Healthcare providers face mounting pressure to optimize their revenue streams while maintaining quality patient care. At the heart of this challenge lies payer contract management, a critical function that directly influences both financial sustainability and patient access to services. Knowing how to negotiate, manage, and optimize these agreements can mean the difference between thriving and merely surviving in today’s healthcare terrain.
Payer Contract Management Essentials
 Payer contract management encompasses the entire lifecycle of agreements between healthcare providers and insurance organizations. This process begins long before the first signature and continues well after implementation, requiring ongoing monitoring, analysis, and adjustment. These contracts serve as the foundation for how providers receive payment for their services and how patients access care within their insurance networks.
Payer contract management encompasses the entire lifecycle of agreements between healthcare providers and insurance organizations. This process begins long before the first signature and continues well after implementation, requiring ongoing monitoring, analysis, and adjustment. These contracts serve as the foundation for how providers receive payment for their services and how patients access care within their insurance networks.
The stakes are high in these negotiations. A poorly structured contract can result in years of inadequate reimbursement, while a well-negotiated agreement can provide stable revenue and attract more patients to the practice. Healthcare administrators must approach these contracts with the same strategic mindset they would apply to any major business decision.
Key Components of Payer Contracts
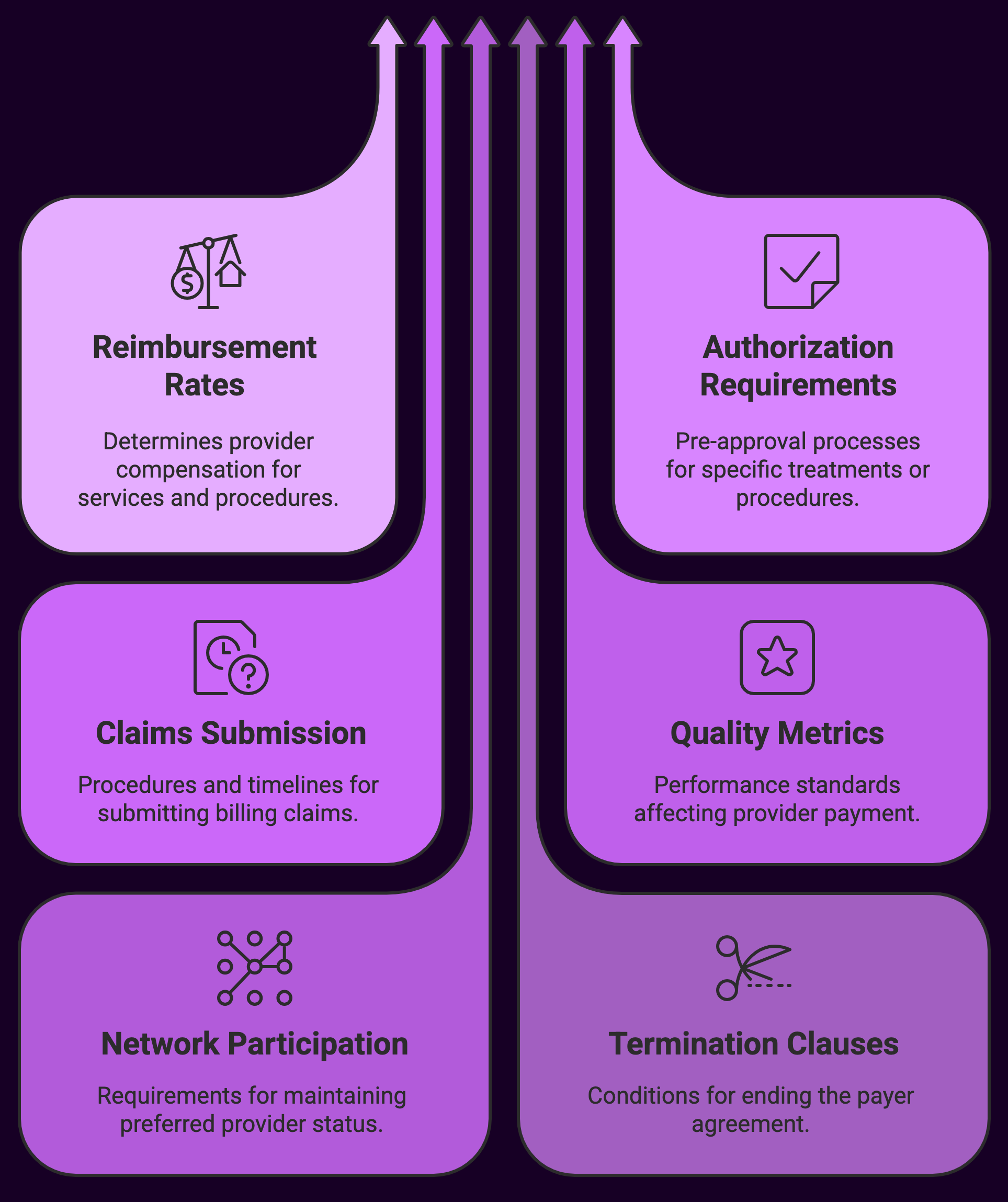
Every payer contract contains several essential elements that healthcare providers must understand thoroughly:
- Reimbursement rates and fee schedules – These determine how much providers receive for specific services and procedures
- Authorization requirements – Pre-approval processes for certain treatments or procedures
- Claims submission protocols – Specific procedures and timelines for billing
- Quality metrics and reporting obligations – Performance standards that may affect payment
- Network participation terms – Requirements for maintaining preferred provider status
- Termination clauses – Conditions under which either party can end the agreement
The reimbursement structure often represents the most critical component. Providers may encounter various payment models, from traditional fee-for-service arrangements to value-based care contracts that tie compensation to patient outcomes. Each model presents unique opportunities and risks that require careful evaluation.
Authorization requirements can significantly impact practice workflow and patient satisfaction. Some contracts require pre-authorization for routine procedures, while others only mandate approval for high-cost treatments.
The Contract Negotiation Process
Contract negotiations require thorough preparation and strategic thinking. Providers must analyze their current performance data, understand market conditions, and identify their negotiating strengths before entering discussions with payers.
Pre-negotiation preparation steps include:
- Analyzing current contract performance and identifying problem areas
- Gathering data on patient volume, procedure frequency, and revenue by payer
