Negotiating the maze of state credentialing requirements can feel like trying to solve a Rubik’s cube blindfolded. Whether you’re a seasoned healthcare provider expanding your practice across state lines or a newly minted physician starting your career, understanding the nuances of state-specific credentialing requirements is crucial for your success.
 In the undermentioned content, we’ll break down everything you need to know about state-by-state credentialing requirements, helping you avoid common credentialing pitfalls and streamline your process.
In the undermentioned content, we’ll break down everything you need to know about state-by-state credentialing requirements, helping you avoid common credentialing pitfalls and streamline your process.
Understanding the Basics of State Credentialing
Before we jump into state-specific requirements, let’s gain clarity on the basics. State credentialing isn’t just about checking boxes or going through the motions. It’s about ensuring patient safety and maintaining healthcare quality standards across different jurisdictions. Each state has its own medical board, nursing board, and other regulatory bodies that oversee healthcare provider credentialing.
The Foundation of State Requirements
At its core, state credentialing typically includes verification of:
- Education and training
- Licensure
- Board certifications
- Work history
- Malpractice insurance
- Clinical privileges
- Professional references
- Background checks
However, here’s where it gets interesting: how states handle these requirements can vary significantly. What’s perfectly acceptable in California might not fly in Texas, and what works in New York could be insufficient in Florida.
Key Differences Between State Requirements
Timeline Variations
One of the biggest differences you’ll encounter is timing. Some states work at lightning speed (well, relatively speaking), while others seem to operate on geological time.
Here’s what you need to know:
Fast-track states (2-4 weeks):
- Arizona
- Nevada
- Utah
- Wisconsin
Standard timeline states (4-8 weeks):
- Florida
- Texas
- Ohio
- Michigan
Extended process states (8+ weeks):
- California
- New York
- Illinois
- New Jersey
Documentation Requirements
The paperwork game varies significantly by state.
Let’s break down some key differences, for example:
California
- Requires original transcripts sent directly from educational institutions
- Mandates LiveScan fingerprinting for background checks
- Needs detailed explanation of any gaps in work history longer than 30 days
Texas
- Accepts notarized copies of educational documents
- Requires state-specific background check forms
- Mandates completion of state jurisprudence exam
New York
- Demands certified translations for any non-English documents
- Requires detailed verification of all postgraduate training
- Needs specific forms for reference letters
Florida
- Accepts electronic verification of education in most cases
- Requires proof of CME completion
- Mandates specific background screening through the state system
Regional Breakdowns and Specific State Requirements
Northeast Region
The Northeast tends to have some of the strictest requirements.
Let’s look at some specifics, for example:
Massachusetts
- Requires completion of Patient Care Assessment Program
- Mandates specific opioid prescribing education
- Needs detailed hospital privilege verification
Connecticut
- Requires state-specific controlled substance registration
- Mandates specific background check through state police
- Needs verification of all state licenses ever held
Rhode Island
- Requires proof of malpractice insurance with specific coverage amounts
- Mandates completion of substance abuse training
- Needs detailed verification of work history for the past 10 years
Southeast Region
The Southeast often focuses heavily on controlled substance requirements and background checks, for example:
Georgia
- Requires specific DEA registration for each practice location
- Mandates completion of human trafficking awareness training
- Needs detailed explanation of any malpractice claims
North Carolina
- Requires completion of controlled substance prescribing course
- Mandates specific background check through state bureau
- Needs verification of hospital privileges for past 5 years
Midwest Region
Midwest states often have unique requirements related to rural healthcare, for example:
Illinois
- Requires specific collaborative agreement documentation
- Mandates completion of sexual harassment prevention training
- Needs detailed verification of all previous practice locations
Michigan
- Requires specific controlled substance licenses
- Mandates completion of human trafficking training
- Needs detailed verification of all previous state licenses
Western Region
Western states often lead the way in technological integration, for example:
Washington
- Accepts electronic verification through specific platforms
- Requires completion of suicide prevention training
- Mandates specific background check through state patrol
Oregon
- Requires pain management CME
- Mandates cultural competency training
- Needs verification of all previous practice settings
Special Considerations for Telemedicine Providers
The explosion of telemedicine has added another layer of complexity to state credentialing.
