers can practice medicine in specific settings. It provides legal protection for healthcare organizations by demonstrating due diligence in vetting their medical staff. It also helps maintain professional standards across the medical community and supports quality improvement initiatives by identifying areas where providers may need additional training or support.
The credentialing process serves multiple critical functions within the healthcare system. It protects patients by ensuring that only qualified providers can practice medicine in specific settings. It provides legal protection for healthcare organizations by demonstrating due diligence in vetting their medical staff. It also helps maintain professional standards across the medical community and supports quality improvement initiatives by identifying areas where providers may need additional training or support.
The stakes in medical credentialing are exceptionally high. Unlike many other professions where errors might result in financial losses or inconvenience, mistakes in healthcare can directly impact patient safety and outcomes. This reality drives the thoroughness and rigor that characterizes medical credentialing processes.
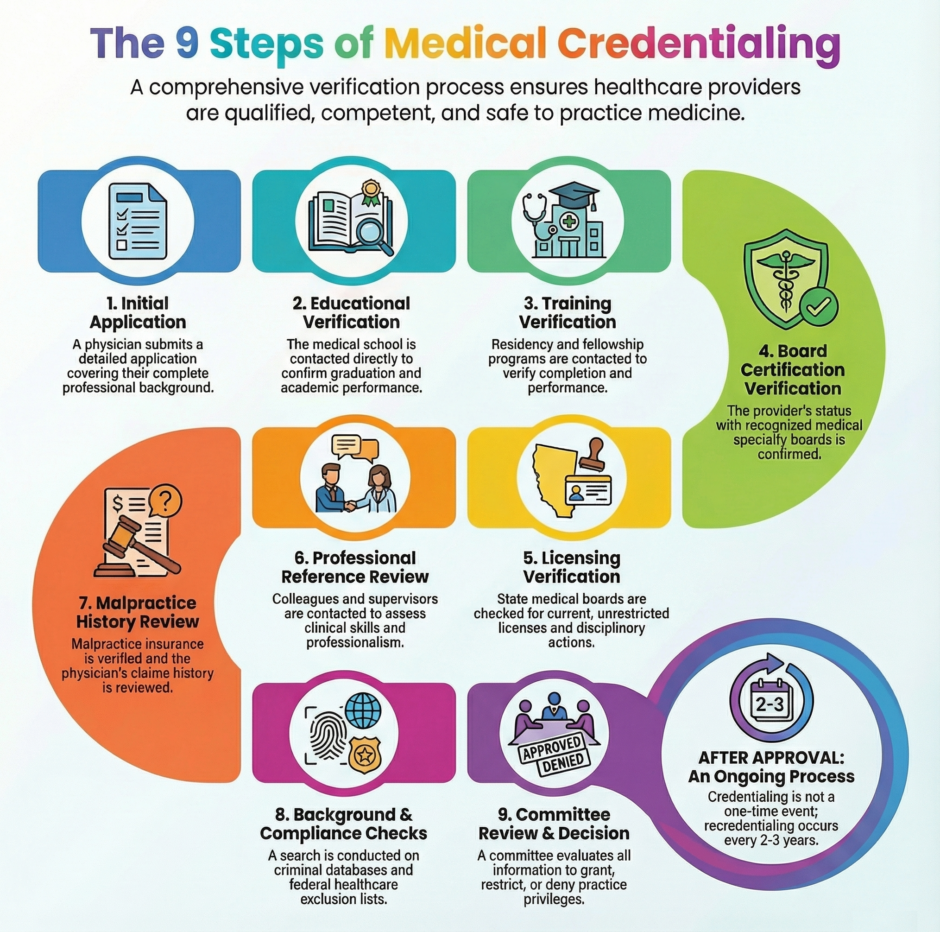
The Medical Credentialing Process in 9-Steps
When a physician applies for hospital privileges or seeks to join a medical group, they must undergo a thorough credentialing process that typically takes three to six months to complete. This timeline reflects the extensive verification requirements and the careful review process that credentialing committees must undertake.
