The credentialing process stands as one of the most time-consuming administrative tasks in healthcare. For medical practices of any size, the maze of paperwork, verification requirements, and ongoing maintenance can drain valuable resources and delay revenue. Yet credentialing remains non-negotiable. Without proper credentials, providers cannot join insurance networks, submit claims, or receive reimbursement for their services.
The good news? Credentialing doesn’t have to be overwhelming. With the right approach and support, practices can streamline their credentialing operations, reduce administrative burden, and get providers enrolled faster. This article breaks down the credentialing process and offers practical strategies to make it more manageable for your practice.
What Is Provider Credentialing?
 Provider credentialing is the process of verifying that healthcare professionals have the proper qualifications, training, and credentials to provide medical services. Insurance companies, hospitals, and healthcare organizations require this verification before allowing providers to join their networks or treat patients.
Provider credentialing is the process of verifying that healthcare professionals have the proper qualifications, training, and credentials to provide medical services. Insurance companies, hospitals, and healthcare organizations require this verification before allowing providers to join their networks or treat patients.
The credentialing process examines several key areas. These include medical education and training, board certifications, state licenses, work history, malpractice insurance coverage, and any history of sanctions or legal issues. Credentialing organizations verify each piece of information through primary sources, which means they go directly to medical schools, licensing boards, and other official entities rather than simply accepting documents from the provider.
This verification process protects patients by ensuring their doctors meet established standards. It also protects insurance companies and healthcare facilities from liability risks. However, the thoroughness required makes credentialing notoriously slow and paperwork-intensive.
Why Credentialing Takes So Long
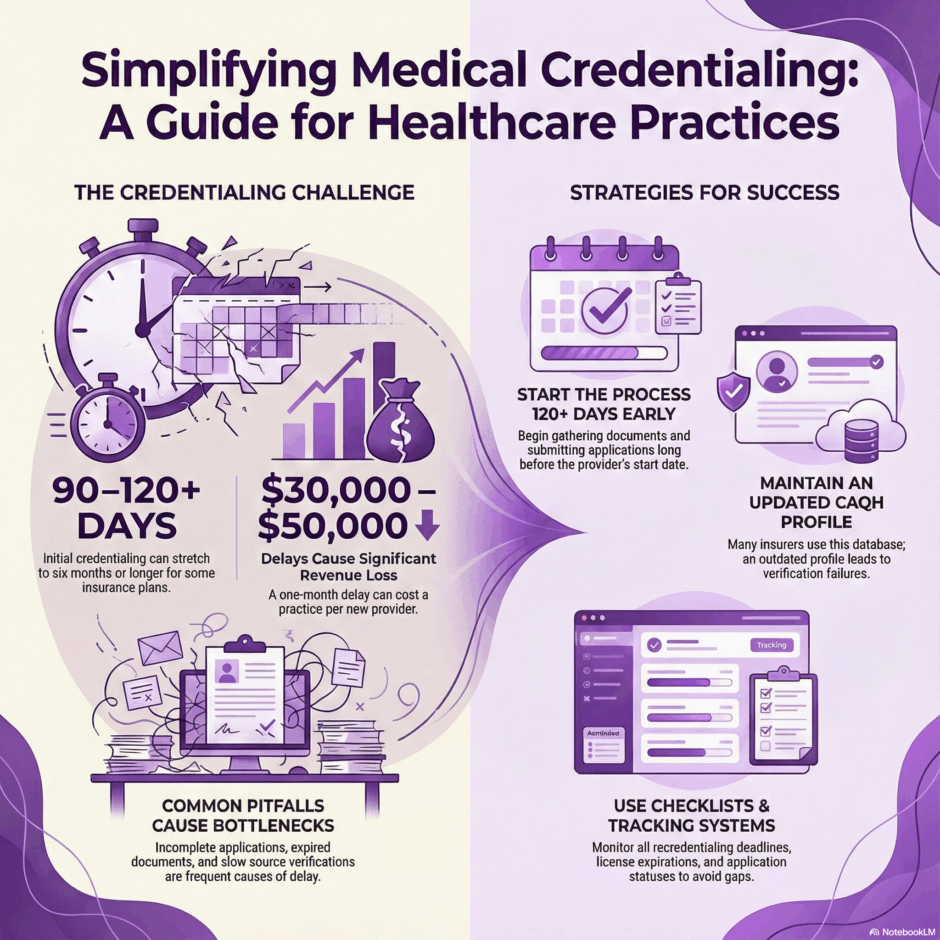
Most providers find the timeline frustrating. Initial credentialing typically takes 90 to 120 days, though it can stretch to six months or longer for certain insurance plans. Several factors contribute to these delays.