Here’s what you need to know:
Interstate Medical Licensure Compact (IMLC)
The IMLC has been a game-changer for telemedicine providers. Currently, 33 states participate, making it easier to practice across state lines.
Key points include:
- Expedited licensing process for qualified providers
- Single application for multiple state licenses
- Standardized verification process
- Regular updates to requirements and participating states
State-Specific Telemedicine Requirements
Even with the IMLC, states maintain specific requirements for telemedicine practice:
- Some states require in-person initial visits
- Different states have varying requirements for remote prescribing
- Technology and security requirements vary by state
- Documentation requirements can differ for virtual visits
Interstate Compacts and Multi-State Practice
Nursing Licensure Compact (NLC)
Similar to the IMLC, the NLC facilitates multi-state practice for nurses:
- Allows practice in multiple states with a single license
- Standardizes requirements across participating states
- Regular updates to participating states and requirements
- Specific requirements for compact license eligibility
Other Professional Compacts
Various healthcare professions have their own interstate compacts:
- Physical Therapy Compact
- Psychology Interjurisdictional Compact (PSYPACT)
- Advanced Practice Registered Nurse Compact
- Emergency Medical Services Compact
Common Challenges and Solutions
Challenge 1: Keeping Track of Multiple State Requirements
Solution: Implement a robust tracking system:
- Use credential management software
- Create state-specific checklists
- Set up automatic renewal reminders
- Maintain detailed documentation of requirements by state
Challenge 2: Managing Timeline Variations
Solution: Develop a strategic approach:
- Start applications early
- Prioritize slower states
- Maintain current documentation
- Use expedited processes when available
Challenge 3: Handling Different Verification Requirements
Solution: Create a comprehensive verification strategy:
- Maintain relationships with previous institutions
- Keep detailed records of all verifications
- Use CAQH ProView for standardized data
- At Medwave, we can create or update a CAQH Pro-View account for you
- Implement a system for tracking verification requests
Best Practices for Multi-State Credentialing
