If you’re a healthcare provider, you probably groan at the memory of the credentialing process. Stacks of paperwork, endless verification calls, and waiting and more waiting…The average provider credentialing process takes between 60 to 120 days. That’s three to four months of potential patient care and revenue lost to administrative overhead.
What if we told you that the future of credentialing is already here, and it looks nothing like the paper-pushing nightmare we’ve all come to dread? Let’s discuss how blockchain, artificial intelligence, and other emerging technologies are revolutionizing the way we verify healthcare credentials.
The Current Credentialing Conundrum
Before we look into the future, let’s acknowledge just how broken the present system is, currently.
Today’s credentialing process typically involves:
- Providers manually completing lengthy applications
- Staff verifying credentials with multiple primary sources
- Hospital committees reviewing applications
- Insurance companies conducting their own separate verifications
- State licensing boards maintaining yet another database
All these steps happen in silos, creating redundancies that cost the healthcare industry billions each year. A single provider might go through this process dozens of times throughout their career, with each organization essentially redoing the same verification work.
The inefficiency isn’t just annoying, it’s dangerous. Delayed credentialing means delayed care. It means qualified providers sitting on the sidelines while patients wait for appointments. It means hospitals lose money and insurers create unnecessary bottlenecks.
Enter Blockchain: The Credentialing Game-Changer
Think of blockchain as a digital ledger that can’t be altered without consensus. Once information is entered, it’s there permanently and transparently. For credentialing, this is revolutionary.
Imagine a provider completes medical school and board certification. These credentials are verified once and added to a blockchain. When that provider applies to a hospital, instead of starting from scratch, the hospital simply accesses the blockchain to confirm the credentials are valid. No duplicate verification needed.
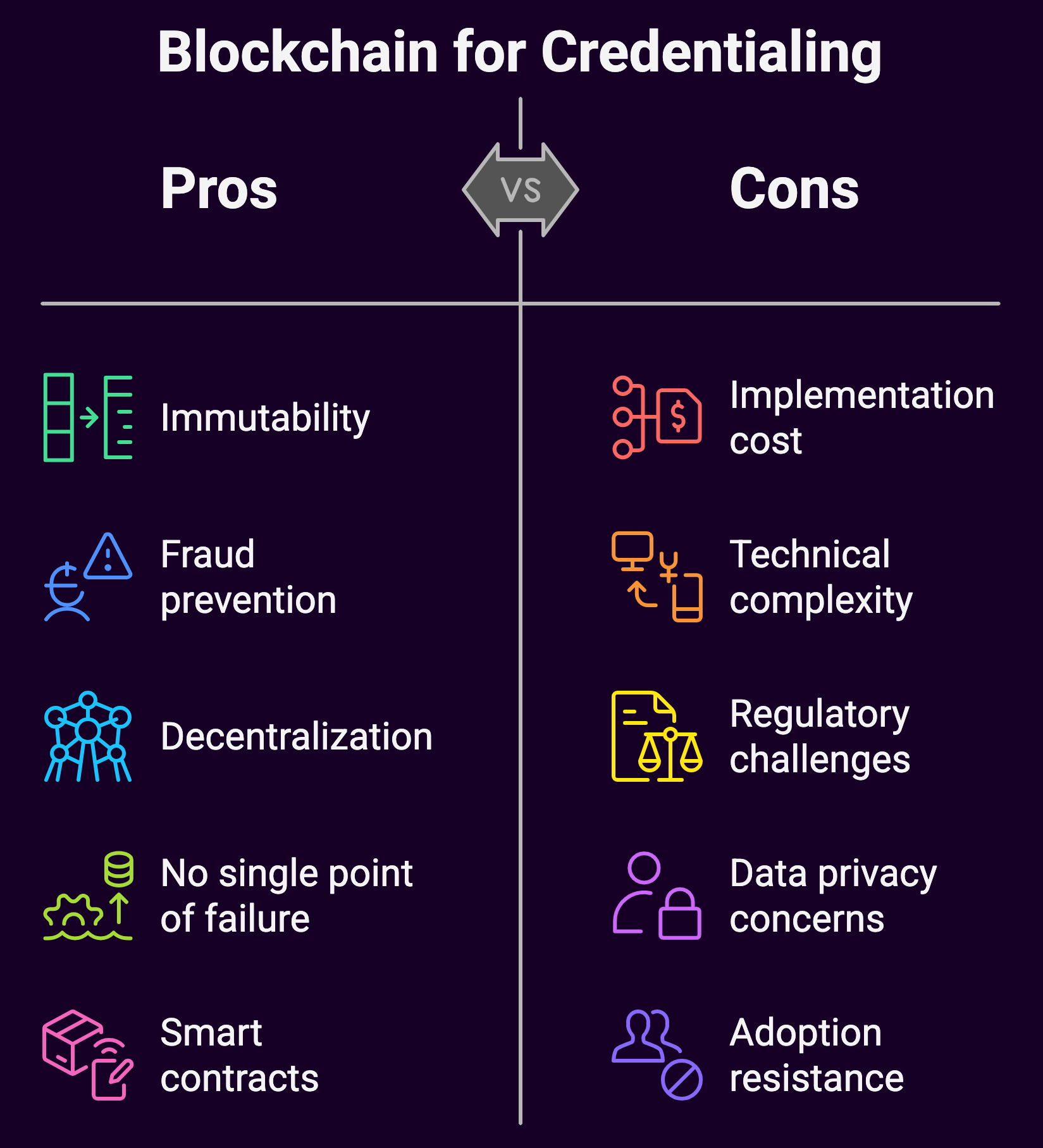
The benefits of blockchain credentialing include:
Immutability
Once credentials are verified and recorded on the blockchain, they can’t be altered without detection. This eliminates concerns about credential fraud and tampering.
Decentralization
No single entity controls the entire blockchain. This means no single point of failure and no single authority that can manipulate the data.
Smart Contracts
These are self-executing contracts with terms written directly into code. For credentialing, smart contracts could automatically trigger revalidation processes when licenses are about to expire.
