In healthcare, we often hear about breakthroughs in patient care, new treatments, and cutting-edge diagnostics. Yet behind the scenes, there’s another revolution quietly reshaping how healthcare organizations operate, especially when it comes to their financial health. This revolution is powered by FHIR Interoperability.
 At Medwave, we see the direct impact that delays, errors, and information silos have on a practice’s financial well-being. That’s why the principles behind FHIR are so important. It’s not just an IT buzzword; it’s a game-changer for revenue cycle management (RCM).What is FHIR, and how does it secretly supercharge your RCM? Let’s break it down.
At Medwave, we see the direct impact that delays, errors, and information silos have on a practice’s financial well-being. That’s why the principles behind FHIR are so important. It’s not just an IT buzzword; it’s a game-changer for revenue cycle management (RCM).What is FHIR, and how does it secretly supercharge your RCM? Let’s break it down.
What is FHIR; Why Does It Matter So Much?
First, let’s clear up the acronym. FHIR stands for Fast Healthcare Interoperability Resources. Don’t let the technical name intimidate you. In simpler terms, FHIR is like a universal translator and a super-efficient postal service for healthcare data.
Imagine every piece of information about a patient (including their doctor’s notes, lab results, prescriptions, insurance details, and billing codes) is written in a different language and stored in separate, locked cabinets across various hospitals, clinics, and labs. Sharing this vital information quickly and accurately becomes a nightmare. Mistakes happen, delays mount, and the patient’s care (and the clinic’s finances) suffer.
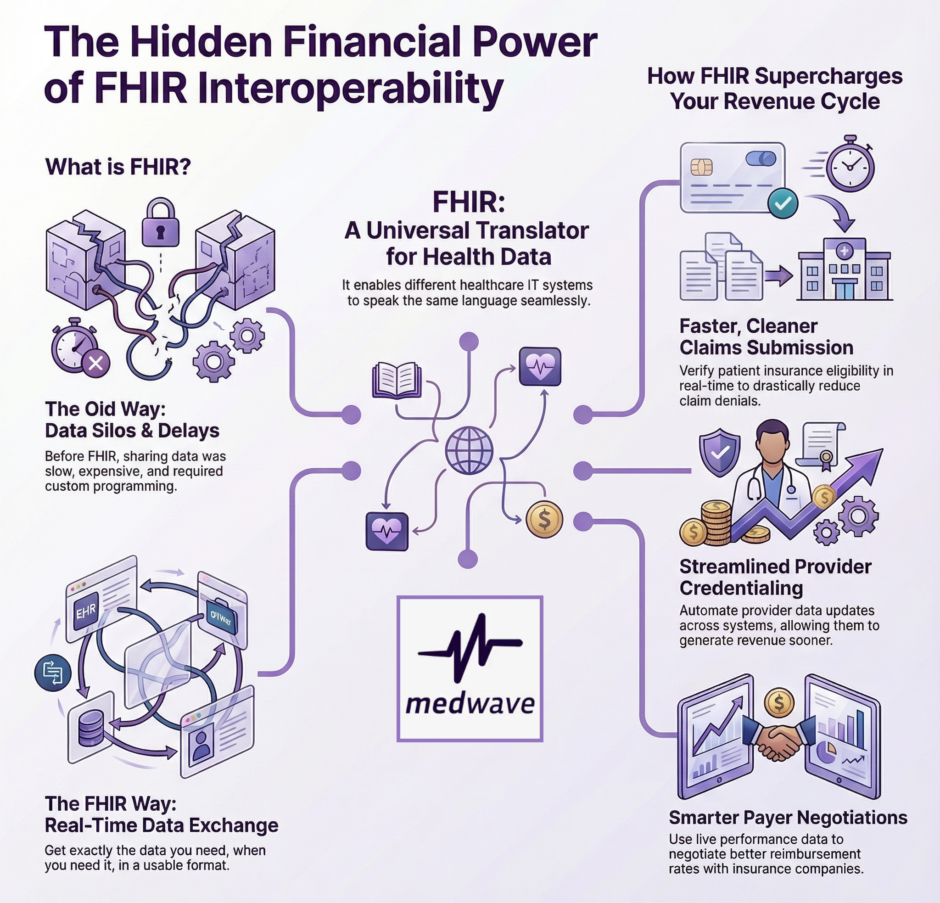
Before FHIR, healthcare data exchange was a bit like trying to connect a DVD player to a modern smart TV without the right cables. You had older, sometimes clunky, methods of sharing data (like HL7v2, for the tech-savvy among us). While these methods worked to some degree, they often required a lot of custom programming, extra effort, and constant tweaking to get different systems to “talk” to each other. It was slow, expensive, and prone to glitches.