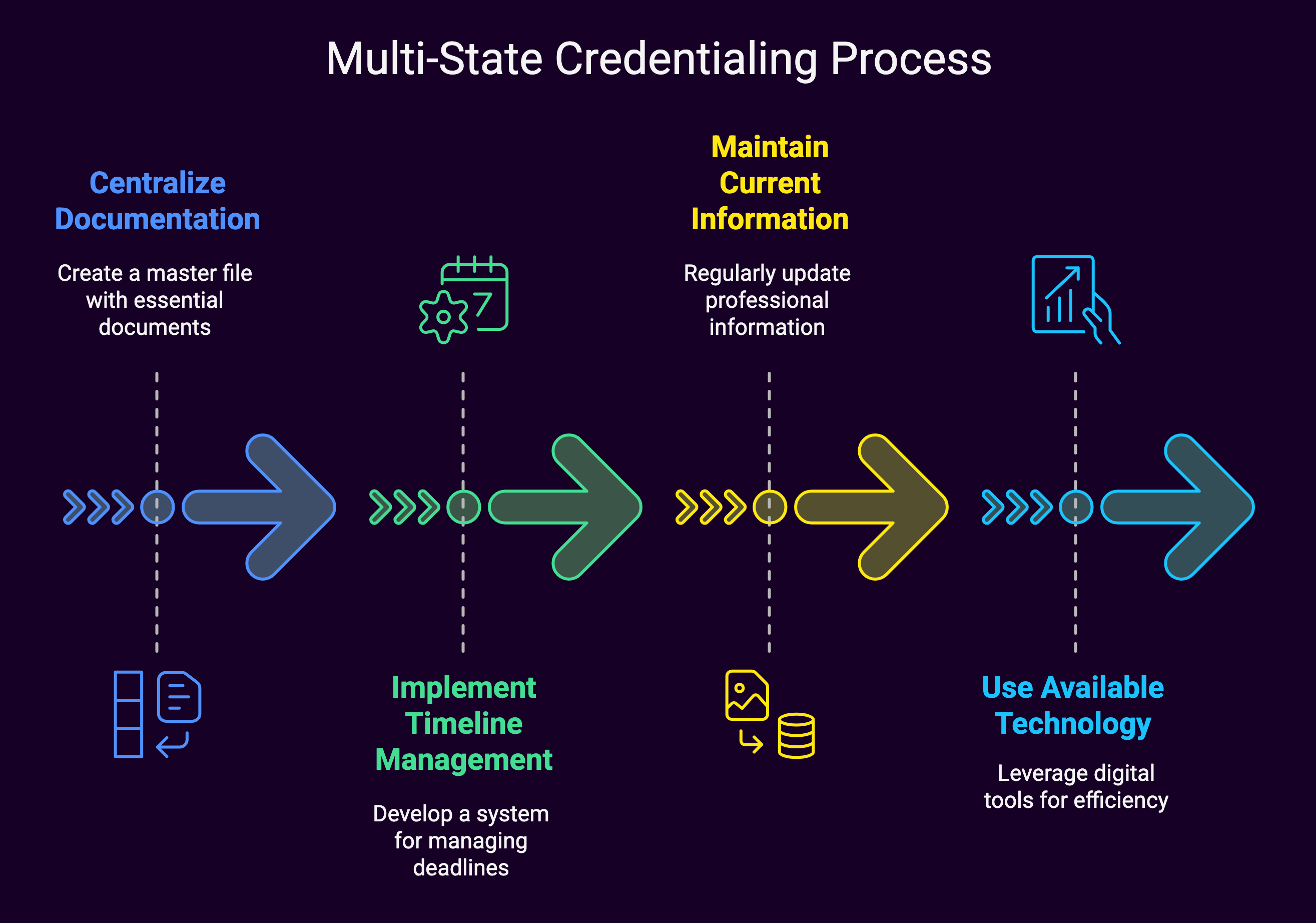
1. Centralize Your Documentation
Create a master file containing:
- Education certificates
- License information
- Board certifications
- Work history
- Reference contact information
- Malpractice insurance documentation
2. Implement a Timeline Management System
Develop a system that includes:
- Application deadlines
- Renewal dates
- Verification timeframes
- Follow-up schedules
- Processing time estimates
3. Maintain Current Information
Regular updates should include:
- Professional development activities
- CME completion
- Address changes
- Practice updates
- Insurance coverage changes
4. Use Available Technology
Leverage technology solutions:
- Credentials verification organizations (CVOs)
- Online application systems
- Digital document storage
- Automated renewal reminders
- Electronic verification platforms
Resources and Tools for Success
State Medical Board Websites
Each state maintains its own medical board website with current requirements:
- Application forms
- Fee schedules
- Processing timelines
- Specific state requirements
- Contact information
Professional Organizations
Many organizations provide credentialing support:
- American Medical Association (AMA)
- National Association Medical Staff Services (NAMSS)
- State medical societies
- Specialty-specific organizations
Credentialing Services
Consider using professional credentialing services:
- CVOs
- Credentials verification services
- Application processing services
- Document management services
Summary: State-by-State Provider Credentialing Requirements
Negotiating state-by-state credentialing requirements doesn’t have to be overwhelming. Understanding the variations between states, maintaining organized documentation, and utilizing available resources allows healthcare providers to create an efficient process for managing multiple state credentials. Requirements constantly evolve, so staying informed about changes and maintaining current documentation is crucial for success.
The key is to approach state credentialing strategically, using available tools and resources while maintaining detailed records and staying ahead of deadlines. Whether you’re managing credentials for a single state or planning to practice across multiple jurisdictions, a systematic approach will help ensure smooth sailing through the credentialing process.