- Researching market rates and competitor agreements where possible
- Identifying unique value propositions that differentiate the practice
- Setting clear objectives and minimum acceptable terms
During negotiations, providers should focus on more than just reimbursement rates. Payment timing, administrative burden, and quality reporting requirements can all impact the true value of a contract. A higher reimbursement rate means little if the administrative costs of compliance eat into the additional revenue.
Quality metrics increasingly influence contract terms. Many payers now include performance bonuses or penalties based on patient satisfaction scores, clinical outcomes, or efficiency measures. Providers must evaluate whether they can realistically meet these standards and whether the potential rewards justify the additional effort required.
Technology and Contract Management
 Modern contract management relies heavily on technology solutions to track performance, identify issues, and optimize revenue. Electronic health record systems can integrate with contract management platforms to provide real-time visibility into how well providers are performing under their various agreements.
Modern contract management relies heavily on technology solutions to track performance, identify issues, and optimize revenue. Electronic health record systems can integrate with contract management platforms to provide real-time visibility into how well providers are performing under their various agreements.
Automated reporting tools help practices stay compliant with quality reporting requirements while reducing administrative burden. These systems can flag potential problems before they become costly issues, such as claims that may be denied due to authorization requirements or coding errors.
Data analytics play an increasingly important role in contract evaluation. Analyzing patterns in claim denials, payment delays, and authorization approvals allows providers to identify which contracts provide the best overall value. This information becomes invaluable during renewal negotiations or when deciding whether to participate in new networks.
Performance Monitoring and Optimization
Once contracts are in place, ongoing monitoring becomes essential. Many providers make the mistake of signing agreements and then forgetting about them until renewal time. This passive approach often results in missed opportunities and unaddressed problems that compound over time.
Key performance indicators to monitor regularly include:
- Claim denial rates by payer and procedure type
- Average payment turnaround times
- Authorization approval rates and processing speeds
- Patient satisfaction with insurance-related processes
- Overall revenue per encounter by payer
- Administrative costs associated with each contract
Regular performance reviews allow providers to identify trends and address issues proactively. For example, a sudden increase in claim denials might indicate changes in payer policies that require adjustments to billing practices. Similarly, longer payment processing times might signal the need for follow-up on outstanding claims.
Common Challenges and Solutions
 Healthcare providers face numerous challenges in managing payer contracts effectively. Knowledge of these common pitfalls and their solutions can help practices avoid costly mistakes and optimize their contract portfolio.
