The healthcare industry has long struggled with the complex, time-consuming process of medical credentialing. Traditionally a paper-heavy, manual endeavor that could take months to complete, medical credentialing is undergoing a revolutionary transformation through artificial intelligence (AI) and machine learning technologies. This digital revolution is reshaping how healthcare organizations verify provider qualifications, maintain compliance, and ensure patient safety.
Medical Credentialing in the AI-Era
Medical credentialing is the systematic process of verifying healthcare providers’ qualifications, including their education, training, licensure, certifications, and professional experience. This critical process ensures that only qualified medical professionals are authorized to provide patient care within healthcare organizations.

The stakes are incredibly high. Inadequate credentialing can lead to compromised patient safety, regulatory violations, and significant legal liability.
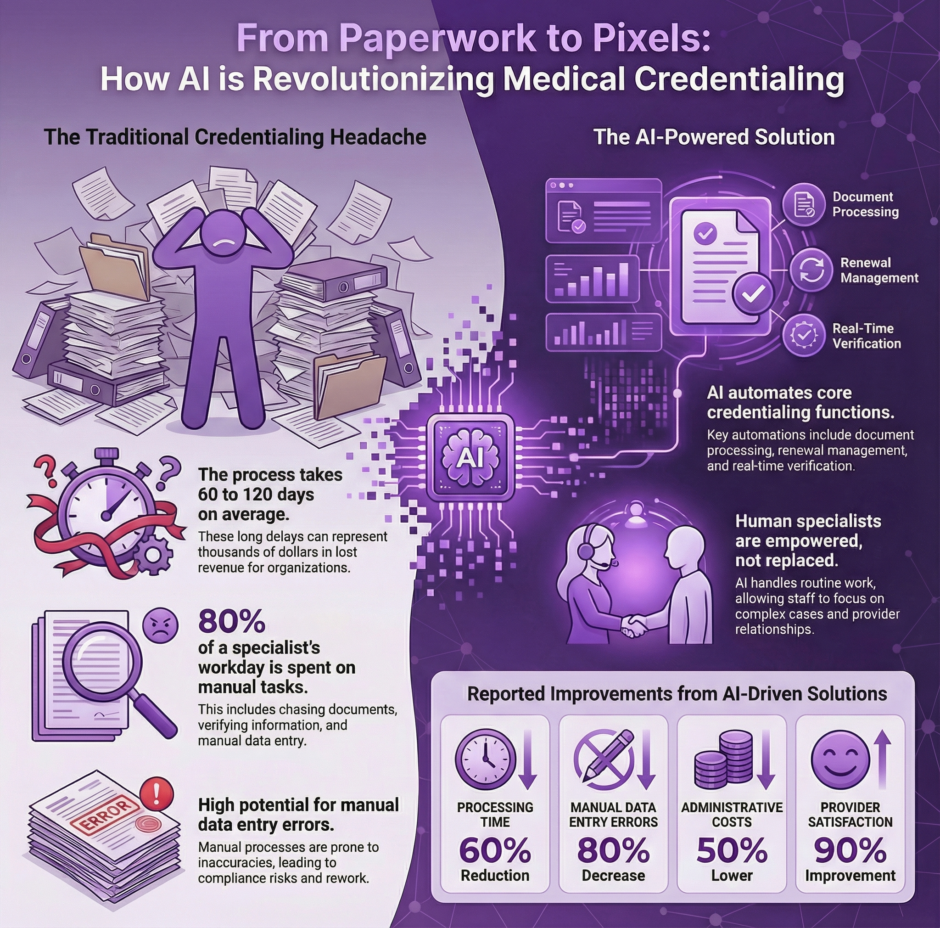
The traditional credentialing process has been notoriously cumbersome, often taking 90 to 180 days to complete. Healthcare administrators have historically wrestled with mountains of paperwork, endless phone calls to verification sources, and frustratingly slow processing times. However, AI technologies are fundamentally changing this landscape by automating routine tasks, accelerating verification processes, and improving accuracy across all credentialing activities.
Key Applications of AI in Medical Credentialing
Automated Document Processing and Verification
AI-powered systems excel at processing and analyzing vast amounts of documentation required for medical credentialing. Machine learning algorithms can automatically extract relevant information from certificates, diplomas, transcripts, and other credentialing documents, significantly reducing the manual data entry that has traditionally consumed countless administrative hours.
Optical Character Recognition (OCR) technology enhanced with AI capabilities can accurately read and interpret various document formats, even when dealing with handwritten materials or documents of varying quality. This automation extends beyond simple data extraction to include intelligent document classification, ensuring that each piece of documentation is properly categorized and routed through appropriate verification channels.
