Ready to join the Anthem provider network? You’re in the right place. As one of America’s largest health benefits companies, Anthem reaches millions of patients across the country through Medicare Advantage plans, Medicaid managed care programs, and commercial health insurance products. Getting credentialed with Anthem opens doors to a massive patient base and significant revenue opportunities for your practice.
 Anthem serves over 47 million members across 25 states and Washington D.C. Their Medicare Advantage plans alone cover approximately 2.7 million seniors, while their Medicaid programs provide care to over 8 million individuals and families. Add in the millions more who receive coverage through employer-sponsored commercial plans, and you can see why joining this network is such a valuable move for healthcare providers.
Anthem serves over 47 million members across 25 states and Washington D.C. Their Medicare Advantage plans alone cover approximately 2.7 million seniors, while their Medicaid programs provide care to over 8 million individuals and families. Add in the millions more who receive coverage through employer-sponsored commercial plans, and you can see why joining this network is such a valuable move for healthcare providers.
In this guide, we’ll walk you through everything you need to know about Anthem credentialing. From gathering your initial documents to maintaining your credentials over time, we’ve got you covered. Whether you’re a solo practitioner or part of a larger medical group, this information will help you get through the credentialing process smoothly and set you up for long-term participation in the Anthem network.
What Anthem Looks For in Providers
Anthem takes a whole-health approach to patient care, which means they’re looking for providers who share that vision. They want healthcare professionals who prioritize quality outcomes, meet high standards of excellence, and stay on top of regulatory requirements. Whether you’re applying to participate in their Medicare, Medicaid, or commercial networks, Anthem expects you to maintain proper licensing, demonstrate quality care delivery, and follow state-specific regulations.
The company also pays close attention to network adequacy standards. This means they consider geographic coverage, specialty availability, and access to care when reviewing applications. If your practice fills a need in their network, whether that’s based on location, specialty, or patient population served, you’ll likely find the credentialing process goes more smoothly.
Getting Your Documentation Ready
Before you even start your application, you need to gather the right paperwork. Think of this as building your professional portfolio. Anthem requires specific documents that verify your qualifications, training, and ability to practice medicine safely.
Here’s what you’ll need to have on hand:
Core Professional Documents
- Current state medical license (and any additional state licenses if you practice in multiple locations)
- DEA registration if you prescribe controlled substances
- Board certification in your specialty
- Professional liability insurance policy with adequate coverage limits
- Five years of work history with no unexplained gaps
- Verification of your medical education and training
- A government-issued photo ID
- Your National Provider Identifier (NPI)
- Medicare and Medicaid provider numbers if applicable
- Tax identification documents
Anthem-Specific Materials
- Hospital affiliation documentation showing where you have admitting privileges
- After-hours coverage arrangements for your patients
- Information about your electronic health records system
- Agreements to participate in quality measure reporting
- State-specific network participation forms
One of the most important pieces of the puzzle is your CAQH ProView Profile. This is a centralized database that stores all your credentialing information, and Anthem pulls data directly from it. Make sure your CAQH profile is 100% complete and up-to-date before you submit your Anthem application. Missing or outdated information in CAQH is one of the most common reasons for credentialing delays. Additionally, we created our own CAQH ProView Form to assist providers with the CAQH process.
Using the Anthem Provider Portal

Anthem has an online provider portal that serves as your home base throughout the credentialing process. You’ll register for an account, complete your provider profile, and submit all your documentation through this system. The portal also lets you track your application status, update your information, and communicate with Anthem’s credentialing team.
Once you’re set up in the portal, you’ll upload all your required documents, submit W-9 forms, and complete enrollment materials specific to the Anthem networks you want to join. The interface is fairly straightforward, but make sure you save copies of everything you upload. Keep detailed records of when you submitted each document and any confirmation numbers you receive.
The portal isn’t just for initial credentialing either. You’ll use it throughout your relationship with Anthem to update demographic information, manage your network participation, and access claims and payment information.
Walking Through the Credentialing Steps
The Anthem credentialing process happens in distinct phases, and knowing what to expect at each stage helps you stay organized and avoid delays.