Healthcare providers face numerous challenges in managing payer contracts effectively. Knowledge of these common pitfalls and their solutions can help practices avoid costly mistakes and optimize their contract portfolio.
Authorization delays represent one of the most frequent sources of frustration. Patients may experience treatment delays while waiting for insurance approval, leading to dissatisfaction and potential health risks. Providers can address this challenge by implementing robust authorization tracking systems and maintaining open communication with both payers and patients about approval status.
Claim denials create administrative burden and cash flow problems. Many denials result from preventable issues such as coding errors, missing documentation, or failure to obtain proper authorizations. Investing in staff training and quality assurance processes can significantly reduce denial rates and improve overall revenue cycle performance.
Contract complication often overwhelms smaller practices that lack dedicated administrative staff. These providers may benefit from outsourcing contract management to specialized firms or investing in software solutions that simplify tracking and compliance.
Financial Impact Assessment
Knowing the true financial impact of payer contracts requires looking beyond simple reimbursement. Providers must consider the total cost of participation, including administrative expenses, quality reporting requirements, and opportunity costs.
Some contracts may offer attractive reimbursement, yet require extensive documentation that increases overhead costs. Others might provide lower rates but streamlined processes that reduce administrative burden. The net effect on practice profitability depends on the specific circumstances and capabilities of each provider organization.
Cash flow considerations also play a crucial role in contract evaluation. Payers with slow payment processing can strain practice finances, even if their reimbursement is competitive. Providers must balance the need for prompt payment against the desire to participate in networks with large patient populations.
Future Trends in Payer Contracting
 The healthcare industry continues to shift toward value-based payment models that reward quality and efficiency over volume. This transition requires providers to adapt their contract management strategies and develop new capabilities for measuring and reporting outcomes.
The healthcare industry continues to shift toward value-based payment models that reward quality and efficiency over volume. This transition requires providers to adapt their contract management strategies and develop new capabilities for measuring and reporting outcomes.
Artificial intelligence and machine learning technologies are beginning to influence contract management processes. These tools can analyze vast amounts of data to identify optimization opportunities and predict future performance trends. Early adopters of these technologies may gain significant competitive advantages in negotiations.
Patient satisfaction metrics are becoming increasingly important in contract terms. Payers recognize that satisfied patients are more likely to engage with their care and achieve better outcomes, leading to lower overall costs. Providers who excel in patient experience may find themselves in stronger negotiating positions.
Building Internal Capabilities
Managing payer contracts effectively requires dedicated resources and expertise. Larger healthcare organizations often have specialized teams focused on contract management, while smaller practices may need to develop these capabilities gradually or consider outsourcing options.
Staff training plays a critical role in contract management. Team members who understand authorization requirements, billing procedures, and quality metrics can help ensure compliance and optimize performance under each agreement. Regular training updates become necessary as contracts change and new requirements emerge.
Documentation and process standardization help practices maintain consistency across different payer relationships. Clear procedures for handling authorizations, submitting claims, and responding to denials reduce errors and improve efficiency.
Strategic Considerations
Payer contract management must align with broader organizational strategy and goals. Practices focused on growth may prioritize contracts that provide access to large patient populations, even if reimbursement is modest. Organizations emphasizing high-end services might seek contracts that recognize their specialized capabilities with premium payments.
Geography also influences contract strategy. Providers in competitive markets may have more negotiating leverage, while those in underserved areas might need to accept less favorable terms to ensure adequate patient access to care.
The relationship between contract management and practice development deserves careful attention. Contracts that support the practice’s clinical strengths and strategic direction provide more value than those that simply offer competitive reimbursement for services the practice rarely performs.
Summary: A Payer Contract Management Strategy
 Effective payer contracting represents a critical competency for healthcare providers in today’s market environment. The process requires ongoing attention, strategic thinking, and continuous improvement to optimize both financial performance and patient care delivery.
Effective payer contracting represents a critical competency for healthcare providers in today’s market environment. The process requires ongoing attention, strategic thinking, and continuous improvement to optimize both financial performance and patient care delivery.
Providers who invest in developing strong contract management capabilities position themselves for long-term stability and growth, while those who neglect this function may find themselves struggling to maintain viable operations.
The key lies in treating contract management as an integral part of practice strategy rather than simply an administrative necessity.
Contact us, we can assist with any payer contracting need and/or challenge.