1. Initial Application and Documentation
The credentialing process begins when a physician submits a detailed application that can span dozens of pages. This application requests complete information about every aspect of the physician’s professional background. The physician must provide detailed information about their medical education, including specific dates of attendance, degrees earned, and any honors or distinctions received. They must also document all residency and fellowship training, including program names, dates, and supervising physicians.
The application requires a complete employment history, including all positions held since medical school graduation. For each position, the physician must provide specific details about their responsibilities, patient populations served, and reasons for leaving. This employment history helps credentialing committees understand the physician’s experience and identify any potential red flags or gaps in employment.
Professional references form another crucial component of the initial application. Physicians must provide contact information for colleagues, supervisors, and other healthcare professionals who can speak to their clinical competence, professional behavior, and overall suitability for the position. These references typically include department heads, medical directors, and peer physicians who have worked closely with the applicant.
2. Educational Verification
Educational verification represents one of the most fundamental aspects of medical credentialing. The credentialing committee contacts medical schools directly to confirm that the physician graduated from an accredited institution and to verify their academic performance. This primary source verification is essential because it ensures that the physician received proper foundational training in medical sciences and clinical practice.
The verification process extends beyond simply confirming graduation dates. Credentialing committees often review academic transcripts to understand the physician’s performance in key subject areas and to identify any academic difficulties or distinctions. They also verify that the medical school maintains proper accreditation from recognized bodies such as the Liaison Committee on Medical Education (LCME) for US medical schools or equivalent international accrediting organizations.
For physicians who attended international medical schools, the verification process often includes additional steps to ensure that their education meets US standards. This may involve verification through organizations like the Educational Commission for Foreign Medical Graduates (ECFMG) and confirmation that the physician has passed required examinations such as the United States Medical Licensing Examination (USMLE) steps.
3. Residency and Fellowship Training Verification
Residency training verification forms another critical component of medical credentialing. The credentialing committee contacts training programs directly to confirm that the physician completed required residency training in their specialty area. This verification includes confirming the duration of training, evaluating the physician’s performance during residency, and ensuring that the training program meets accreditation standards established by the Accreditation Council for Graduate Medical Education (ACGME) or equivalent bodies.
The verification process examines multiple aspects of the physician’s residency training. Credentialing committees review evaluations from residency supervisors, confirm that the physician met all training requirements, and verify that they successfully completed the program. They also examine any disciplinary actions or concerns that arose during training and assess how these issues were resolved.
For physicians who completed fellowship training in subspecialties, this additional training must also be verified and documented. Fellowship verification follows similar procedures to residency verification, including confirmation of program accreditation, review of performance evaluations, and verification of successful completion. This subspecialty training verification is particularly important for physicians seeking privileges in specialized areas of practice.
4. Board Certification Verification
Board certification verification adds another essential layer to the credentialing process. The credentialing committee confirms that the physician has passed rigorous examinations administered by recognized medical specialty boards such as the American Board of Internal Medicine, American Board of Surgery, or other specialty boards recognized by the American Board of Medical Specialties (ABMS).
This verification process ensures that the physician has demonstrated competency in their chosen specialty through standardized testing that evaluates both theoretical knowledge and practical application of medical principles. The credentialing committee verifies not only that the physician passed these examinations but also that they maintain current board certification through required continuing medical education and periodic re-examination.
Some credentialing processes also recognize board certification from osteopathic specialty boards or international certification bodies, depending on the healthcare organization’s policies and the physician’s background. The key requirement is that the certifying body maintains recognized standards and credible examination processes.
5. Licensing Verification
Medical license verification represents a fundamental aspect of credentialing that ensures physicians have the legal authority to practice medicine. The credentialing committee confirms that the physician holds current, unrestricted medical licenses in all states where they have practiced or intend to practice. This verification includes checking with state medical boards to confirm license status and reviewing any disciplinary actions, license suspensions, or restrictions that might affect the physician’s ability to practice safely and effectively.