- Firstly, the sheer volume of information required is substantial. A single credentialing application might request dozens of documents, references, and data points. Each insurance company has its own application with slightly different requirements, meaning providers often complete multiple lengthy applications for different payers.
- Secondly, primary source verification takes time. When a credentialing organization contacts a medical school to verify a degree from 15 years ago, that school might take weeks to respond. Multiply this across multiple verifications, and delays accumulate quickly.
- Thirdly, incomplete applications are common. Missing documents, expired certifications, gaps in work history, or unsigned forms send applications back to providers for correction. Each round trip adds weeks to the process.
- Finally, insurance companies receive thousands of credentialing applications. Their review committees typically meet monthly or even quarterly, creating natural bottlenecks in the approval pipeline.
The Hidden Costs of Credentialing Delays

When a new provider joins your practice, every day without credentials represents lost revenue. A physician who cannot bill insurance must either see patients without reimbursement or sit idle while the practice pays their salary. For a provider who could generate $30,000 to $50,000 monthly in collections, even a one-month delay represents significant financial loss.
Beyond direct revenue loss, credentialing delays create operational headaches. Staff must explain to patients why their new doctor isn’t in-network yet. Schedules remain partially empty. The provider’s excitement about joining your practice might turn to frustration. In competitive markets, talented providers might even reconsider their decision to join your team.
Recredentialing presents similar challenges. Insurance plans require providers to update their credentials every two to three years. Miss a recredentialing deadline, and the provider gets dropped from the network. This means scrambling to reapply, potential gaps in coverage, and claim denials during the gap period.
Key Steps in the Credentialing Process
While each payer has unique requirements, most credentialing follows a similar pattern. Starting the process early makes a real difference. As soon as you know a provider will join your practice, begin gathering documents. Don’t wait for their start date.
The first step involves collecting provider information. This includes medical school diplomas, residency and fellowship certificates, state medical licenses, DEA certificates, board certifications, CV or work history, professional references, malpractice insurance documentation, and hospital privileges documentation.
Next comes application completion. You’ll submit applications to each insurance plan where you want the provider credentialed. The Council for Affordable Quality Healthcare (CAQH) database helps here. Many insurance companies pull information from CAQH rather than requiring separate applications, so maintaining an updated CAQH profile is crucial.
After submission, the verification phase begins. The credentialing organization contacts medical schools, licensing boards, previous employers, and references to verify the information you provided. They also check the National Practitioner Data Bank for any sanctions or malpractice history.
Once verification is complete, the application goes to the insurance company’s credentialing committee for review. This committee meets on a set schedule, typically monthly. If approved, the provider receives a network participation agreement to sign.
Finally, the practice must complete enrollment steps like setting up the provider in the insurance company’s systems, obtaining a National Provider Identifier (NPI) if the provider doesn’t already have one, and confirming the provider appears in the insurance company’s directory.
Common Credentialing Mistakes to Avoid
 Many practices make avoidable errors that slow credentialing unnecessarily. One frequent mistake is waiting too long to start. Credentialing should begin at least 120 days before the provider’s start date, ideally even earlier. Starting late guarantees your new provider will have an unproductive first few months.
Many practices make avoidable errors that slow credentialing unnecessarily. One frequent mistake is waiting too long to start. Credentialing should begin at least 120 days before the provider’s start date, ideally even earlier. Starting late guarantees your new provider will have an unproductive first few months.