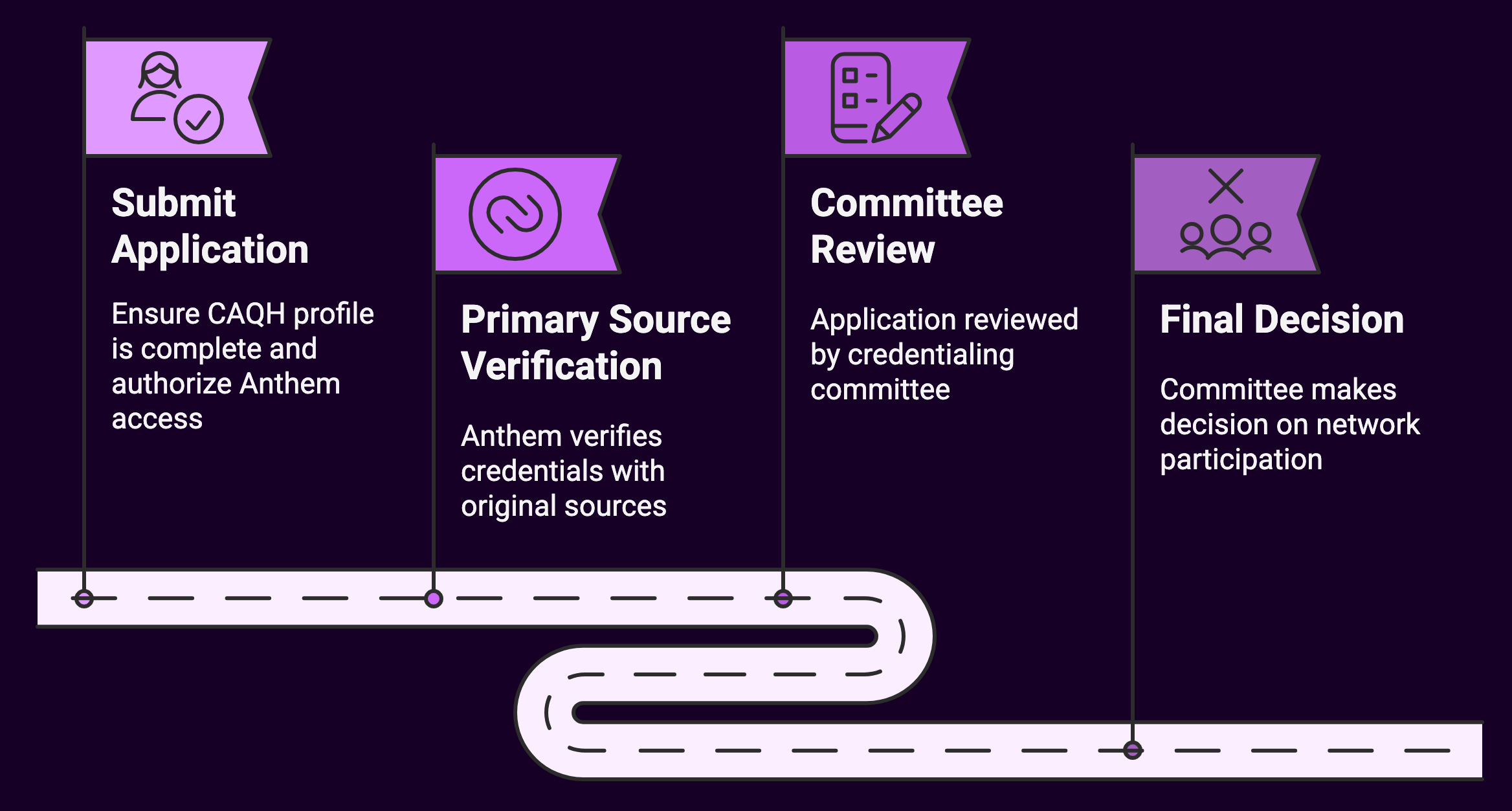
Phase One: Submitting Your Application
Start by making sure your CAQH profile is complete and current. Then authorize Anthem to access your CAQH information. You’ll also need to complete Anthem-specific enrollment forms and provide supporting documentation that goes beyond what’s in CAQH. Different states may have additional requirements, so check what’s needed for the specific locations where you practice.
Phase Two: Primary Source Verification
This is where Anthem does their homework on you. They verify everything directly with the original sources. They’ll check your medical license with the state medical board, confirm your education with your medical school, verify your residency and fellowship training, and check the status of your board certifications. They’ll also look into your work history to make sure there are no unexplained gaps, review any malpractice claims or settlements, confirm your DEA registration, and check federal databases to ensure you haven’t been sanctioned or excluded from Medicare or Medicaid.
This verification process typically takes 60 to 90 days. It’s the longest part of credentialing, but there’s not much you can do to speed it up. Just make sure all your information is accurate from the start so nothing comes back with discrepancies that need to be resolved.
