An Explanation of Benefits (EOB) plays a crucial role in helping patients understand the costs and coverage associated with their healthcare services.
 An EOB is a document that provides a detailed breakdown of a medical claim, outlining the services rendered, the amount billed, the insurance coverage, and the patient’s financial responsibility. Let’s delve deeper into the significance of EOBs and how they impact the medical billing process.
An EOB is a document that provides a detailed breakdown of a medical claim, outlining the services rendered, the amount billed, the insurance coverage, and the patient’s financial responsibility. Let’s delve deeper into the significance of EOBs and how they impact the medical billing process.
Medical billing involves the intricate process of submitting and processing claims for healthcare services provided to patients. EOBs serve as a vital communication tool between insurance companies, healthcare providers, and patients, helping everyone involved gain clarity regarding the financial aspects of medical treatment.
Medical Billing Overview
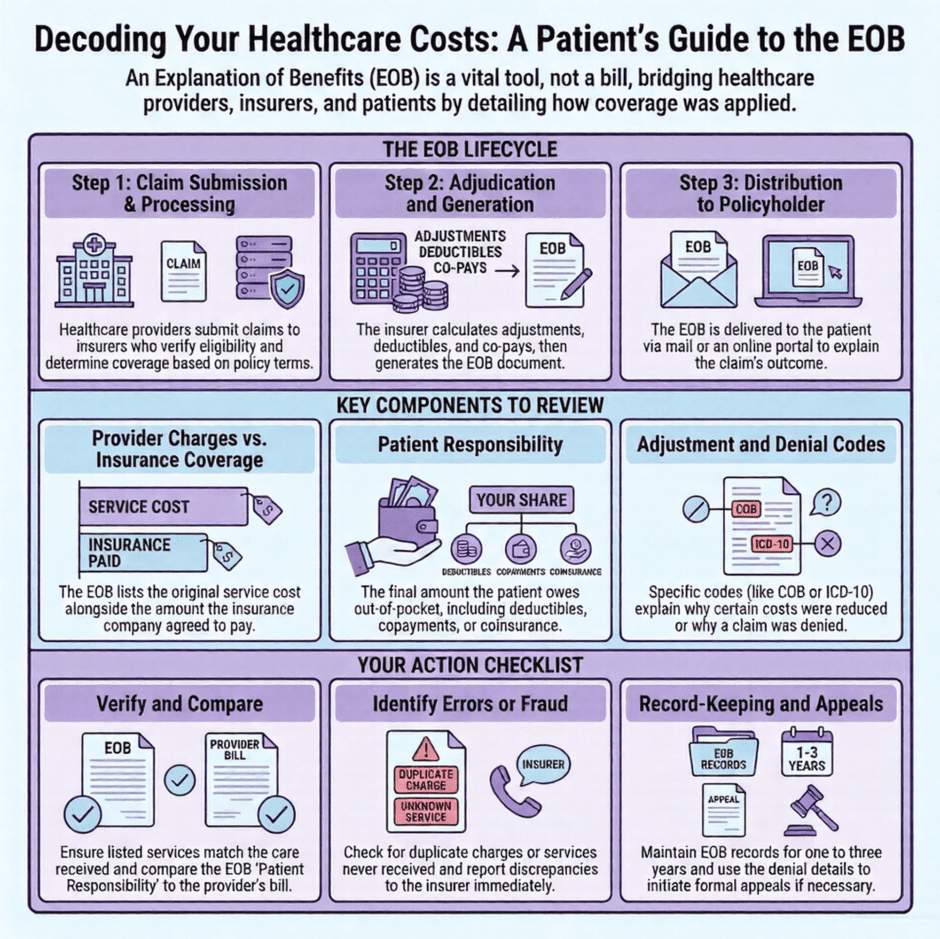
Before diving into the specifics of EOBs, it’s important to have knowledge of medical billing. The billing process encompasses various steps, including patient registration, insurance verification, claim submission, claim processing, and reimbursement. EOBs come into the picture during the claim processing phase.
What are Explanation of Benefits (EOBs)?
Explanation of Benefits, commonly referred to as EOBs or EOBS, is a term you’ll frequently encounter in medical billing. It’s also known as Explanation of Medical Benefits (OMBs). Simply put, EOBs are documents that outline the details of a claim adjudication process by insurance payers.