Another common error is submitting incomplete applications. Review every application carefully before submission. Make sure all required documents are attached, all questions are answered, and all signatures are in place. One missing item can delay the entire process by weeks.
Practices also frequently let the CAQH profile go stale. Many providers create their CAQH profile once and forget about it. When licenses renew, certifications update, or addresses change, the CAQH profile must be updated immediately. An outdated profile causes verification failures and application rejections.
Some practices lack a tracking system for credentialing deadlines. Without tracking, it’s easy to miss recredentialing dates or forget to follow up on pending applications. Create a spreadsheet or use practice management software to monitor every provider’s credentialing status with each payer.
Finally, practices sometimes fail to verify that credentialing actually completed. Getting approval is only part of the process. You must confirm the provider is active in the payer’s system, has the correct information in their directory, and that claims will process properly before assuming everything is done.
Strategies for Simpler Credentialing
Several approaches can make credentialing less painful for your practice. Firstly, create a credentialing checklist specific to your providers and locations. Document exactly what each payer requires and the steps in your process. This checklist helps ensure consistency and nothing gets overlooked.
Maintain a credentialing calendar that tracks important dates:
- Initial application submission dates
- Expected completion dates
- Recredentialing due dates
- License and certification expiration dates
- Malpractice insurance renewal dates
- CAQH profile update dates
Set reminders well in advance of each deadline so you have time to gather necessary documents and submit renewals before expiration.
 Build relationships with payer credentialing representatives. Having a contact person at each insurance company makes it easier to check application status, resolve issues, and expedite approvals when possible. Don’t be afraid to follow up regularly on pending applications.
Build relationships with payer credentialing representatives. Having a contact person at each insurance company makes it easier to check application status, resolve issues, and expedite approvals when possible. Don’t be afraid to follow up regularly on pending applications.
Keep digital copies of all credentialing documents organized in a secure location. When it’s time to recredential or apply to a new payer, you’ll have everything at your fingertips rather than scrambling to request documents again.
Consider whether outsourcing makes sense for your practice. Many practices lack the staff expertise or bandwidth to handle credentialing efficiently. Credentialing specialists know payer requirements inside and out, maintain relationships with payer representatives, and can often expedite approvals. For practices that are growing, opening new locations, or hiring multiple providers, outsourcing credentialing can be a smart investment.
Getting Help with Credentialing
Managing credentialing in-house requires dedicated time and expertise. Between initial applications, recredentialing, responding to payer requests, and tracking deadlines, credentialing can easily become a full-time job. For many practices, partnering with a credentialing specialist makes practical sense.
Professional credentialing services bring several advantages. They know the specific requirements for each payer and can ensure applications are complete and accurate the first time. They have established contacts at insurance companies who can provide status updates and help resolve issues quickly. They maintain tracking systems so no deadlines are missed. And they free up your staff to focus on patient care and other practice priorities rather than paperwork.
When evaluating credentialing partners, look for experience with your specialty and the payers most important to your practice. Ask about their average credentialing timelines, how they track progress, and how they communicate with your team. The right partner should make credentialing feel effortless while ensuring providers get enrolled as quickly as possible.
Summary: Credentialing Simplified
 Credentialing may be tedious, but it’s too important to neglect. Your practice’s revenue depends on properly credentialed providers who can bill insurance companies for their services. The key is approaching credentialing systematically rather than reactively.
Credentialing may be tedious, but it’s too important to neglect. Your practice’s revenue depends on properly credentialed providers who can bill insurance companies for their services. The key is approaching credentialing systematically rather than reactively.
Start early, stay organized, maintain accurate records, and don’t hesitate to seek expert help when you need it. With the right processes and support, you can minimize credentialing delays and keep your practice running smoothly.
At Medwave, we specialize in billing, credentialing, and payer contracting services that remove administrative burden from healthcare practices. Our team handles the entire credentialing process from application through approval, ensuring your providers get enrolled quickly and stay current with all recredentialing requirements. This allows you to focus on what matters most: providing excellent patient care while maintaining healthy revenue flow.