The licensing verification process extends beyond simply confirming current license status. Credentialing committees review the physician’s entire licensing history, including any disciplinary actions taken by state medical boards, voluntary license surrenders, or restrictions placed on practice. They also verify that the physician meets continuing medical education requirements for license renewal and that all license fees and requirements are current.
For physicians licensed in multiple states, the credentialing committee must verify each license independently. This multi-state verification can be particularly complex but is essential for physicians who practice across state lines or who have moved between states during their careers.
6. Professional Reference and Peer Review
Professional reference verification involves contacting colleagues, supervisors, and other healthcare professionals who have worked with the physician. These references provide crucial insights into the physician’s clinical competence, professional behavior, communication skills, and overall suitability for hospital privileges or group membership.
The credentialing committee typically requires multiple references from different sources to gain a thorough knowledge of the physician’s professional capabilities. These references might include department chairs, medical directors, nursing supervisors, and peer physicians who can speak to different aspects of the physician’s practice. The committee often uses structured reference forms to ensure that all relevant areas are addressed consistently.
Reference verification goes beyond simply confirming that the physician worked at specific locations. References are asked to evaluate the physician’s clinical skills, decision-making abilities, communication with patients and colleagues, professionalism, and ability to work effectively within healthcare teams. They may also be asked about any concerns or areas for improvement that they observed during their professional relationship with the physician.
7. Malpractice Insurance and Claims History
Malpractice insurance verification ensures that the physician carries adequate professional liability coverage to protect both the physician and the healthcare organization. The credentialing committee confirms that the physician’s insurance meets the organization’s minimum requirements and reviews the physician’s claims history to identify any patterns of concern.
The claims history review is particularly important because it can reveal patterns of practice that might indicate increased risk or areas where the physician might benefit from additional training or support. The credentialing committee examines not only the number of claims but also the nature of the claims, their outcomes, and any corrective actions taken by the physician or previous employers.
This review process requires careful consideration because malpractice claims can occur even when care meets appropriate standards. The credentialing committee must distinguish between isolated incidents and patterns that might indicate systemic issues with the physician’s practice or decision-making.
8. Background Checks and Regulatory Compliance
Extremely in-depth background checks form an essential component of medical credentialing that helps ensure physicians meet the ethical and legal standards expected of healthcare professionals. These checks include criminal history verification, exclusion list checks, and review of any regulatory actions taken against the physician.
The background check process includes searches of federal and state criminal databases, sex offender registries, and terrorist watch lists. While not all criminal history automatically disqualifies a physician from practice, credentialing committees must carefully evaluate any findings to determine whether they impact the physician’s ability to provide safe patient care.
Exclusion list checks verify that the physician has not been excluded from participation in federal healthcare programs such as Medicare and Medicaid. The credentialing committee checks databases maintained by the Office of Inspector General and other regulatory bodies to ensure that the physician can participate in these programs without creating compliance issues for the healthcare organization.
9. Credentialing Committee Review and Decision
After completing the in-depth verification process, the credentialing committee reviews all gathered information to make informed decisions about the physician’s privileges. This review process involves multiple healthcare professionals who evaluate the physician’s qualifications against established criteria and standards specific to the healthcare organization and the physician’s intended scope of practice.
The committee review is thorough and deliberative, often involving multiple meetings and careful consideration of all available information. Committee members may include medical staff leaders, department chairs, quality improvement professionals, and risk management representatives who bring different perspectives to the evaluation process.
The credentialing committee may reach several different conclusions based on their review. They may grant full privileges as requested, allowing the physician to practice within their requested scope. They may grant privileges with restrictions, limiting certain aspects of practice until the physician demonstrates additional competency or addresses identified concerns. In some cases, they may deny privileges entirely if they determine that the physician does not meet the organization’s standards or poses unacceptable risks to patient safety.