Several healthcare systems are already piloting blockchain credentialing solutions.
AI: Making Credentialing Intelligent
If blockchain is the foundation of future credentialing, artificial intelligence is the architect designing a more efficient structure on top of it.
AI can transform credentialing in several ways:
Automated Primary Source Verification
AI algorithms can scan databases, websites, and digital documents to verify credentials without human intervention. What once took staff weeks can be accomplished in minutes.
Predictive Analytics
By analyzing patterns in credentialing data, AI can flag potential issues before they become problems. For example, it might identify providers who are likely to have licensure issues based on similar patterns from previous cases.
Natural Language Processing (NLP)
NLP can extract relevant information from unstructured data sources like recommendation letters, making these qualitative elements easier to incorporate into the credentialing process.
One healthcare network implemented an AI-powered credentialing system that reduced processing time by 80% and decreased errors by over 90%. The system automatically pulled data from primary sources, tracked changing requirements across different states, and alerted staff to discrepancies that needed human attention.
Digital Identities and Portable Credentials
Beyond blockchain and AI, the concept of a digital professional identity is gaining traction. This is essentially a secure, verified digital version of your professional self that can be shared with authorized parties.
The Federation of State Medical Boards has been exploring a digital “passport” system that would allow physicians to practice across state lines without going through full credentialing in each state. This is especially relevant in the age of telehealth, where providers may treat patients in multiple states.
Here’s how digital identities work:
- A provider establishes a verified digital identity containing their credentials
- This identity is cryptographically secured to prevent tampering
- The provider controls access, granting permission to specific organizations
- Updates to credentials occur in real-time and are automatically shared with authorized parties
Biometric Verification: Beyond Passwords
Increasingly, healthcare recognizes the importance of cybersecurity and biometric verification is becoming part of the credentialing ecosystem. Fingerprints, facial recognition, and even behavioral biometrics (how you type or move your mouse) can add layers of security to ensure that only the legitimate credential holder can access and share their information.
