The Merit-Based Incentive Payment System (MIPS) represents a critical component of healthcare’s value-based payment system, directly impacting your practice’s Medicare reimbursements. Yet many healthcare providers find themselves leaving money on the table due to suboptimal MIPS strategies. Knowledge of how to optimize your performance across all four MIPS categories can mean the difference between payment penalties and substantial bonuses.
MIPS Essentials
MIPS affects nearly 800,000 eligible clinicians nationwide, making it one of the most widespread quality reporting programs in healthcare.
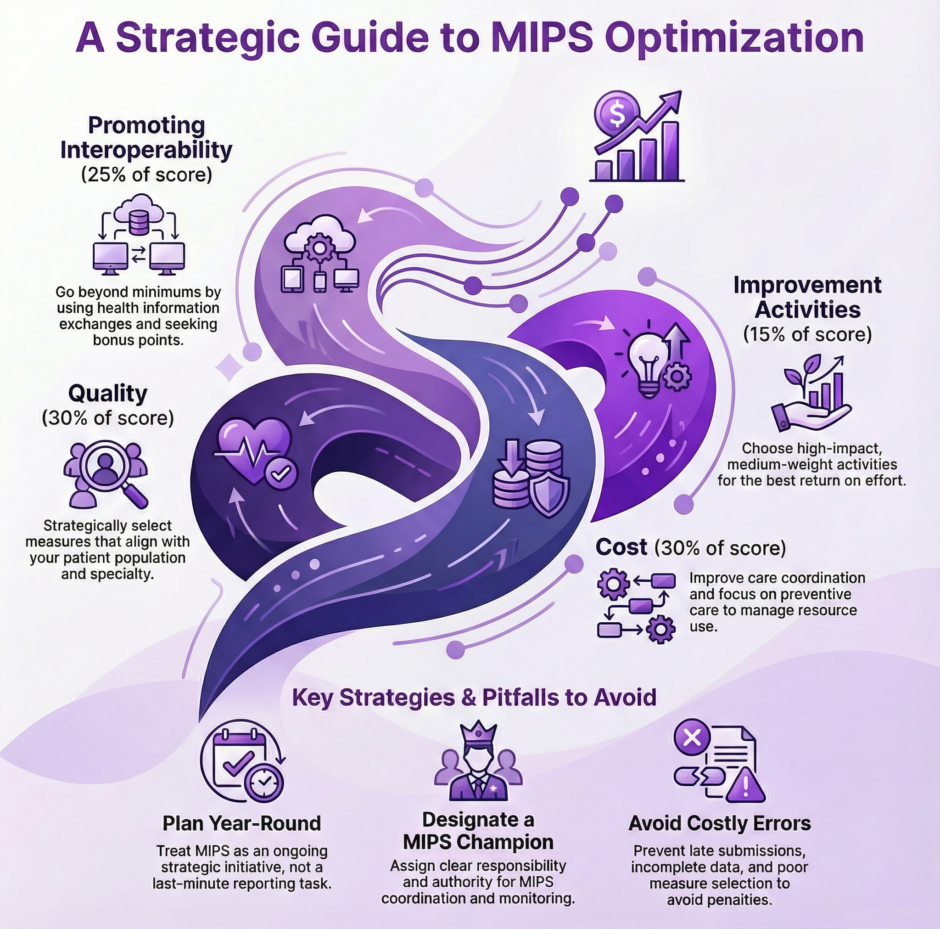
The program evaluates providers across four distinct performance categories, each carrying specific weight in your final score:
- Quality (30%): Clinical care outcomes and patient safety measures
- Cost (30%): Resource utilization and efficiency metrics
- Improvement Activities (15%): Practice improvement and care coordination efforts
- Promoting Interoperability (25%): Electronic health record usage and health information exchange
Your performance in these areas determines whether you receive positive, negative, or neutral payment adjustments to your Medicare Part B payments. With potential adjustments ranging from -9% to +9% in recent years, the financial implications are substantial for practices of all sizes.
