The term “delegated credentialing” might not immediately grab your attention. Yet, this behind-the-scenes process significantly impacts how healthcare providers operate, how quickly patients can access care, and how efficiently our healthcare system functions.
What Makes Delegated Credentialing Different?
Delegated credentialing shifts this responsibility from health plans (insurance companies) to healthcare organizations themselves. Through this arrangement, a health plan formally authorizes a healthcare organization, such as a hospital, physician group, or integrated delivery network to handle the credentialing process on their behalf.

In other words, instead of each insurance company separately verifying a doctor’s credentials, they trust the healthcare organization to do this work according to mutually agreed-upon standards. The health plan then accepts the organization’s credentialing decisions.
Let’s use an example: Imagine a large medical group with 50 physicians that contracts with 10 different health plans. Without delegated credentialing, each of those 10 health plans would separately credential all 50 physicians, creating 500 separate credentialing processes. With delegated credentialing, the medical group credentials each physician once, and all 10 health plans accept that credential. This converts 500 processes into just 50.
The Delegation Agreement: Setting the Rules
The foundation of delegated credentialing is the delegation agreement. A formal contract between the health plan and the healthcare organization.
This agreement:
- Defines the specific credentialing responsibilities being delegated
- Establishes performance standards and requirements
- Outlines reporting obligations and timeframes
- Sets terms for oversight and auditing
- Details remediation processes if standards aren’t met
- Specifies termination conditions
Health plans don’t simply hand over credentialing authority and walk away. Instead, they maintain oversight through regular audits and reports to ensure their standards are consistently met. Typically, a health plan will conduct pre-delegation assessments before granting authority and will perform annual audits thereafter.
Benefits of Delegated Credentialing
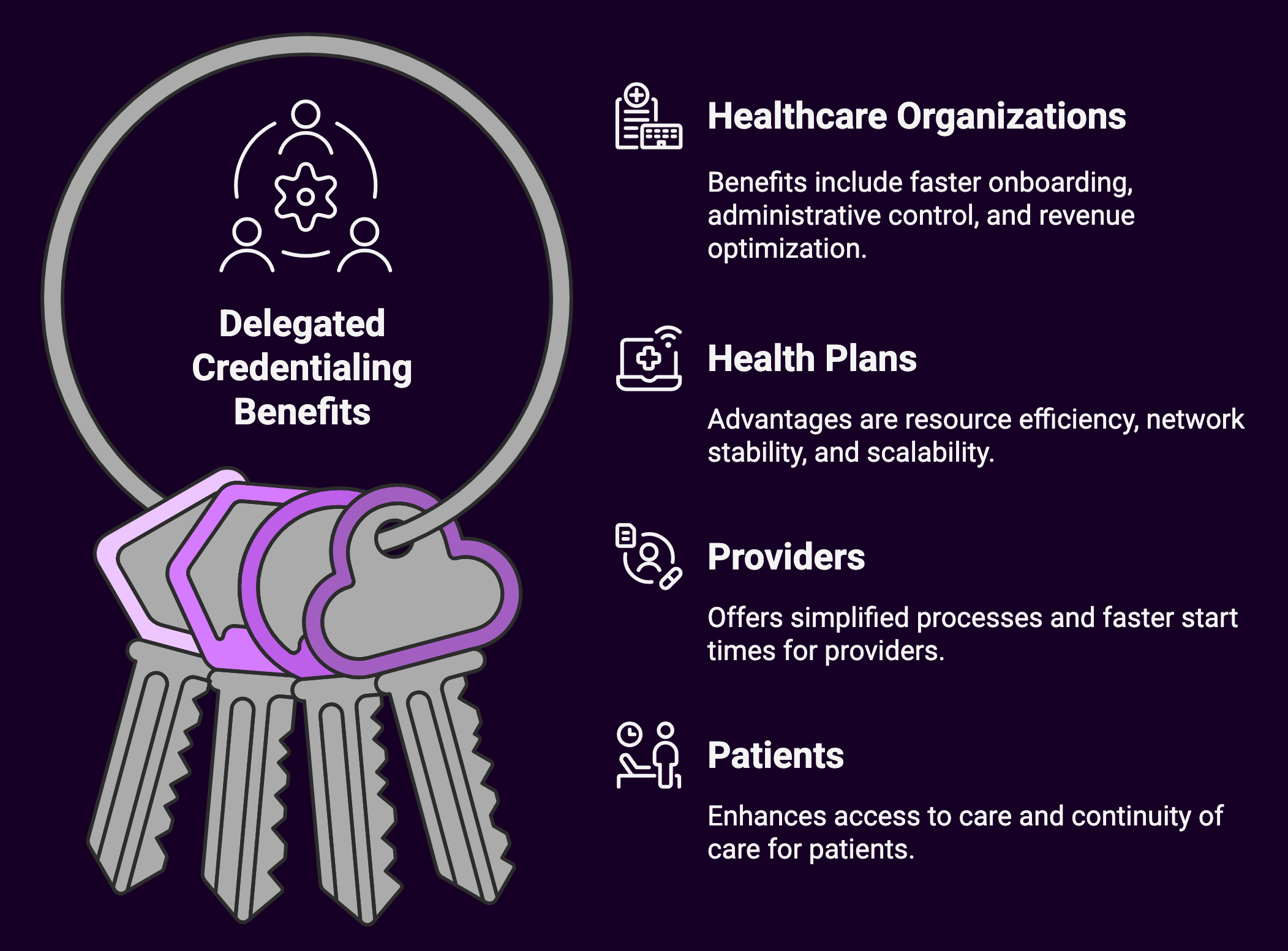
For Healthcare Organizations
- Accelerated Provider Onboarding: Organizations can bring new providers into their networks faster. Reducing the time from hiring to billing from months to weeks.
