Healthcare has undergone a fundamental shift over the past several decades, moving away from the traditional paternalistic model where doctors made decisions for patients without much input. The healthcare of today increasingly embraces patient-centered care models that place individuals at the heart of their medical journey, recognizing them as active partners rather than passive recipients of treatment.
 This transformation represents more than just a philosophical change, it’s a practical reimagining of how healthcare delivery works. Patient-centered care models prioritize the whole person, not just their medical condition, and seek to align treatment plans with individual values, preferences, and life circumstances.
This transformation represents more than just a philosophical change, it’s a practical reimagining of how healthcare delivery works. Patient-centered care models prioritize the whole person, not just their medical condition, and seek to align treatment plans with individual values, preferences, and life circumstances.
Defining Patient-Centered Care
At its core, patient-centered care is a healthcare approach that respects and responds to individual patient preferences, needs, and values. Rather than following a one-size-fits-all methodology, this model ensures that patient values guide all clinical decisions. The approach recognizes that effective healthcare requires collaboration between patients, families, and healthcare providers.
The Institute of Medicine defines patient-centered care as “care that is respectful of and responsive to individual patient preferences, needs, and values and ensures that patient values guide all clinical decisions.” This definition highlights the collaborative nature of modern healthcare relationships and emphasizes the importance of treating each person as a unique individual with distinct circumstances and goals.
Core Principles of Patient-Centered Care
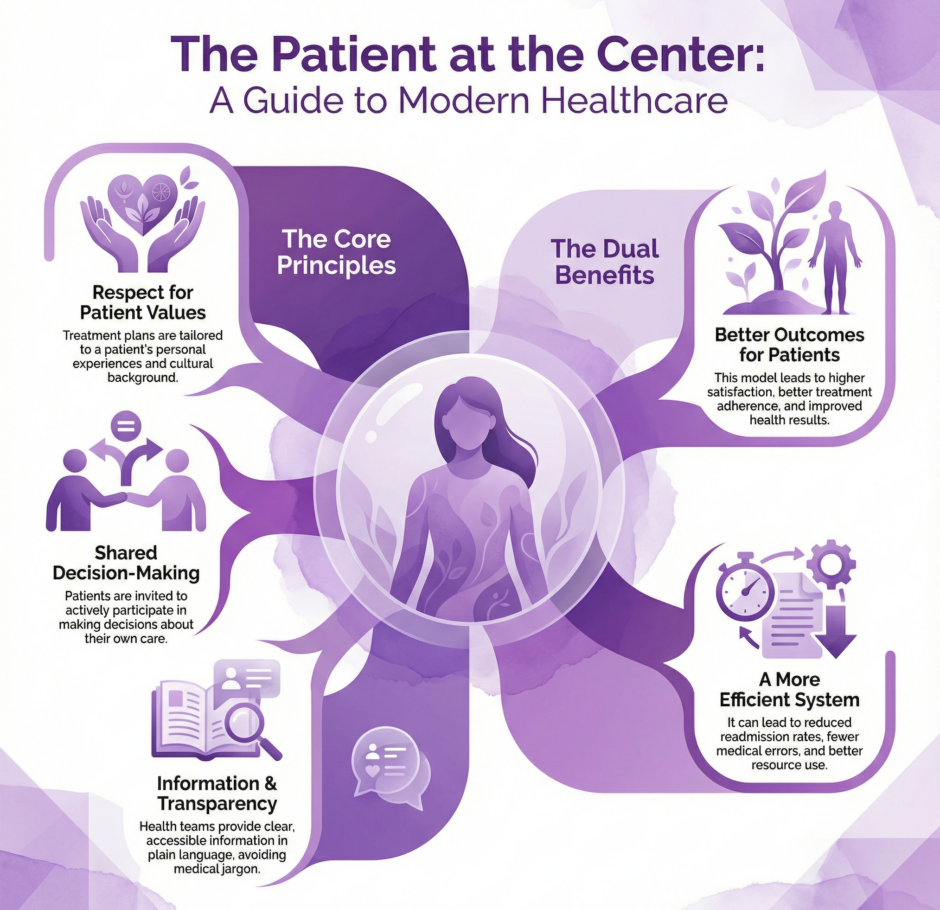
Patient-centered care models operate on several fundamental principles that distinguish them from traditional healthcare approaches:
- Respect for Patient Values and Preferences
Healthcare providers acknowledge that patients bring their own perspectives, cultural backgrounds, and personal experiences to their medical care. Treatment plans are developed with consideration for these individual factors, ensuring that recommendations align with what matters most to each person. - Information Sharing and Transparency
Patients receive clear, accessible information about their health conditions, treatment options, and potential outcomes. Healthcare teams communicate in plain language, avoiding medical jargon that might create barriers to comprehension. - Participation in Care Decisions
Rather than being told what to do, patients are invited to actively participate in making decisions about their care. This includes discussing various treatment options, weighing benefits and risks, and considering how different approaches might fit into their daily lives. - Coordination and Integration
Patient-centered care models emphasize seamless coordination between different healthcare providers, departments, and services. This integration ensures that patients don’t fall through cracks in the system and that all aspects of their care work together harmoniously.