Phase Three: Committee Review
After verification is complete, your application goes before a credentialing committee. These committees meet regularly to review applications and make decisions about network participation. They look at your verification results, quality indicators, compliance history, professional references, and any history of disciplinary actions. They also consider network adequacy needs, basically, whether Anthem needs providers with your specialty in your geographic area.
Phase Four: Final Decision
The credentialing committee will make one of several decisions. You might receive full approval to join the network, or you might get conditional approval that comes with specific requirements you need to meet. Sometimes the committee asks for additional information before making a final decision. In some cases, applications are denied, but you have the right to appeal if that happens.
Special Requirements for Medicare and Medicaid
If you’re planning to see Anthem Medicare Advantage patients, there are additional hoops to jump through. You need to be enrolled as a Medicare provider, participate in quality reporting programs, and engage with the Medicare Star Ratings program. Anthem also wants to know about your experience with special needs populations, especially if you’ll be serving seniors with chronic conditions. You’ll need to complete compliance training specific to Medicare regulations and get familiar with prior authorization protocols for Medicare Advantage plans.
Medicaid participation comes with its own set of requirements too. You need to be enrolled in your state’s Medicaid program and sign managed care organization agreements. States have access standards that dictate how quickly patients need to be able to get appointments, and you’ll need to meet those standards. Cultural competency training is often required, along with demonstration that you can serve special populations like pregnant women, children with special healthcare needs, or individuals with disabilities.
Smart Strategies for a Smooth Process
 Organization is your best friend during credentialing. Set up a digital filing system where you organize documents by category. Track expiration dates for licenses, certifications, and insurance policies so nothing lapses while your application is being reviewed. Use consistent file naming conventions so you can find things quickly, and keep backup copies of everything in at least two places.
Organization is your best friend during credentialing. Set up a digital filing system where you organize documents by category. Track expiration dates for licenses, certifications, and insurance policies so nothing lapses while your application is being reviewed. Use consistent file naming conventions so you can find things quickly, and keep backup copies of everything in at least two places.
Communication matters just as much as documentation. Designate one person in your practice as the primary contact for credentialing matters. Document every phone call, email, and interaction you have with Anthem’s credentialing team. Use official communication channels, the provider portal and designated email addresses, rather than trying to reach out through informal channels. Follow up regularly on your application status, but don’t be a pest. A status check every two to three weeks is reasonable during the verification phase.
Start early. The entire credentialing process from application submission to final approval typically takes 90 to 120 days, though it can be longer if there are complications. If you’re planning to join the Anthem network, begin the process at least four months before you actually need to start seeing Anthem patients. This buffer gives you room to handle any unexpected delays or requests for additional information.
Keeping Your Credentials Current
Getting credentialed is just the beginning. Staying credentialed requires ongoing maintenance. You need to attest to your CAQH profile at least quarterly, which means logging in and confirming that all your information is still accurate. Track renewal dates for your medical license, DEA registration, board certifications, and liability insurance. Don’t wait until the last minute, start the renewal process well before expiration dates.
Any significant changes to your practice need to be reported to Anthem promptly.
This includes:
- Moving to a new practice location or adding a new office
- Changes to your phone number, fax number, or email address
- Adding or losing physicians in your practice
- Expanding or reducing the services you offer
- Changes to your after-hours coverage arrangements
- Modifications to your practice ownership or corporate structure
Failing to report changes can create problems with claims processing, patient access, and even your network participation status.
Handling Common Problems
 Even with careful preparation, issues can pop up during credentialing. Application delays are frustrating but common. If your application seems stuck, first check that your CAQH profile is complete and current. Log into the provider portal to see if there are any status updates or requests for information you might have missed. If everything looks good on your end, reach out to the provider relations department for a status update. Keep documentation of all your attempts to get information.
Even with careful preparation, issues can pop up during credentialing. Application delays are frustrating but common. If your application seems stuck, first check that your CAQH profile is complete and current. Log into the provider portal to see if there are any status updates or requests for information you might have missed. If everything looks good on your end, reach out to the provider relations department for a status update. Keep documentation of all your attempts to get information.
Information discrepancies can really slow things down. Maybe your CAQH profile lists one address for your medical school but the school’s records show a different address. Or perhaps there’s a date mismatch in your employment history. When discrepancies come up, review all your submitted information carefully, update your CAQH profile with the correct information, and submit documentation that clarifies the discrepancy. Follow up to make sure Anthem received your corrections and document everything.