An EOB is a document sent by insurance companies to policyholders or patients who have received healthcare services. The primary purpose of an EOB is to explain how an insurance claim was processed and to inform the patient about the financial implications of the services received.
EOBs serve as a bridge of information, offering insights into the coverage provided by the insurance policy, any adjustments made to the billed amount, and the patient’s financial responsibility for the services rendered.
Key Components of an EOB
- Patient Information: EOBs typically start with the policyholder’s personal information, including their name, policy number, and contact details. Ensuring the accuracy of this information is crucial for effective communication and record-keeping.
- Claim Details: The EOB will outline the specific claim or service being addressed, including the date of service, the healthcare provider’s name, and a description of the service rendered. This section helps policyholders identify the context of the EOB and understand the services for which they are being billed.
- Provider Charges: Insurance companies include the healthcare provider’s charges in the EOB to give policyholders visibility into the cost of the services received. The EOB will detail the individual charges for each service, allowing policyholders to compare them with their healthcare provider’s pricing.
- Insurance Coverage: This section provides an overview of the insurance company’s coverage for the specific claim or service. It highlights the amount covered, the deductible (if applicable), and any coinsurance or copayment responsibilities.
- Patient Responsibility: EOBs also include a breakdown of the policyholder’s financial responsibility. This may include deductibles, copayments, or coinsurance amounts. Understanding this section helps policyholders anticipate and plan for their out-of-pocket expenses.
Decoding EOB Terminology
Explanation of Codes
EOBs often contain various codes and abbreviations that can be confusing for policyholders. To better understand the information presented, here are some common codes and their meanings:
- COB: Coordination of Benefits – This code indicates if the policyholder has multiple insurance plans and how they work together to cover the claim.
- EOB: Explanation of Benefits – Refers to the document itself.
- EOB Denial Codes: These codes provide reasons for claim denials or partial coverage.
- ICD-10 Codes: International Classification of Diseases, 10th Revision – These codes represent specific diagnoses or medical conditions.
Importance of EOB
Receiving and understanding EOBs is essential for patients as they provide valuable information about the financial aspects of their medical care. Here are a few key benefits of receiving EOBs:
- Transparency and Clarity: EOBs help patients understand the breakdown of charges, the amount covered by insurance, and the patient’s responsibility for payment. This transparency promotes informed decision-making and reduces any confusion or surprises related to medical bills.
- Tracking Healthcare Expenses: EOBs provide a comprehensive overview of the services rendered, including dates, descriptions, and costs. Patients can use these documents to track their healthcare expenses, ensuring accuracy and facilitating budgeting.
- Insurance Coverage Verification: EOBs allow patients to verify that the insurance company has correctly processed their claims and applied the appropriate coverage. In case of discrepancies, patients can take necessary steps to resolve issues and ensure accurate billing.
- Identifying Errors and Fraud: EOBs provide an opportunity for patients to review the billed services and detect any potential errors or instances of fraud. By carefully examining the EOB, patients can identify discrepancies, such as duplicate charges or services not received, and report them to the insurance company for investigation.
- Appealing Decisions: If a claim is denied or partially covered by insurance, the EOB provides details about the reasons for the decision. Patients can use this information to understand the grounds for denial and take appropriate steps, such as appealing the decision or discussing alternative options with their healthcare provider.
How EOBs are Generated
EOBs are generated as part of the medical claims processing workflow. When a healthcare provider submits a claim to an insurance company, the insurer processes the claim and generates an EOB. This document is then sent to the policyholder or the patient, usually by mail or electronically through an online portal.
The EOB generation process involves multiple steps, including verifying the patient’s eligibility, reviewing the services provided, determining the coverage and payment details, and calculating the patient’s financial responsibility. The insurance company’s claims processing system generates the EOB based on these factors and the terms outlined in the patient’s insurance policy.
Common Challenges
While EOBs provide valuable information, they can sometimes be complex and challenging to understand. Here are some common challenges associated with EOBs and tips for overcoming them:
- Complex Terminology: EOBs often contain medical and insurance terminology that may be unfamiliar to patients. To overcome this challenge, patients can seek assistance from their healthcare provider or insurance company to clarify any terms they don’t understand.
- Lack of Itemized Details: In some cases, EOBs may not provide detailed information about each service or procedure, making it difficult for patients to identify specific charges. Patients can request an itemized bill from their healthcare provider to gain a better understanding of the services rendered and their associated costs.
