Measuring and monitoring the right key performance indicators (KPIs) for medical credentialing can mean the difference between a thriving practice and one struggling with revenue cycles. Undermentioned, the essential metrics that every healthcare practice should track to ensure efficient credentialing processes and maintain healthy revenue streams.
Understanding the Importance of Credentialing Metrics
Before diving into specific KPIs, it’s crucial to understand why measuring credentialing performance is so vital.
Credentialing isn’t just a box-checking exercise, it’s a fundamental process that directly impacts:
- Revenue cycle management
- Patient satisfaction
- Provider satisfaction
- Compliance requirements
- Practice reputation
- Operational efficiency
By tracking the right metrics, practices can identify bottlenecks, prevent revenue leakage, and optimize their credentialing processes for better outcomes.
Essential Time-Based KPIs
1. Total Credentialing Cycle Time

This fundamental metric measures the entire credentialing process from start to finish. The clock starts ticking when you begin collecting provider information and stops when the provider receives final approval from all payers.
Key components to track include:
- Initial application completion time
- Primary source verification duration
- Payer processing time
- Follow-up and resolution periods
Industry benchmarks suggest that optimal credentialing cycle times should fall between 60-90 days, though this can vary by specialty and region. Breaking down this metric by payer can reveal which insurance companies consistently take longer to process applications, allowing for better planning and expectation setting.
2. Application Processing Time
This metric focuses specifically on the time your team spends preparing and submitting credentialing applications.
It should track:
- Document collection duration
- Application form completion time
- Quality review periods
- Submission processing time
Efficient practices typically complete initial application processing within 5-7 business days.
Longer durations might indicate:
- Insufficient staffing
- Inefficient processes
- Technology limitations
- Training gaps
3. Verification Response Times
Tracking how long it takes to receive responses from various verification sources helps identify bottlenecks and plan accordingly.
Monitor response times for:
- Educational institutions
- Previous employers
- Licensing boards
- Professional references
- Hospital affiliations
Create separate benchmarks for each verification type, as they typically have different response patterns.
For example:
- Educational verification: 5-10 business days
- Employment verification: 3-7 business days
- License verification: 1-3 business days
- Reference responses: 7-14 business days
Accuracy and Quality Metrics
1. Application Accuracy Rate
This critical metric measures the percentage of applications submitted without errors or omissions.
Track:
Error Types
- Missing information
- Incorrect data entry
- Outdated documentation
- Signature issues
- Incomplete forms
Error Sources
- Provider input
- Staff processing
- System integration issues
- Communication gaps
A high-performing credentialing department should maintain an application accuracy rate of 95% or higher.
Lower rates may indicate:
- Need for additional training
- Process improvement opportunities
- Technology upgrade requirements
- Resource constraints
2. First-Time Approval Rate
This metric measures the percentage of applications approved without requiring additional information or corrections.
It’s a key indicator of process efficiency and should include:
- Initial submission success rate
- Payer-specific approval rates
- Specialty-specific patterns
- Provider-level tracking
Industry leaders typically achieve first-time approval rates of 85-90%.
Lower rates might suggest:
- Application quality issues
- Missing documentation patterns
- Payer-specific challenges
- Training opportunities
Financial Impact Metrics
1. Revenue Impact Tracking
Monitor the financial implications of credentialing processes through:
Revenue Delay Metrics
- Dollars held in pending status
- Average revenue delay per incomplete credential
- Revenue impact by payer
- Specialty-specific financial impact
Lost Revenue Tracking
- Non-recoverable claims due to credentialing gaps
- Retroactive billing limitations
- Patient transfer costs
- Referral network impacts
2. Credentialing Cost Metrics
Track all expenses associated with credentialing activities:
Direct Costs
- Staff salaries and benefits
- Software and technology expenses
- Verification fees
- Training and education costs
Indirect Costs
- Administrative overhead
- Opportunity costs
- Compliance-related expenses
- Revenue cycle impact
Compliance and Risk Metrics
1. Expiration Tracking
Monitor upcoming expirations and renewal requirements for:
- Medical licenses
- DEA registrations
- Board certifications
- Insurance policies
- Hospital privileges
- Payer enrollments
Track the percentage of credentials updated before expiration, aiming for 100% compliance.