- Administrative Control: Organizations gain greater control over their credentialing processes rather than being subject to the varying timelines and requirements of multiple health plans.
- Revenue Optimization: Faster credentialing means new providers can begin seeing patients and billing insurance sooner, improving cash flow and reducing gaps in care delivery.
- Streamlined Operations: Centralizing credentialing within the organization creates opportunities for standardization and efficiency, particularly when integrating new practices or providers.
- Competitive Advantage: The ability to credential providers quickly can be a significant recruiting advantage when competing for in-demand specialists.
For Health Plans
- Resource Efficiency: Delegating credentialing responsibilities reduces the administrative burden on health plans, allowing them to allocate resources elsewhere.
- Network Stability: Organizations with delegated authority tend to maintain more stable provider networks with fewer gaps in coverage.
- Focus on Oversight: Rather than managing day-to-day credentialing activities, health plans can focus on quality oversight and ensuring compliance with standards.
- Scalability: As networks grow, delegated credentialing allows health plans to scale their provider networks without proportionally scaling their administrative staff.
For Providers
- Simplified Process: Providers complete one credentialing application rather than submitting similar information to multiple health plans.
- Faster Start Times: Reduced credentialing timelines mean providers can begin seeing patients and generating revenue sooner after joining an organization.
- Local Support: Providers work with their own organization’s credentialing staff, who are often more accessible than health plan representatives.
- Reduced Administrative Burden: Less paperwork and fewer follow-up requests from multiple health plans free up provider time for patient care.
For Patients
- Improved Access to Care: Faster provider credentialing means new physicians can begin seeing patients sooner, reducing wait times and improving access.
- Broader Provider Networks: More efficient credentialing processes can lead to broader provider networks as health plans can add providers more readily.
- Continuity of Care: When providers change organizations, faster credentialing helps minimize disruptions in patient care.
Challenges and Considerations
While delegated credentialing offers significant advantages, it’s not without challenges:
For Healthcare Organizations
- Resource Investment: Organizations must develop robust credentialing departments with specialized staff and technology. An investment that smaller organizations might struggle to justify.
- Regulatory Compliance: Organizations must stay current with evolving credentialing regulations from multiple authorities, including state licensing boards, accreditation bodies, and federal agencies.
- Audit Preparation: Regular preparation for delegation audits requires significant time and resources.
- Technology Requirements: Effective delegated credentialing typically requires sophisticated credentialing software systems.
- Risk Assumption: With authority comes responsibility. Organizations assume liability for credentialing decisions that previously belonged to health plans.
For Health Plans
- Loss of Direct Control: Delegating credentialing means trusting another organization’s processes and decisions.
- Oversight Challenges: Maintaining effective oversight across multiple delegated organizations can be complex.
- Inconsistent Standards: Different delegated organizations may interpret standards differently, creating potential inconsistencies across the network.
- Remediation Difficulties: When problems are identified during audits, implementing corrective actions across independent organizations can be challenging.
Is Delegated Credentialing Right for Every Organization?
Not necessarily.
Organizations should consider several factors before pursuing delegated status:
- Size and Scale: Generally, larger organizations with significant provider volumes benefit most from delegation.
- Infrastructure: Does the organization have the necessary staffing, technology, and processes in place?
- Expertise: Credentialing requires specialized knowledge of regulatory requirements and industry standards.
- Provider Mix: Organizations with high provider turnover or many specialties face more complex credentialing demands.