Key Components of Patient-Centered Care Models
Several essential components work together to create effective patient-centered care environments:
- Individualized care plans that reflect personal goals and circumstances
- Shared decision-making processes that involve patients as equal partners
- Cultural competency training for healthcare staff to serve diverse populations
- Family and caregiver involvement when appropriate and desired by the patient
- Accessible communication channels that accommodate different preferences and abilities
- Continuity of care across different providers and settings
- Patient education resources tailored to individual learning styles and needs
These components create a framework that supports personalized healthcare delivery while maintaining clinical excellence and safety standards.
Benefits for Patients and Healthcare Systems
 Patient-centered care models offer significant advantages for both individuals receiving care and the healthcare organizations providing it. For patients, these models often result in higher satisfaction scores, better adherence to treatment plans, and improved health outcomes. When people feel heard and respected by their healthcare team, they’re more likely to engage actively in their care and follow through with recommendations.
Patient-centered care models offer significant advantages for both individuals receiving care and the healthcare organizations providing it. For patients, these models often result in higher satisfaction scores, better adherence to treatment plans, and improved health outcomes. When people feel heard and respected by their healthcare team, they’re more likely to engage actively in their care and follow through with recommendations.
From a healthcare system perspective, patient-centered approaches can lead to reduced readmission rates, decreased medical errors, and more efficient use of resources. When patients are well-informed and engaged, they’re better equipped to manage their health conditions independently, potentially reducing the need for emergency interventions or repeated visits.
Research consistently demonstrates that patient-centered care correlates with improved clinical outcomes across various medical conditions. Patients who participate actively in their care decisions tend to experience better pain management, faster recovery times, and higher overall satisfaction with their healthcare experience.
Implementation Strategies
Transitioning to patient-centered care models requires deliberate planning and systematic changes across healthcare organizations. Leadership commitment is essential, as this transformation affects every aspect of how care is delivered.
- Staff Training and Development
Healthcare professionals need training in communication skills, cultural competency, and shared decision-making techniques. This education helps providers develop the skills necessary to engage effectively with patients from diverse backgrounds and with varying levels of health literacy. - Technology Integration
Modern patient-centered care often relies on technology to facilitate communication and information sharing. Electronic health records, patient portals, and telemedicine platforms can enhance the patient experience by providing convenient access to health information and care team communication. - Physical Environment Design
The physical layout of healthcare facilities plays a role in supporting patient-centered care. Design elements that promote privacy, comfort, and family involvement help create environments where patients feel respected and supported. - Policy and Procedure Updates
Healthcare organizations must review and revise policies to align with patient-centered principles. This might include changes to visiting hours, family involvement protocols, and communication standards.
Challenges and Barriers
Despite the clear benefits, implementing patient-centered care models faces several obstacles that healthcare organizations must address:
- Time Constraints
Healthcare providers often work under significant time pressures, making it challenging to engage in lengthy discussions with patients about their preferences and values. Organizations must find ways to build meaningful patient interaction time into workflow processes. - Resource Limitations
Patient-centered care sometimes requires additional resources, including staff training, technology investments, and potentially longer appointment times. Healthcare organizations must balance these costs against the long-term benefits of improved patient outcomes and satisfaction. - Cultural Resistance
Some healthcare professionals may resist changes to traditional practice patterns, particularly those who are accustomed to more paternalistic approaches. Change management strategies must address these cultural barriers and help staff embrace new ways of delivering care. - Regulatory and Payment Challenges
Current healthcare payment models don’t always incentivize patient-centered approaches, potentially creating financial barriers to implementation. Organizations must navigate these constraints while working toward more patient-focused care delivery.
Measuring Success in Patient-Centered Care
Evaluating the effectiveness of patient-centered care models requires multiple metrics that capture both clinical outcomes and patient experience measures:
- Patient satisfaction scores and feedback
- Clinical quality indicators and health outcomes
- Patient engagement levels and care plan adherence
- Communication effectiveness ratings
- Care coordination metrics
- Patient safety indicators
- Staff satisfaction and retention rates
These measurements help healthcare organizations identify areas for improvement and demonstrate the value of patient-centered approaches to stakeholders, including patients, staff, and leadership.
Summary: Patient-Centered Care Models are the Future
 The future of patient-centered care models looks toward increased personalization and technology integration. Artificial intelligence and machine learning tools may help healthcare providers better tailor treatments to individual patient characteristics and preferences. Mobile health applications and wearable devices are creating new opportunities for patients to actively monitor their health and communicate with their care teams.
The future of patient-centered care models looks toward increased personalization and technology integration. Artificial intelligence and machine learning tools may help healthcare providers better tailor treatments to individual patient characteristics and preferences. Mobile health applications and wearable devices are creating new opportunities for patients to actively monitor their health and communicate with their care teams.
Precision medicine approaches are becoming more sophisticated, allowing for treatment plans that consider individual genetic profiles, lifestyle factors, and personal preferences. These advances promise to make patient-centered care even more individualized and effective.
Healthcare organizations are also exploring new models of care delivery, such as medical homes and accountable care organizations, that emphasize coordination and patient-centered approaches across different providers and settings.

