Let’s talk about something that might not be the most exciting topic, but it’s absolutely crucial if you want to play ball with the big leagues of healthcare insurance. We’re talking about credentialing. That oh-so-fun process of getting your ducks in a row to prove you’re legit and qualified to provide care to patients covered by major carriers.
 We know what you might be thinking: “Credentialing? Ugh, that sounds like a massive headache.” And you’re not wrong. iIt can definitely be a pain in the you-know-what. But, here’s the thing: if you want to get paid for treating patients from the biggest names in the insurance game, you gotta’ go through the credentialing process. It’s just part of the deal.
We know what you might be thinking: “Credentialing? Ugh, that sounds like a massive headache.” And you’re not wrong. iIt can definitely be a pain in the you-know-what. But, here’s the thing: if you want to get paid for treating patients from the biggest names in the insurance game, you gotta’ go through the credentialing process. It’s just part of the deal.
So, let’s break it down and talk about why credentialing is so important, and what you need to do to get credentialed with some of the biggest carriers out there.
The Big “Whys” of Credentialing
At its core, credentialing is all about protecting patients and ensuring they’re receiving care from qualified, competent professionals. Insurance companies have a responsibility to their members to make sure the providers in their networks meet certain standards – and credentialing is how they verify that.
It’s kind of like getting backstage passes to a concert. The venue wants to make sure you’re legit and not some random person trying to sneak in. They check your ID, your credentials, and make sure you’re supposed to be there. Same deal with insurance carriers and their provider networks.
It’s not just about keeping randos out, as credentialing also helps carriers maintain quality control and ensure their members have access to safe, effective care. By vetting providers and facilities, they can identify any potential red flags or issues that could impact patient safety or quality of care.
So, while it might seem like a hassle, credentialing is actually a pretty important part of keeping the whole healthcare system running smoothly and protecting patients.
The Network All-Stars
Now that we’ve covered the “whys” let’s talk about the “whos.” As in, who are the major health insurance carriers for which providers need to be credentialed?
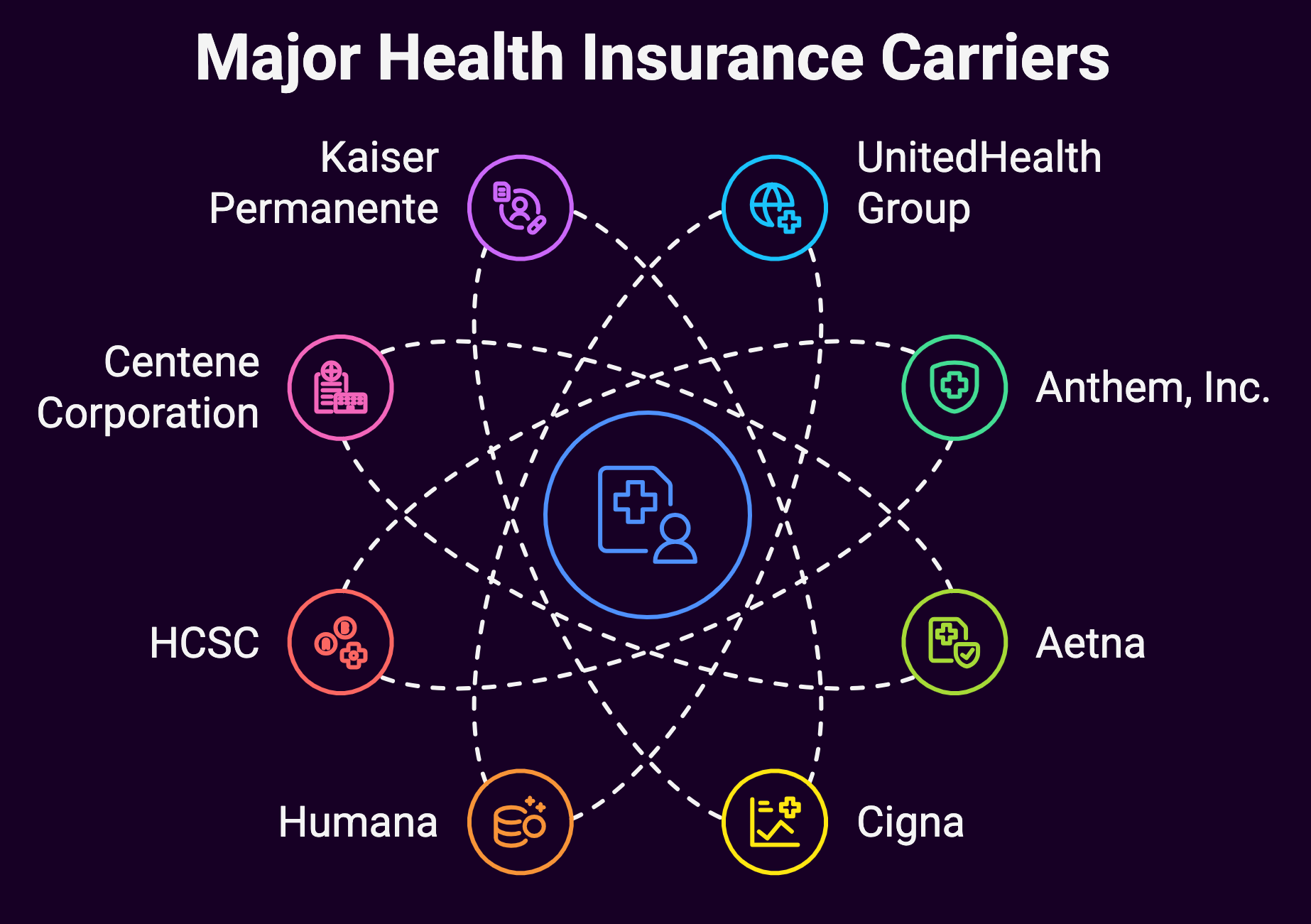
Here are some of the biggest names in the game:
UnitedHealth Group
As the largest single health carrier in the nation, UnitedHealth Group is a total powerhouse. If you want to be in their network and treat their millions of members, you better believe you’ll need to go through their credentialing process.