The Interoperability Challenge
The promise of these technologies hinges on interoperability. The ability of different systems to communicate with each other seamlessly. While blockchain provides a technical foundation for this, the healthcare industry will need to agree on standards.
Organizations like CAQH (Council for Affordable Quality Healthcare) and FHIR (Fast Healthcare Interoperability Resources) are already working on standardization efforts. The goal is to create a universal “language” that all credentialing systems can speak, regardless of the technology they use.
Regulatory Considerations

Innovation in credentialing doesn’t happen in a vacuum. Regulatory bodies will play a crucial role in determining how quickly these technologies can be adopted.
Some forward-thinking state medical boards are already amending regulations to accommodate blockchain verification and AI-powered credentialing. However, others remain cautious, citing concerns about data privacy and the reliability of automated systems.
The federal government is also getting involved. The Centers for Medicare & Medicaid Services (CMS) has expressed interest in streamlining credentialing to reduce administrative costs across the healthcare system. Their backing could accelerate adoption of these technologies.
What This Means for Healthcare Providers
If you’re a healthcare provider, these changes promise a future where:
- You verify your credentials once and control who accesses them
- Joining a new organization takes days instead of months
- License renewals happen automatically, with reminders before expiration
- Moving across state lines doesn’t mean starting the credentialing process from scratch
- Your verified credentials become a professional asset you own and manage
The Patient Impact
Patients rarely think about provider credentialing, but they feel its effects every day.
Streamlined credentialing means:
- Shorter wait times for appointments with new providers
- Increased access to care, especially in underserved areas
- Greater confidence in provider qualifications
- Lower healthcare costs as administrative overhead decreases
Implementation Timeline: When Will This Become Reality?
While some of these technologies are already being piloted, widespread adoption will likely follow this timeline:
Near-term (1-2 years)
- More healthcare systems adopting AI-powered primary source verification
- Limited blockchain pilots expanding to regional networks
- Digital identity solutions gaining regulatory approval in progressive states
Mid-term (3-5 years)
- Interoperable blockchain credentialing networks connecting multiple states
- AI becoming standard for credential monitoring and verification
- Biometric verification becoming commonplace for credential access
Long-term (5-10 years)
- Global blockchain networks for international credential verification
- Fully automated credentialing becoming the standard
- Legacy paper-based systems being completely phased out
Challenges to Overcome
Despite the promise, several challenges remain:
Data Privacy Concerns
Healthcare data is highly regulated. Any credentialing solution must comply with HIPAA and other privacy regulations.
Initial Cost
While these technologies will save money long-term, the initial implementation costs can be substantial.
Resistance to Change
Healthcare has traditionally been slow to adopt new technologies. Overcoming institutional inertia will require evidence of concrete benefits.
Technical Limitations
Blockchain, in particular, has scalability challenges that need to be addressed for industry-wide implementation.
Getting Started Now
If you’re a healthcare administrator interested in future-proofing your credentialing process, consider these steps:
- Audit your current credentialing workflow to identify bottlenecks
- Research vendors offering AI-powered credentialing solutions
- Join industry groups focused on credentialing innovation
- Participate in pilot programs for blockchain credentialing
- Update your policies to accommodate digital verification methods
Summary: A Credentialing Tech Revolution
![]() The credentialing revolution isn’t just about the tech. It’s about tearing down and rebuilding a system that’s been driving providers crazy for decades. Credentialing using blockchain and AI? They’re just tools. The real change is shifting power back to healthcare professionals.
The credentialing revolution isn’t just about the tech. It’s about tearing down and rebuilding a system that’s been driving providers crazy for decades. Credentialing using blockchain and AI? They’re just tools. The real change is shifting power back to healthcare professionals.
This shift cuts deeper than efficiency. It’s acknowledging that a doctor’s credentials belong to them, not buried in filing cabinets across a dozen different HR departments. It recognizes that verification should protect patients without punishing providers.
Tomorrow’s credentialing will be fast, secure, and actually make sense. It’ll clear administrative roadblocks so healthcare can focus on what matters, treating people.
Contact us to assist with your provider credentialing needs and/or challenges.