Real-Time Primary Source Verification
One of the most significant advancements in AI-driven credentialing involves automated primary source verification. AI systems can directly interface with licensing boards, educational institutions, and certification bodies to verify credentials in real-time, eliminating the need for manual phone calls and written requests that traditionally slowed the credentialing process.
These intelligent systems can continuously monitor multiple databases simultaneously, cross-referencing provider information across various sources to ensure accuracy and completeness. When discrepancies are detected, AI algorithms can flag potential issues for human review, allowing credentialing staff to focus their attention on cases requiring professional judgment.
Predictive Analytics for Risk Assessment
AI technologies enable healthcare organizations to implement sophisticated risk assessment protocols during the credentialing process. Machine learning algorithms can analyze patterns in provider data, identifying potential red flags that might indicate increased liability risks or compliance concerns. These systems can evaluate factors such as malpractice history, disciplinary actions, and practice patterns to generate risk scores that help organizations make informed credentialing decisions.
Predictive analytics also help organizations anticipate credentialing renewal needs, automatically generating alerts when provider credentials are approaching expiration dates. This proactive approach prevents lapses in credentialing that could disrupt patient care or create compliance issues.
Intelligent Workflow Management
AI-powered workflow management systems optimize the entire credentialing process by intelligently routing applications through various stages of review. These systems can automatically assign priority levels based on urgency, complexity, and organizational needs, ensuring that critical credentialing requests receive appropriate attention.
Machine learning algorithms continuously analyze workflow patterns to identify bottlenecks and inefficiencies in the credentialing process. Learning from historical data, these systems can recommend process improvements and automatically adjust workflows to maximize efficiency while maintaining quality standards.
Benefits of AI Implementation in Medical Credentialing
Dramatic Reduction in Processing Time
The most immediately apparent benefit of AI implementation is the substantial reduction in credentialing processing time. Organizations implementing AI-driven credentialing solutions report processing time reductions of 50-70%, with some routine credentialing activities completing in days rather than months.
This acceleration occurs through multiple mechanisms. Automated document processing eliminates manual data entry delays, while real-time verification capabilities remove the waiting periods associated with traditional verification methods. Intelligent routing ensures that applications move efficiently through the credentialing workflow without unnecessary delays.
Enhanced Accuracy and Reduced Errors
AI systems demonstrate remarkable accuracy in data processing and verification activities, significantly reducing the human errors that have historically plagued manual credentialing processes. Machine learning algorithms excel at pattern recognition and can identify inconsistencies or anomalies that might escape human attention during manual review.
The standardization inherent in AI processing also eliminates the variability that can occur when different staff members handle credentialing tasks using slightly different approaches or interpretations. This consistency improves overall credentialing quality and reduces the risk of compliance issues.
Cost Efficiency and Resource Optimization
Healthcare organizations implementing AI credentialing solutions realize substantial cost savings through improved efficiency and reduced manual labor requirements. Staff previously dedicated to routine credentialing tasks can be reassigned to more complex responsibilities that require human expertise and judgment.
The reduction in processing time also translates to faster provider onboarding, enabling healthcare organizations to address staffing needs more rapidly and potentially increasing revenue through quicker deployment of qualified providers.
Improved Compliance and Audit Readiness
AI systems maintain detailed digital records of all credentialing activities, creating audit trails that facilitate regulatory compliance and accreditation processes. These systems can automatically generate reports required for various compliance purposes, reducing the administrative burden associated with regulatory requirements.
The enhanced accuracy and standardization provided by AI processing also improve organizations’ readiness for accreditation surveys and regulatory audits, as credentialing documentation is more likely to be complete, accurate, and properly organized.
Current AI Technologies in Medical Credentialing
Natural Language Processing (NLP)
Natural Language Processing enables AI systems to understand and interpret unstructured text within credentialing documents. This technology allows systems to extract meaningful information from narrative descriptions, recommendation letters, and other textual materials that would be difficult to process using traditional automated methods.
NLP capabilities are particularly valuable when dealing with international credentials or documents that may not follow standardized formats. The technology can interpret context and meaning, enabling more sophisticated analysis of credentialing materials.
Machine Learning Algorithms
Machine learning forms the foundation of most AI credentialing applications, enabling systems to learn from historical data and improve their performance over time. Supervised learning algorithms can be trained to recognize patterns in successful credentialing applications, while unsupervised learning can identify anomalies or unusual patterns that may require additional scrutiny.
Reinforcement learning techniques allow AI systems to optimize their decision-making processes based on feedback from credentialing outcomes, continuously improving their effectiveness in supporting credentialing decisions.
Robotic Process Automation (RPA)
Robotic Process Automation handles repetitive, rule-based tasks within the credentialing workflow. RPA bots can automatically submit verification requests, follow up on pending items, and update credentialing databases without human intervention.
These automated processes operate continuously, providing 24/7 capability for routine credentialing tasks and ensuring that time-sensitive activities receive immediate attention regardless of business hours.