Key metrics include:
- Advance notice effectiveness
- Renewal submission timing
- Gap occurrence rates
- Resolution timeframes
2. Compliance Rate Metrics
Measure adherence to regulatory requirements and internal policies:
Documentation Compliance
- Complete file percentage
- Missing document patterns
- Update frequency compliance
- Audit readiness scores
Process Compliance
- Policy adherence rates
- Procedure following percentage
- Documentation accuracy
- Verification completeness
Operational Efficiency Metrics
1. Workload Distribution Metrics
Track how credentialing work is distributed and managed:
Staff Productivity Metrics
- Applications processed per staff member
- Verification completion rates
- Follow-up efficiency
- Quality scores
Resource Utilization
- Staff capacity usage
- Technology utilization rates
- Peak period management
- Overtime requirements
2. Process Efficiency Metrics
Monitor the effectiveness of credentialing procedures:
Automation Metrics
- Automated vs. manual processes
- System integration effectiveness
- Digital adoption rates
- Error reduction impact
Communication Efficiency
- Response time tracking
- Information flow metrics
- Stakeholder engagement
- Update effectiveness
Provider Satisfaction Metrics
1. Provider Experience Tracking
Measure provider satisfaction with credentialing processes:
Satisfaction Surveys
- Process satisfaction scores
- Communication effectiveness ratings
- Support availability feedback
- Overall experience metrics
Provider Engagement
- Response time satisfaction
- Update process feedback
- Portal usage rates
- Support request patterns
2. Provider Portal Metrics
If using a provider portal, track:
- Portal adoption rates
- Document submission patterns
- Self-service utilization
- Technical support needs
Technology Performance Metrics
1. System Efficiency Metrics
Monitor the performance of credentialing software and systems:
Technical Metrics
- System uptime
- Processing speed
- Integration effectiveness
- Error rates
User Metrics
- User adoption rates
- Feature utilization
- Training effectiveness
- Support ticket patterns
2. Data Quality Metrics
Track the accuracy and completeness of credentialing data:
Data Accuracy
- Error detection rates
- Correction frequencies
- Validation success rates
- Consistency scores
Data Completeness
- Required field completion
- Optional field utilization
- Update frequency
- Version control effectiveness
Communication and Coordination Metrics
1. Stakeholder Communication Metrics
Monitor communication effectiveness with all stakeholders:
Internal Communication
- Team coordination scores
- Update effectiveness