Anthem, Inc.
Anthem is another heavy hitter, operating Blue Cross Blue Shield plans in 14 states. Getting credentialed with Anthem can open up a whole lot of patient pools for providers.
Aetna
Now owned by CVS Health, Aetna is a name that pretty much every provider is familiar with. And you can bet they have a rigorous credentialing process to ensure quality care for their members.
Cigna
As a globally recognized health service company, Cigna takes credentialing seriously. If you want to be part of their network, be prepared to jump through some hoops to prove your worth.
Humana
With a big focus on Medicare Advantage plans, Humana is a major player – especially for providers treating older adults. And just like the other big names, they’ve got a credentialing process you’ll need to navigate.
Health Care Service Corporation (HCSC)
Operating Blue Cross Blue Shield plans in multiple states, HCSC is another big fish that providers will want to be credentialed with – especially if they practice in HCSC’s coverage areas.
Centene Corporation
As a leader in government-sponsored managed care programs like Medicaid and Medicare Advantage, Centene is a name that a lot of providers – especially those serving underserved populations – will need to be familiar with.
Kaiser Permanente
With their integrated managed care model, Kaiser Permanente has a bit of a unique approach to credentialing. But if you want to be part of their system, you’ll need to play by their rules.
Molina Healthcare
Another big player in government-sponsored healthcare programs, Molina Healthcare is focused on serving underserved communities. Getting credentialed with them can open up access to a lot of patients.
Highmark Health
Operating in several states, Highmark Health is a regional powerhouse that providers in their coverage areas will want to get credentialed with.
The Credentialing Playbook
Alright, now that we’ve covered the major players, let’s talk about what it actually takes to get credentialed with these big-name carriers.
While the specific requirements can vary a bit from carrier to carrier, there are some common threads:
Verification of Credentials
This is kind of the bread and butter of the credentialing process. Carriers want to make sure you are who you say you are and that you’ve got the education, training, licenses, and certifications to back up your credentials.
Expect to provide things like:
- Proof of education (transcripts, diplomas, etc.)
- Verification of any relevant training programs or residencies
- Current licenses and certifications for your specialty
- Board certification information (if applicable)
They’ll also dig into your professional history, checking for any gaps in employment, disciplinary actions, or malpractice suits that could raise red flags.
Background Checks
In addition to verifying your credentials, carriers will also conduct thorough background checks to ensure you don’t have any skeletons in the closet that could impact patient safety or the integrity of their network.
This usually involves criminal background checks, but may also include things like checking the Office of Inspector General’s List of Excluded Individuals/Entities (LEIE) to make sure you haven’t been excluded from participating in federal healthcare programs.
Insurance and Compliance
Another big part of the credentialing process is making sure you’ve got all your ducks in a row from an insurance and compliance standpoint.
Carriers want to see proof of things like:
- Professional liability insurance (malpractice insurance)
- General liability insurance
- Compliance with federal regulations like HIPAA
- Any other relevant state or local regulations
They need to know that you’re operating legally and have the proper protections in place to cover any potential incidents or issues.
Site Visits and Attestations
For facility-based providers like hospitals, surgery centers, or healthcare organizations, the credentialing process often involves site visits to assess things like:
- Physical environment and safety standards
- Staffing levels and qualification of personnel
- Adherence to clinical policies and procedures
- Infection control protocols
- Emergency management plans
Individual providers may also have to complete attestations related to their ability to perform certain procedures, their commitment to evidence-based practices, and their willingness to follow the carrier’s policies and protocols.
Ongoing Monitoring and Re-credentialing
It’s important to note that credentialing isn’t just a one-and-done thing. Most carriers require periodic re-credentialing (often every 2-3 years) to ensure that providers are maintaining standards and keeping up with any changes in regulations or requirements.
They’ll also monitor for any adverse events, disciplinary actions, or changes in status that could impact a provider’s standing in the network.
Credentialing Bottom Line
Credentialing is a rigorous process designed to ensure quality care and patient safety. The major carriers take it seriously, and providers need to be prepared to jump through all the necessary hoops. Get organized, be prepared to gather a mountain of paperwork, and consider enlisting some help to navigate the process. At Medwave, we can take a lot of the administrative burden off your plate, ensuring your applications are complete and giving you a better chance at getting credentialed smoothly. Credentialing is difficult; outsource it.