- Health Plan Relationships: Strong, collaborative relationships with health plans facilitate successful delegation agreements.
- Risk Tolerance: Organizations must be comfortable with the liability associated with credentialing decisions.
The Evolution of Delegated Credentialing
Delegated credentialing has evolved significantly over the past two decades. Early delegation agreements were often informal and focused primarily on basic verification activities. Today’s agreements are comprehensive, covering primary source verification, ongoing monitoring, and even subspecialty credentialing.
Several factors have driven this evolution:
Accreditation Standards
Organizations like the National Committee for Quality Assurance (NCQA), The Joint Commission, and URAC have developed detailed credentialing standards that serve as the foundation for most delegation agreements. These standards continually evolve, requiring delegated organizations to adapt their processes accordingly.
Regulatory Requirements
Federal and state regulations increasingly impact credentialing requirements. The Centers for Medicare and Medicaid Services (CMS) has specific credentialing requirements for Medicare Advantage plans, while states have their own regulations governing provider credentialing timeframes and processes.
Technology Advancements
Modern credentialing software systems have transformed what’s possible in credentialing efficiency. Cloud-based platforms allow for real-time primary source verification, automated monitoring of sanctions and license expiration, and sophisticated reporting capabilities that support delegation requirements.
Consolidation in Healthcare
As healthcare organizations grow through mergers and acquisitions, centralized credentialing becomes increasingly important for operational efficiency. Delegated credentialing allows large systems to standardize processes across multiple locations and provider types.
Emerging Trends in Delegated Credentialing
As we look to the future, several trends are shaping the evolution of delegated credentialing:
Credentials Verification Organizations (CVOs)
Some healthcare organizations are outsourcing their credentialing functions to specialized CVOs while maintaining their delegated status with health plans. This creates a “delegation chain” where the health plan delegates to the healthcare organization, which then subcontracts to the CVO.
Standardization Initiatives
Industry groups are working toward greater standardization in credentialing processes and requirements. Initiatives like the Council for Affordable Quality Healthcare (CAQH) ProView aim to create unified provider data repositories that streamline the credentialing process.
Blockchain for Credentialing
Emerging blockchain solutions promise to create immutable, verifiable records of provider credentials that could be securely shared across organizations, potentially revolutionizing how credentials are verified and monitored.
Telehealth Implications
The rapid expansion of telehealth has created new challenges for credentialing, particularly when providers deliver care across state lines. Organizations with delegated credentialing authority must develop processes for managing interstate licensing and credentialing requirements.
Automated Primary Source Verification
Advances in artificial intelligence and data connectivity are enabling more automated approaches to primary source verification, reducing manual effort and accelerating credentialing timelines.
Best Practices for Successful Delegation
For organizations considering or currently managing delegated credentialing, these best practices can help ensure success:
- Invest in Technology: Modern credentialing software significantly improves efficiency and compliance tracking.
- Standardize Processes: Develop clear, documented workflows that ensure consistency across all credentialing activities.
- Establish Robust Internal Auditing: Don’t wait for health plan audits. Conduct regular internal reviews to identify and address compliance gaps.
- Maintain Detailed Documentation: Comprehensive records are essential for demonstrating compliance during audits.
- Stay Current with Regulatory Changes: Assign responsibility for monitoring evolving credentialing requirements and standards.
- Develop Strong Health Plan Relationships: Regular communication with health plan representatives builds trust and facilitates problem-solving.
- Train Staff Continuously: Ensure credentialing staff receive ongoing education on industry standards and best practices.
- Implement Quality Controls: Multiple checkpoints throughout the credentialing process help catch errors before they become compliance issues.
Summary: The Strategic Value of Delegated Credentialing
 Delegated credentialing represents a strategic capability that enables healthcare organizations to operate more efficiently, respond more quickly to market opportunities, and provide better service to both providers and patients.
Delegated credentialing represents a strategic capability that enables healthcare organizations to operate more efficiently, respond more quickly to market opportunities, and provide better service to both providers and patients.
Since healthcare is progressing toward value-based care models with complex network arrangements, the ability to efficiently manage provider credentials across multiple health plans becomes increasingly important. Organizations that master delegated credentialing gain a significant operational advantage in this environment.
While not without challenges, delegated credentialing offers substantial benefits for healthcare organizations willing to invest in the necessary infrastructure and expertise. For health plans, thoughtful delegation to capable partners can improve network management while reducing administrative costs.
Ultimately, when implemented effectively, delegated credentialing creates a win-win-win scenario: healthcare organizations gain efficiency and control, health plans reduce administrative burden while maintaining standards, and patients benefit from improved access to credentialed providers. This all contributes to a more effective healthcare system.