FHIR steps in as the modern solution. It’s built on widely accepted web standards, similar to how many popular internet applications share data today. This means it’s designed to be lightweight, easy to implement, and flexible. It allows different healthcare IT systems, from Electronic Health Records (EHRs) to lab systems, pharmacy systems, and yes, even billing and RCM platforms, to speak the same language, using a common set of “resources.”
These “resources” are standardized building blocks of healthcare data, like patient demographics, appointments, medications, and insurance claims. By defining these resources in a consistent way, FHIR makes it incredibly simple for systems to exchange specific pieces of information without needing to swap entire patient records. It’s about getting exactly the data you need, when you need it, in a format everyone can use.
The Direct Line from FHIR to Your Revenue Cycle
 How does this technical standard directly improve your RCM? The answer lies in real-time data exchange and the elimination of friction.
How does this technical standard directly improve your RCM? The answer lies in real-time data exchange and the elimination of friction.
Think about the journey a patient’s bill takes, from their initial visit to the final payment. It involves many steps, many hands, and many opportunities for information to get misplaced or miscommunicated. FHIR acts as a lubricant, making this entire process smoother and faster.
By standardizing how billing information is formatted and shared, from insurance eligibility checks to claims submission to payment posting, FHIR ensures that each system along the chain can instantly understand and process the data it receives. This reduces manual data entry, minimizes errors, and can cut days or even weeks off the revenue cycle.
1. Faster, Cleaner Claims Submission
One of the biggest headaches in RCM is denied claims. A claim denial means delays, extra work, and a hit to your bottom line. Often, denials happen because of missing information, incorrect patient demographics, or issues with insurance eligibility.
With FHIR, your billing system can pull up-to-the-minute patient and insurance data directly from the EHR or payer portals.
Imagine this scenario:
- A patient checks in for an appointment.
- Your front office staff logs their information.
- In the background, FHIR-enabled systems verify the patient’s insurance eligibility and benefits in real-time, directly with the payer. This means you know exactly what services are covered before the patient even sees the doctor.
- Any discrepancies are flagged immediately, allowing for corrections on the spot, not weeks later after a denial.
This real-time validation drastically reduces the number of “dirty” claims, those with errors or missing data. Cleaner claims mean fewer denials, faster processing, and quicker payments. It cuts down on the back-and-forth between your billing team and the payer, freeing up your staff to focus on more critical tasks.
2. Supercharging Credentialing Processes
 Credentialing is the detailed process of verifying a healthcare provider’s qualifications, licenses, and background to ensure they meet the standards for practicing medicine and for being reimbursed by insurance companies. It’s a foundational service Medwave offers, and it’s notoriously time-consuming and document-heavy.
Credentialing is the detailed process of verifying a healthcare provider’s qualifications, licenses, and background to ensure they meet the standards for practicing medicine and for being reimbursed by insurance companies. It’s a foundational service Medwave offers, and it’s notoriously time-consuming and document-heavy.
Historically, credentialing involves mountains of paperwork, faxes, emails, and manual data entry across different systems (like CAQH ProView, payer portals, and your internal practice management software). Each piece of information (a medical license, a board certification, a malpractice insurance policy) has to be collected, verified, and often re-entered multiple times.
FHIR can significantly streamline this. Imagine a future where:
- Provider data (licenses, certifications, education) is maintained in a central, FHIR-enabled provider directory.
- As a provider’s information is updated in one system (e.g., a new license renewal), FHIR allows that update to automatically populate across all linked systems.