- Process alignment
- Information flow metrics
External Communication
- Payer interaction metrics
- Provider communication effectiveness
- Facility coordination
- Vendor management
2. Follow-up Effectiveness
Track the success of follow-up procedures:
- Resolution rates
- Response times
- Escalation patterns
- Completion tracking
Continuous Improvement Metrics
1. Process Improvement Tracking
Monitor the effectiveness of improvement initiatives:
Implementation Metrics
- Change adoption rates
- Impact assessment
- Cost-benefit analysis
- Time-to-value tracking
Outcome Metrics
- Efficiency gains
- Cost reductions
- Quality improvements
- Satisfaction increases
2. Training and Development Metrics
Track staff development and capability improvement:
- Training completion rates
- Skill assessment scores
- Performance improvement
- Knowledge retention
Setting Up a Metrics Program
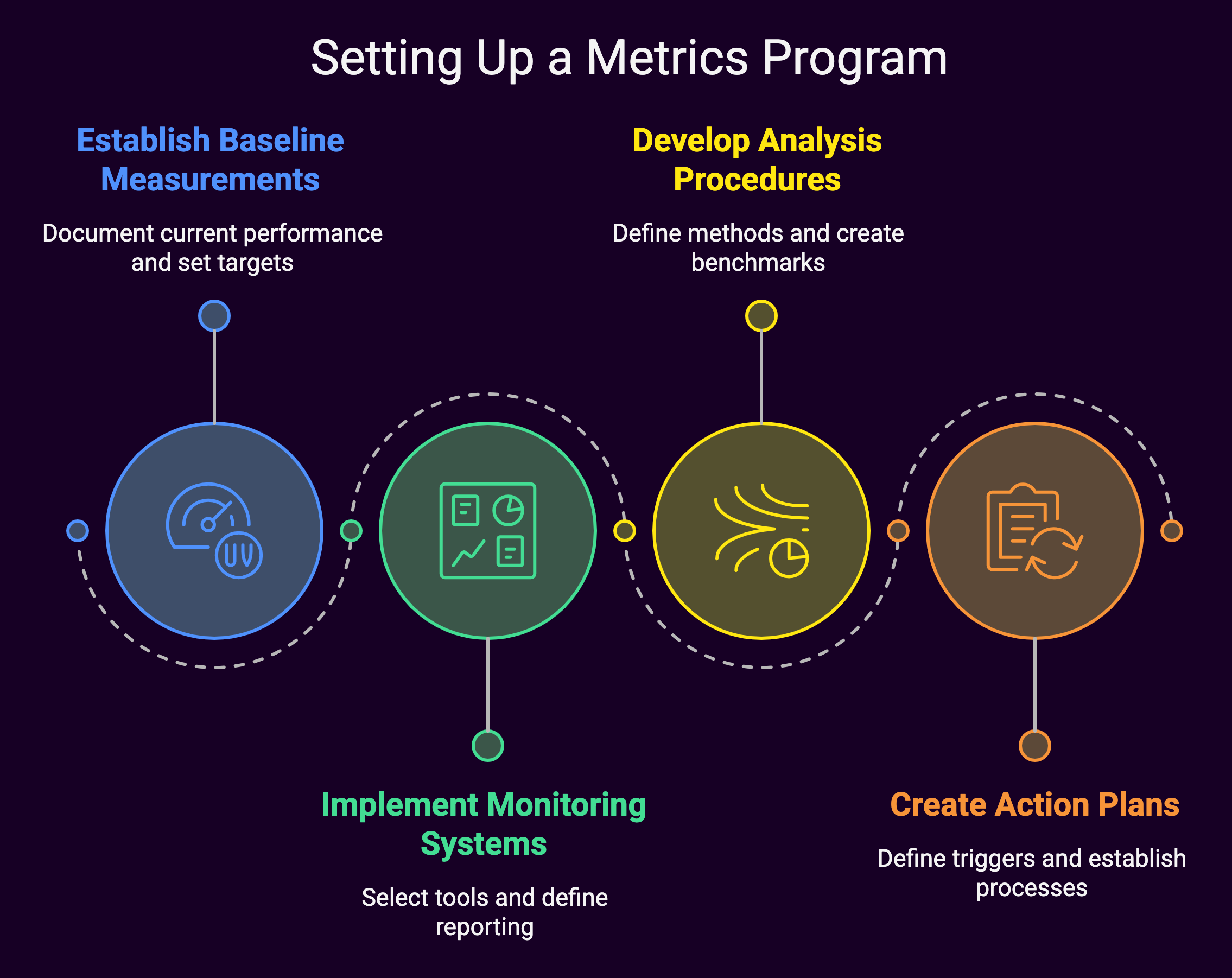
To effectively implement these KPIs, practices should:
1. Establish Baseline Measurements
- Document current performance
- Set realistic targets
- Define measurement periods
- Create tracking mechanisms
2. Implement Monitoring Systems
- Select appropriate tools
- Define reporting frequencies
- Establish review processes
- Create accountability measures
3. Develop Analysis Procedures
- Define analysis methods
- Create comparison benchmarks
- Establish trend monitoring
- Set up alert systems
4. Create Action Plans
- Define response triggers
- Establish improvement processes
- Set up feedback loops
- Monitor effectiveness
Summary: Crucial Medical Credentialing KPIs and Metrics
Tracking the right credentialing KPIs is essential for maintaining efficient operations and healthy revenue cycles.
Successfully implementing these metrics requires:
- Clear organizational commitment
- Appropriate resource allocation
- Effective technology utilization
- Regular monitoring and adjustment
- Continuous improvement focus
By carefully selecting and monitoring these KPIs, practices can:
- Optimize credentialing processes
- Reduce revenue impacts
- Improve provider satisfaction
- Ensure compliance
- Drive operational efficiency
Remember that metrics should be:
- Relevant to practice goals
- Measurable with available resources
- Actionable for improvement
- Time-bound for tracking
- Regularly reviewed and updated
Start with the most critical metrics for your practice and gradually expand your measurement program as processes mature and capabilities improve. A regular review and adjustment of your metrics program ensures it continues to provide valuable insights for practice improvement and success.