- Discrepancies and Errors: Mistakes can occur in the processing of EOBs, such as incorrect billing codes or coverage calculations. Patients should carefully review their EOBs and compare them to the services received. If any discrepancies or errors are found, patients can contact their healthcare provider or insurance company to request corrections.
- Limited Explanation: EOBs may not always provide a comprehensive explanation of the coverage decisions made by the insurance company. Patients can reach out to their insurance company’s customer service department to seek further clarification or to file an appeal if they believe coverage was incorrectly denied.
Maximizing EOB Benefits
To make the most of EOBs, patients can follow these strategies:
- Review EOBs Promptly: Patients should review their EOBs as soon as they receive them. By reviewing the document promptly, patients can address any discrepancies or issues in a timely manner. This includes ensuring that the services listed on the EOB match the services they received and verifying the accuracy of the coverage and financial responsibility information.
- Compare EOBs with Medical Bills: Patients should compare the information provided in the EOB with their medical bills. This helps ensure that the billed amounts, adjustments, and insurance payments align with the information stated on the EOB. Any discrepancies should be addressed with the healthcare provider or insurance company.
- Keep a Record of EOBs: It is important for patients to maintain a record of their EOBs for future reference. This includes both electronic and physical copies of the documents. Keeping a record allows patients to track their healthcare expenses, monitor coverage details, and address any potential issues that may arise later.
- Utilize Online Portals: Many insurance companies provide online portals where patients can access their EOBs electronically. Patients should take advantage of these portals as they offer convenient access to EOBs and enable easier record-keeping. Online portals may also provide additional resources and tools to help patients understand their EOBs and navigate the medical billing process.
- Seek Assistance if Needed: If patients find it challenging to understand their EOBs or have questions about the information presented, they should not hesitate to seek assistance. Contacting the insurance company’s customer service or reaching out to the healthcare provider’s billing department can help clarify any confusion and ensure that patients have a clear understanding of their financial responsibilities.
Role of EOBs in Insurance Claims
EOBs play a crucial role in the insurance claims process. They serve as a communication tool between insurance companies, healthcare providers, and patients. Here’s how EOBs support the insurance claims process:
- Claims Verification: EOBs provide detailed information about the processing of a claim, allowing patients to verify that the insurance company has correctly processed the claim according to the terms of their insurance policy. Patients can review the EOB to ensure that the services rendered are accurately documented and that the insurance coverage has been applied correctly.
- Explanation of Payment: EOBs provide an explanation of how the insurance company has processed the claim and how the payment has been determined. This includes information on the portion of the claim that is covered by insurance, any adjustments made, and the patient’s financial responsibility. The EOB helps patients understand the financial implications of the claim and what they are responsible for paying.
- Tracking Reimbursements: For healthcare providers, EOBs serve as a record of the reimbursement they will receive from the insurance company. By comparing the information on the EOB with their own records, healthcare providers can ensure that they are being reimbursed correctly for the services they have rendered.
- Claim Documentation: EOBs serve as documentation of the services provided and the payment received for both the patient and the healthcare provider. This documentation is important for record-keeping purposes and may be required for future reference, such as when filing taxes or in case of insurance audits.
EOBs and Patient Financial Responsibility
EOBs have a direct impact on the financial responsibility of patients. They provide detailed information about the costs that patients are responsible for paying out of pocket. Here’s how EOBs relate to patient financial responsibility:
- Understanding Financial Responsibility: EOBs help patients understand their financial responsibility for the healthcare services they received. The document clearly states the amount the patient needs to pay, including deductibles, copayments, and coinsurance. By reviewing the EOB, patients can gain clarity on their financial obligations and plan accordingly.
- Budgeting and Financial Planning: EOBs provide patients with important information for budgeting and financial planning. By knowing the amount they owe, patients can set aside funds to cover their medical expenses. This helps them avoid financial surprises and enables them to manage their healthcare costs effectively.
- Appealing Charges: In cases where patients believe that the amount indicated on the EOB is incorrect or unjustified, they have the right to appeal the charges. EOBs provide the necessary details and explanations for patients to initiate the appeals process. This allows patients to advocate for themselves and potentially reduce their financial responsibility.