- Payer contracting teams can instantly access verified provider data, accelerating the onboarding process for new insurance networks.
This real-time synchronization drastically cuts down on the manual work, reduces human error, and speeds up the entire credentialing cycle. Getting providers credentialed faster means they can start seeing patients and generating revenue sooner. It transforms a months-long administrative burden into a more efficient, less frustrating experience.
3. Enhancing Payer Contracting and Rate Negotiation
Payer contracting is where Medwave helps practices get fair rates for their services. This involves negotiating with insurance companies, reviewing contract terms, and ensuring that providers are adequately reimbursed. This process requires accurate data about services provided, claims paid, and current reimbursement rates.
Without real-time data, practices often rely on retrospective analysis, looking back at claims from months or even a year ago to gauge performance. This makes it challenging to negotiate effectively for the future.
FHIR enables a more proactive approach:
- Real-time Performance Metrics: With FHIR, your RCM system can pull live data on current reimbursement rates, denial patterns for specific codes, and the actual cost of care for different procedures. This gives your contracting team unparalleled insights.
- Stronger Negotiation Position: Instead of guessing, you can walk into negotiations with payers armed with precise, up-to-the-minute data on how specific contract terms would impact your practice’s finances. This shifts the negotiation from guesswork to data-driven strategy.
- Faster Contract Implementation: Once new contract terms are agreed upon, FHIR can facilitate the rapid update of your billing system’s fee schedules and rules, ensuring that claims are processed correctly from day one under the new agreement.
This level of data currency allows practices to be more agile in their financial strategies, secure better contract terms, and minimize revenue leakage due to outdated or misapplied rates.
Beyond the Basics: Deeper RCM Advantages
The benefits of FHIR go even further than just claims, credentialing, and contracting.
They touch almost every aspect of financial operations:
- Accurate Patient Estimates
With instant access to payer information and historical claims data, your front office can provide patients with much more accurate estimates of their out-of-pocket costs *before* service. This increases patient satisfaction and improves the likelihood of collecting payments upfront, reducing bad debt. - Reduced Prior Authorization Delays
Prior authorizations are a common source of delays and denials. FHIR can link systems to automate the submission and tracking of prior authorization requests, often populating necessary clinical information directly from the EHR. This speeds up approval times and reduces administrative burden. - Better Denial Management
When a denial *does* occur, FHIR can help by providing instant access to all the related patient, clinical, and administrative data needed for appeals. This makes the denial management process faster and more efficient, increasing the chances of recovering lost revenue. - Enhanced Reporting and Analytics
With data flowing freely and consistently between systems, generating meaningful reports and performing predictive analytics becomes much simpler and more accurate. This allows RCM leaders to spot trends, identify areas for improvement, and make data-driven decisions that strengthen the practice’s financial health.
The Path Forward with FHIR: A Collaborative Effort
 Implementing FHIR interoperability isn’t a magic button, but it’s a direction that the entire healthcare industry is moving towards, driven by both technological advancements and regulatory mandates. The government’s push for greater interoperability (through initiatives like the 21st Century Cures Act) underscores the importance of standards like FHIR.
Implementing FHIR interoperability isn’t a magic button, but it’s a direction that the entire healthcare industry is moving towards, driven by both technological advancements and regulatory mandates. The government’s push for greater interoperability (through initiatives like the 21st Century Cures Act) underscores the importance of standards like FHIR.
For practices, clinics, and healthcare organizations, embracing FHIR means looking at their IT infrastructure not as isolated silos, but as interconnected parts of a larger, data-sharing ecosystem. It requires working with vendors who prioritize interoperability and asking tough questions about how their systems exchange data.
At Medwave, we believe that real-time data exchange is the cornerstone of efficient and profitable revenue cycle management.
Leveraging FHIR allows practices to:
- Streamline billing workflows
- Accelerate provider credentialing
- Optimize payer contracting
- Improve the overall financial experience for both patients and providers
It’s about creating a smarter, more responsive, and financially stronger healthcare system for everyone involved. The ability to exchange information seamlessly and in real-time will no longer be a luxury, it will be a necessity for any practice aiming to thrive.