Quality Category: Building Your Foundation
 The Quality category forms the cornerstone of MIPS performance, requiring providers to report on six quality measures. However, many practices approach this category reactively rather than strategically. To maximize your Quality score, focus on measures where your practice naturally excels while identifying opportunities for targeted improvement.
The Quality category forms the cornerstone of MIPS performance, requiring providers to report on six quality measures. However, many practices approach this category reactively rather than strategically. To maximize your Quality score, focus on measures where your practice naturally excels while identifying opportunities for targeted improvement.
Start by analyzing your patient population and common diagnoses. Select measures that align with your specialty and patient mix, ensuring you’ll have sufficient case volume to demonstrate meaningful performance. For instance, a cardiology practice should prioritize measures related to blood pressure control, lipid management, and medication adherence rather than generic measures that may not reflect their expertise.
Data collection timing plays a crucial role in quality performance. Rather than scrambling to gather information at year-end, implement systematic data collection processes throughout the reporting period. This approach allows you to identify performance gaps early and take corrective action before it’s too late to impact your scores.
Consider the benchmarking methodology when selecting measures. MIPS uses historical data to establish performance thresholds, meaning measures with wide performance variation among providers offer greater opportunities for high scores. Research which measures in your specialty have favorable benchmarking distributions and prioritize these in your measure selection strategy.
Cost Category: Managing What You Can Control
The Cost Category often feels frustrating to providers because it measures factors that seem outside their direct control. However, understanding how Cost scores are calculated reveals opportunities for meaningful improvement. MIPS evaluates cost performance through episode-based cost measures and total per capita costs, comparing your resource utilization to peer providers treating similar patients.
Focus on care coordination and care transitions, as these areas significantly impact cost performance. Patients who experience smooth transitions between care settings and receive well-coordinated care typically require fewer emergency interventions and redundant services. Establish clear communication protocols with referring providers, ensure timely follow-up appointments, and implement medication reconciliation processes to reduce costly adverse events.
Preventive care represents another avenue for cost optimization. While preventive services require upfront investment, they often reduce downstream costs associated with disease progression and acute care episodes. Document preventive care activities thoroughly and ensure appropriate coding to demonstrate your commitment to population health management.
Review your referral patterns and consider whether you’re directing patients to high-value specialists and facilities. While you cannot control the costs incurred by other providers, thoughtful referral decisions can influence the overall cost of care for your attributed patients.
Improvement Activities: Demonstrating Continuous Enhancement
 The Improvement Activities category offers perhaps the most flexibility in MIPS, allowing providers to choose from over 100 different activities across various domains.
The Improvement Activities category offers perhaps the most flexibility in MIPS, allowing providers to choose from over 100 different activities across various domains.
This flexibility can be overwhelming, but it also presents opportunities to align MIPS reporting with genuine practice improvement initiatives.
Medium-weight activities (worth 20 points each) typically offer the best return on investment, requiring less intensive implementation than high-weight activities while still providing substantial score contributions.
Consider these high-impact medium-weight options:
- Implementing medication reconciliation processes
- Conducting regular care team meetings
- Participating in quality improvement collaboratives
- Using patient engagement tools and resources
- Implementing fall risk assessment protocols
High-weight activities (worth 40 points each) require more substantial commitment but can significantly boost your Improvement Activities score with fewer individual activities. These often involve participation in registries, advanced care models, or population health initiatives that may align with your practice’s strategic goals.
Document your Improvement Activities implementation thoroughly throughout the year. MIPS audits focus heavily on this category, and detailed documentation of your activities, implementation timelines, and outcomes will be essential if your practice is selected for audit.
Promoting Interoperability: Leveraging Technology Effectively
The Promoting Interoperability category, formerly known as Meaningful Use, evaluates how effectively your practice uses certified electronic health record technology to improve patient care and care coordination. Many providers view this category as a checkbox exercise, but strategic approaches can yield both high MIPS scores and genuine practice benefits.
The base score component requires meeting specific thresholds for various EHR functions. However, simply meeting minimum thresholds leaves points on the table. Analyze your current interoperability performance levels and identify opportunities to exceed thresholds without creating excessive administrative burden.