Quality and Compliance Expectations
Anthem takes quality measurement seriously. Once you’re in the network, you’ll participate in HEDIS measure reporting, patient satisfaction surveys, and clinical quality indicator tracking. You’ll need to meet standards for patient access and availability, engage in preventive care initiatives, and participate in care coordination programs. These are ongoing requirements of network participation.
Compliance is equally important. You need to stay current with Medicare and Medicaid regulations, state insurance department standards, and HIPAA privacy and security rules. Anthem monitors for fraud and abuse, so make sure your billing practices are squeaky clean. Quality reporting isn’t optional, and you need to help Anthem meet network adequacy standards by maintaining appropriate office hours and accepting new patients as agreed.
Resources You Can Tap Into
 You’re not alone in this process. Anthem has a provider relations department specifically designed to help network providers. They can answer questions about credentialing, network participation, and policy changes. There’s also a credentialing services team that handles the nuts and bolts of application processing. For quality programs, there’s a dedicated team that can help you with measure reporting and quality improvement initiatives. If you’re participating in Medicare or Medicaid networks, there are specialists who focus on those programs.
You’re not alone in this process. Anthem has a provider relations department specifically designed to help network providers. They can answer questions about credentialing, network participation, and policy changes. There’s also a credentialing services team that handles the nuts and bolts of application processing. For quality programs, there’s a dedicated team that can help you with measure reporting and quality improvement initiatives. If you’re participating in Medicare or Medicaid networks, there are specialists who focus on those programs.
Online resources are available too. The Anthem Provider Portal is your main hub, but you’ll also work with the CAQH ProView platform. State Medicaid agency websites have information about state-specific requirements, and Medicare has extensive provider resources on their website. Anthem publishes materials about their quality programs that can help you prepare for participation.
Setting Yourself Up for Long-Term Success
Think of credentialing as the start of a long-term relationship, not a one-time event. Get to know your provider relations representative and don’t hesitate to reach out when you have questions. Attend Anthem training session, they often offer updates on policy changes, quality programs, and network expectations. Consider participating in provider advisory groups where you can give feedback and learn from other providers in the network.
Stay informed about policy updates by reading communications from Anthem carefully. They send out provider bulletins, newsletters, and policy updates that contain important information about changing requirements, new programs, and network expectations. Set aside time regularly to review these communications rather than letting them pile up in your inbox.
When it comes to recredentialing, preparation is everything. Anthem recredentials providers every three years, and you should start preparing at least six months before your recredentialing date. Update all your documentation, complete your CAQH attestation, and review your quality performance metrics. If there are any compliance issues or concerns, address them proactively. Make sure your continuing education is current and that you’ve completed any required training.
State and Network Considerations
 If you practice in multiple states or participate in different Anthem networks, remember that requirements can vary significantly. Each state has different licensing requirements and Medicaid program rules. Quality measures might differ by state, and network needs vary based on local demographics and existing provider availability. Make sure you’re familiar with the specific requirements for each state and network where you want to participate.
If you practice in multiple states or participate in different Anthem networks, remember that requirements can vary significantly. Each state has different licensing requirements and Medicaid program rules. Quality measures might differ by state, and network needs vary based on local demographics and existing provider availability. Make sure you’re familiar with the specific requirements for each state and network where you want to participate.
Geographic coverage requirements mean Anthem looks at where providers are located to ensure adequate access to care across their service areas. Specialty availability standards ensure that patients can access specialists within reasonable distances and timeframes. Access time standards dictate how soon patients should be able to get appointments. If you’re going to provide after-hours coverage or offer services in languages other than English, Anthem will factor that into their network adequacy planning.
Working with Medwave
 Credentialing with Anthem doesn’t have to be overwhelming. At Medwave, we handle billing, credentialing, and payer contracting for healthcare providers like you. We know the Anthem credentialing process inside and out, and we can manage everything from initial application to ongoing credential maintenance. Let us handle the paperwork, follow-ups, and compliance tracking so you can focus on patient care.
Credentialing with Anthem doesn’t have to be overwhelming. At Medwave, we handle billing, credentialing, and payer contracting for healthcare providers like you. We know the Anthem credentialing process inside and out, and we can manage everything from initial application to ongoing credential maintenance. Let us handle the paperwork, follow-ups, and compliance tracking so you can focus on patient care.
Getting credentialed with Anthem opens up significant opportunities for your practice. With the right preparation, organization, and support, you can move through the process smoothly and build a productive long-term relationship with one of America’s largest health insurance networks. Keep this guide handy as a reference, stay proactive about maintaining your credentials, and don’t hesitate to reach out for help when you need it.