Ongoing Monitoring and Recredentialing
Medical credentialing is not a one-time process but rather an ongoing system of monitoring and evaluation. Most healthcare organizations require regular recredentialing, typically every two to three years, to ensure that physicians maintain their qualifications and continue to practice safely and effectively.
 The recredentialing process involves reviewing the physician’s performance during the intervening period, including quality metrics, patient satisfaction scores, peer evaluations, and any incidents or concerns that arose during practice. The process also includes verification of continued compliance with licensing, board certification, and continuing medical education requirements.
The recredentialing process involves reviewing the physician’s performance during the intervening period, including quality metrics, patient satisfaction scores, peer evaluations, and any incidents or concerns that arose during practice. The process also includes verification of continued compliance with licensing, board certification, and continuing medical education requirements.
Continuous monitoring between formal recredentialing cycles helps identify issues that require immediate attention. This monitoring might include review of quality indicators, patient complaints, sentinel events, or changes in the physician’s licensure or certification status. Healthcare organizations maintain systems to track these indicators and respond quickly when concerns arise.
The Impact of Medical Credentialing
Medical credentialing has profound impacts on healthcare quality, patient safety, and the broader healthcare system. For patients, credentialing provides assurance that their healthcare providers have met rigorous standards and have been thoroughly vetted before being granted privileges to practice. This assurance is particularly important given the complexity of modern healthcare and the potential consequences of inadequate care.
For healthcare organizations, credentialing provides legal protection and helps maintain quality standards. Organizations that fail to properly credential their medical staff may face liability for negligent credentialing if inadequately qualified physicians cause patient harm. Proper credentialing demonstrates due diligence and helps protect organizations from these risks.
For the medical profession as a whole, credentialing helps maintain professional standards and public trust. The rigorous requirements and continuous monitoring help ensure that the medical profession continues to merit the trust and respect that society places in healthcare providers.
Challenges and Future Directions
 Despite its importance, medical credentialing faces several ongoing challenges. The process can be time-consuming and expensive, potentially creating barriers for qualified physicians seeking to practice in new locations or join new organizations. The lack of standardization across different healthcare organizations can create inefficiencies and delays when physicians move between positions.
Despite its importance, medical credentialing faces several ongoing challenges. The process can be time-consuming and expensive, potentially creating barriers for qualified physicians seeking to practice in new locations or join new organizations. The lack of standardization across different healthcare organizations can create inefficiencies and delays when physicians move between positions.
Technology is beginning to address some of these challenges through digital credentialing platforms that streamline verification processes and improve data sharing between organizations. These platforms can reduce the time and cost associated with credentialing while maintaining the thoroughness and accuracy that patient safety requires.
The future of medical credentialing will likely involve greater standardization, improved technology platforms, and more efficient processes that maintain rigorous standards while reducing administrative burden. Innovations such as blockchain technology may further enhance the security and portability of credentialing information.
Summary: A Step-by-Step Example of The Credentialing Process
 Credentialing exemplifies the thorough approach to professional verification that protects public safety and maintains professional standards. Through its rigorous process of education verification, training confirmation, competency assessment, and ongoing monitoring, medical credentialing ensures that healthcare providers meet the highest standards of qualification and performance.
Credentialing exemplifies the thorough approach to professional verification that protects public safety and maintains professional standards. Through its rigorous process of education verification, training confirmation, competency assessment, and ongoing monitoring, medical credentialing ensures that healthcare providers meet the highest standards of qualification and performance.
This system, while complicated and time-consuming, represents an essential safeguard in healthcare delivery and serves as a model for credentialing processes in other high-stakes professions. Medical credentialing helps illustrate why thorough professional verification is so crucial and how it contributes to maintaining trust and safety in healthcare delivery.