Health Information Exchange represents a significant scoring opportunity that many practices underutilize. Establish connections with regional health information exchanges, hospitals, and specialist practices to facilitate seamless information sharing. These connections not only improve your MIPS scores but also enhance care coordination and reduce redundant testing.
The bonus point opportunities within Promoting Interoperability can significantly impact your overall MIPS score. Public health and clinical data registry reporting, while requiring initial setup effort, provide ongoing bonus points throughout the reporting period. Evaluate which bonus activities align with your practice’s capabilities and patient population.
Strategic Planning and Resource Allocation
 Maximizing MIPS performance requires treating it as an ongoing strategic initiative rather than an annual reporting requirement. Develop a year-round MIPS strategy that integrates performance improvement activities into your practice’s regular operations.
Maximizing MIPS performance requires treating it as an ongoing strategic initiative rather than an annual reporting requirement. Develop a year-round MIPS strategy that integrates performance improvement activities into your practice’s regular operations.
Assign clear responsibilities for MIPS coordination within your practice. Designate a MIPS champion who understands the program requirements and can monitor performance throughout the year. This individual should have sufficient authority to implement necessary changes and coordinate cross-functional improvement efforts.
Invest in staff training and education around MIPS requirements and best practices. Your clinical and administrative staff are crucial to MIPS performance, and their understanding of program requirements directly impacts your ability to capture and document qualifying activities.
Consider leveraging technology solutions to streamline MIPS reporting and performance monitoring. Many EHR vendors offer MIPS-specific reporting modules, and third-party solutions can provide real-time performance dashboards and automated data collection capabilities.
Common Pitfalls and How to Avoid Them
Many practices underperform in MIPS due to preventable mistakes and oversights. Late submission represents one of the most costly errors, as it results in automatic negative payment adjustments regardless of performance quality. Establish submission deadlines well in advance of CMS deadlines to allow time for data validation and error correction.
Incomplete data submission frequently reduces MIPS scores unnecessarily. Review your data completeness rates regularly throughout the reporting period and implement processes to ensure thorough documentation of qualifying activities and patient encounters.
Measure selection errors can significantly impact your Quality category performance. Avoid selecting measures with low case volumes or unfavorable benchmarking unless they represent areas of genuine clinical focus for your practice.
The MIPS of Tomorrow
 MIPS continues to undergo refinements and updates that may impact your optimization strategies. Stay informed about program changes through CMS communications and professional associations.
MIPS continues to undergo refinements and updates that may impact your optimization strategies. Stay informed about program changes through CMS communications and professional associations.
Consider how broader healthcare trends, such as value-based care adoption and health equity initiatives, may influence future MIPS requirements.
The program’s increasing emphasis on outcome measures and patient-reported outcomes suggests that practices should begin implementing systematic approaches to outcome tracking and patient engagement. These investments will likely provide both immediate MIPS benefits and long-term competitive advantages.
Summary: Maximize Your MIPS Performance
![]() Maximizing MIPS performance requires a strategic, year-round approach that goes beyond simple compliance. Know the nuances of each performance category and install targeted improvement initiatives. This will allow practices to transform MIPS from a reporting burden into a catalyst for genuine quality improvement and financial benefit.
Maximizing MIPS performance requires a strategic, year-round approach that goes beyond simple compliance. Know the nuances of each performance category and install targeted improvement initiatives. This will allow practices to transform MIPS from a reporting burden into a catalyst for genuine quality improvement and financial benefit.
The practices that thrive under MIPS are those that view the program as an opportunity to systematically improve care delivery while optimizing reimbursement. Through careful planning, strategic resource allocation, and consistent execution, your practice can achieve top-tier MIPS performance while advancing your broader quality and operational goals.
MIPS optimization is not a one-time effort, but an ongoing process of refinement and improvement. Start with a thorough assessment of your current performance, develop a strategic improvement plan, and implement systematic processes to monitor and enhance your performance throughout the year. The investment in MIPS optimization will pay dividends not only in improved Medicare reimbursements but also in enhanced patient care and practice efficiency.