Challenges and Considerations
Data Privacy and Security Concerns
The implementation of AI in medical credentialing raises important considerations regarding data privacy and security. Healthcare organizations must ensure that AI systems comply with HIPAA requirements and other applicable privacy regulations when processing sensitive provider information.
Robust cybersecurity measures are essential to protect credentialing data from unauthorized access or breaches. Organizations must implement appropriate encryption, access controls, and monitoring systems to maintain the confidentiality and integrity of credentialing information.
Integration Complexities
Integrating AI credentialing solutions with existing healthcare information systems can present technical challenges. Organizations must carefully plan implementation strategies to ensure seamless data flow between AI systems and legacy credentialing databases, HR systems, and other relevant applications.
The complexity of healthcare IT environments often requires custom integration solutions, which can increase implementation costs and timelines. Organizations must balance the benefits of AI implementation against the resources required for successful integration.
Change Management and Staff Training
The introduction of AI technologies requires significant change management efforts to ensure successful adoption. Staff members may require training on new systems and processes, and organizations must address potential resistance to technological change.
Effective change management includes clear communication about the benefits of AI implementation, adequate training programs, and ongoing support to help staff adapt to new workflows and responsibilities.
Quality Assurance and Oversight
While AI systems demonstrate impressive accuracy, healthcare organizations must maintain appropriate oversight and quality assurance measures. Human review remains essential for complex credentialing decisions and situations that fall outside the parameters of AI algorithms.
Organizations must establish clear protocols for when human intervention is required and ensure that staff members maintain the expertise necessary to provide effective oversight of AI-driven credentialing processes.
Future Trends and Developments
Blockchain Integration
The integration of blockchain technology with AI credentialing systems represents an emerging trend that could further transform the credentialing landscape. Blockchain’s immutable record-keeping capabilities could provide additional security and verification for credentialing information while enabling more efficient sharing of verified credentials across healthcare organizations.
Advanced Predictive Capabilities
Future AI systems will likely incorporate more sophisticated predictive capabilities, enabling healthcare organizations to anticipate credentialing needs and potential issues with greater accuracy. These systems may analyze broader datasets to predict provider performance, identify optimal credentialing strategies, and support strategic workforce planning decisions.
Standardization and Interoperability
The healthcare industry is moving toward greater standardization of credentialing processes and data formats, which will enhance the effectiveness of AI systems. Improved interoperability between different AI credentialing platforms will enable more seamless sharing of verified credentials and reduce duplication of verification efforts.
Regulatory Technology (RegTech) Integration
The integration of AI credentialing systems with regulatory technology solutions will provide enhanced compliance monitoring and reporting capabilities. These integrated systems will automatically track regulatory changes, update credentialing requirements, and ensure ongoing compliance with applicable standards.
Implementation Strategies for Healthcare Organizations
Phased Implementation Approach
Healthcare organizations considering AI credentialing solutions should adopt a phased implementation approach that allows for gradual system integration and staff adaptation. Beginning with pilot programs for specific credentialing activities enables organizations to evaluate AI effectiveness while minimizing disruption to ongoing operations.
Successful phased implementation typically begins with automated document processing or verification tasks before progressing to more complex applications such as risk assessment or predictive analytics.
Vendor Selection and Partnership
Choosing the right AI credentialing solution provider is crucial for successful implementation. Organizations should evaluate vendors based on their healthcare industry experience, system integration capabilities, data security measures, and ongoing support services.
Strong vendor partnerships that include implementation support, training, and continuous system optimization are essential for maximizing the benefits of AI credentialing investments.
Performance Measurement and Optimization
Healthcare organizations must establish clear metrics for measuring AI credentialing system performance, including processing time reduction, accuracy improvements, cost savings, and user satisfaction. Regular performance monitoring enables organizations to identify optimization opportunities and ensure that AI systems continue to meet organizational needs.
Continuous improvement processes should incorporate feedback from credentialing staff, providers, and other stakeholders to guide system enhancements and feature developments.
Summary: AI in Medical Credentialing
![]()
The integration of artificial intelligence into medical credentialing represents a transformative shift that addresses longstanding challenges in healthcare administration. Automating routine tasks, accelerating verification processes, and improving accuracy allows AI technologies to enable healthcare organizations to maintain high credentialing standards while significantly reducing administrative burden and costs.
The benefits of AI implementation extend beyond operational efficiency to include enhanced compliance capabilities, improved risk assessment, and better resource utilization. The credentialing process will become increasingly more electronic, automated, streamlined, and effective.
However, successful AI implementation requires careful planning, appropriate oversight, and ongoing optimization. Healthcare organizations must address data security concerns, manage change effectively, and maintain appropriate human oversight to realize the full benefits of AI credentialing solutions.