- Negotiating Payment Plans: If patients are unable to pay their full financial responsibility as indicated on the EOB, they can contact the healthcare provider or billing department to discuss alternative payment arrangements. EOBs serve as a reference point for these discussions and negotiations, helping patients explore options such as payment plans or financial assistance programs.
- Tracking Healthcare Expenses: EOBs serve as a comprehensive record of healthcare expenses for patients. By retaining EOBs, patients can track their medical spending, monitor their out-of-pocket costs, and use the information for tax purposes or insurance coverage verification.
- Financial Accountability: EOBs promote financial accountability by ensuring that patients are aware of their obligations and responsibilities. By reviewing the EOBs and paying their portion promptly, patients contribute to a smooth and efficient medical billing process.
Summary: EOBs in Billing
 Explanation of Benefits (EOBs) serve as essential documents that provide patients with valuable insights into the costs and coverage associated with their healthcare services. By understanding the significance of EOBs, patients can navigate the complexities of medical billing, gain transparency into their financial responsibilities, and make informed decisions regarding their healthcare expenses.
Explanation of Benefits (EOBs) serve as essential documents that provide patients with valuable insights into the costs and coverage associated with their healthcare services. By understanding the significance of EOBs, patients can navigate the complexities of medical billing, gain transparency into their financial responsibilities, and make informed decisions regarding their healthcare expenses.
EOBs not only offer a breakdown of medical claims but also serve as a means to verify insurance coverage, identify errors or discrepancies, and track healthcare expenses. They empower patients to actively participate in the billing process, enabling them to budget, appeal charges if necessary, and negotiate payment arrangements when needed.
EOBs are not just important for healthcare providers; they are also valuable for patients. Patients can review EOBs to understand the details of their healthcare services, the amount charged, and the portion covered by insurance. It helps them track their medical expenses and ensures transparency in healthcare billing.
Moreover, if there are any discrepancies or errors in the EOB, patients can contact their insurance provider to address the issue promptly. By empowering patients with information, EOBs contribute to a more informed and engaged healthcare consumer, promoting trust and accountability in the medical billing process.
EOBs are valuable tools that promote transparency, accountability, and financial well-being for patients. Engaging with EOBs gives patients the ability to effectively manage their healthcare costs and ensure a smoother and more informed medical billing experience.
EOB FAQs
- Can I receive my EOBs electronically?
Yes, many insurance companies offer the option to receive EOBs electronically through online portals or secure email. Check with your insurance provider to see if this option is available to you. - What should I do if I find errors or discrepancies on my EOB?
If you identify errors or discrepancies on your EOB, contact your healthcare provider’s billing department or your insurance company’s customer service. They can assist you in resolving the issues and making any necessary corrections. - Can I appeal a denial of coverage based on the information provided in the EOB?
Yes, if your claim is denied or partially covered by insurance, the EOB will provide details about the decision. You can use this information to understand the grounds for denial and initiate the appeals process with your insurance company. - How long should I keep my EOBs?
It is advisable to keep your EOBs for a certain period, typically around one to three years. This timeframe allows you to maintain a record of your healthcare expenses and coverage information. However, it’s always a good idea to check with your insurance provider or financial advisor for specific recommendations regarding record retention. - What if I don’t understand the terminology or information in my EOB?
If you come across unfamiliar terminology or have difficulty understanding the information presented in your EOB, don’t hesitate to seek assistance. Reach out to your healthcare provider’s billing department or contact your insurance company’s customer service. They can provide clarification and help you better comprehend the details of your EOB. - Are EOBs the same as medical bills?
No, EOBs and medical bills are different documents. An EOB provides an explanation of how your insurance company processed a claim and what your financial responsibility is. On the other hand, a medical bill is a statement from the healthcare provider indicating the amount owed for the services rendered. Both documents work together to provide a comprehensive overview of your healthcare expenses. - Can I use my EOB as proof of payment?
No, an EOB is not considered proof of payment. It is a document that explains how your claim was processed and the amounts covered by insurance. If you need proof of payment, you should refer to receipts, bank statements, or any other documents that indicate you have made payments for the services received. - What should I do if I disagree with the information provided in my EOB?
If you disagree with the information stated in your EOB, such as the coverage decision or the financial responsibility assigned to you, it is important to follow the appropriate steps. Contact your insurance company to discuss your concerns, seek clarification, and if necessary, initiate an appeal to address any disputes or discrepancies.

