 Medical billing has long relied on manual data entry and paperwork to process claims. But this antiquated approach is no longer sustainable in today’s digital healthcare environment.
Medical billing has long relied on manual data entry and paperwork to process claims. But this antiquated approach is no longer sustainable in today’s digital healthcare environment.
The future of medical billing lies with robotic process automation (RPA). RPA automates repetitive data entry and workflow tasks, increasing efficiency, reducing human error, and allowing medical billers to focus on more complex billing requirements and patient needs. Simply put, RPA can eliminate repetitive manual tasks, reduce billing costs, improve accuracy, and get claims paid faster. This technology represents a paradigm shift that will kill the old way of doing things.
Manual medical billing is dead, RPA is the answer.
The Problem with Manual Billing
For decades, medical billing relied on data entry clerks manually transcribing information from patient charts into billing systems.
This cumbersome process was riddled with problems:
- Prone to human error – Studies estimate manual data entry error rates between 5-15%. Typos and mistakes inevitably lead to costly claim denials and revenue loss.
- Inefficient use of staff time – Data entry is tedious and repetitive work that is not the best use of skilled medical billers’ expertise. Yet it takes up much of their day.
- Compliance risks – Billing regulations are complex. Humans can easily make errors staying on top of rules, leading to compliance violations.
- Long revenue cycles – Manual billing is time-consuming. It takes on average 25-35 days to collect on claims. The longer the revenue cycle, the longer practices go without getting paid.
- High costs – Manual workflows require large billing departments to keep up. This overhead expense reduces profit margins.
- Limited analytics – Humans cannot track metrics and identify trends as well as technology. This hampers a practice’s ability to optimize workflows.
- Poor scalability – Adding more patients or staff inevitably creates billing backlogs. It is hard to scale manual processes to handle growth.
These inefficiencies became especially pronounced as healthcare became more complex. The average medical bill now has over 100 fields that must be completed with precise data. As healthcare modernized, medical billing remained stubbornly antiquated. It became clear change was needed to enter the digital age.
The Promise of Automation
Other industries automated repetitive clerical tasks long ago. Yet, healthcare was slow to modernize its labor-intensive billing operations. That finally changed with the advent of robotic process automation. RPA uses software “robots” or “bots” to automate repetitive rules-based tasks. RPA mimics human actions and can rapidly enter data, transfer files, trigger responses, and communicate with other systems. Healthcare finally adopted RPA as it became obvious manual billing could not keep up with increasing complexity.
RPA delivers transformative results for medical billing:
- Improves accuracy – Bots are 100% consistent and do not make mistakes on repetitive tasks like humans. RPA eliminates transcription errors that lead to denied claims.
- Increases efficiency – Software robots work tirelessly 24/7 without breaks. RPA completes billing tasks 3x faster than humans. It reduces billing costs by up to 70%.
- Frees up staff – With bots handling routine tasks, billers can focus on value-added work like denial management and patient questions. This improves job satisfaction.
- Ensures compliance – RPA is programmed to strictly follow all billing rules and requirements. It reduces risk of costly fines for non-compliance.
- Shortens revenue cycles – Automation accelerates claims processing to get invoices paid faster. This improves cash flow for the practice.
- Enhances analytics – RPA provides data to track metrics and pinpoint issues. This yields insights to optimize workflows.
- Scales easily – Bots handle increased workloads without adding staff. RPA creates elasticity to smoothly handle patient volume growth.
- Improves patient experience – Faster and more accurate billing means fewer mistakes and hassles for patients to deal with.
These benefits make it evident why RPA is revolutionizing medical billing. It effectively eliminates the inefficiencies of manual processes. This is fueling the rapid enterprise adoption of RPA across healthcare.
Implementing RPA in Medical Billing
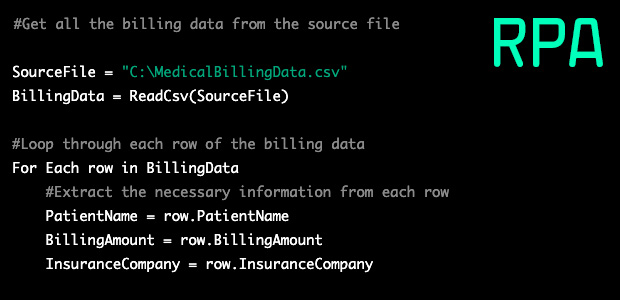
Transitioning from manual to automated billing using RPA involves three key steps:
- Process Selection – The first step is to map out existing billing workflows to identify which ones are suitable for automation based on volume, repetition, and labor intensity. Primary candidates include claims data entry, charge entry, payment posting, denial management, and reporting.
- Software Configuration – Next chosen processes are programmed for automation. This involves capturing rules and steps to replicate tasks. Billing rules and clinical nuances are accounted for to ensure accuracy. APIs may be utilized to integrate RPA with patient accounting systems, EHRs, clearinghouses, and payers.
- Testing and Deployment – Extensive testing ensures the bots are totally accurate before deployment. Billing staff should provide feedback. Bots are continually monitored and optimized after launch. RPA can be deployed incrementally or enterprise-wide.
It is vital to get staff onboard rather than view bots as a threat. RPA augments human capabilities rather than replaces jobs. The improved productivity and job satisfaction ultimately benefit employees. Change management and training help the transition. The process requires careful planning but brings tremendous upside.
Transforming Medical Billing Performance
Adopting RPA can transform medical billing.
Consider these results from real healthcare organizations:
- A hospital cut A/R days from 75 to 55 using RPA for charge capture and coding. This freed up $14 million in working capital.
- A health system achieved 98% claim submission accuracy using automation versus 80% manually. Denials were slashed by 89%.
- A clinic’s patient account representatives processed 300 claims per day with RPA versus only 100 manually.
- A surgical center reduced billing costs by 40% and improved cash flow by 20% with end-to-end billing automation.
- A multi-site medical group increased collections by $5.2 million annually using RPA despite seeing a 15% rise in patient volume.
These examples demonstrate the paradigm shift possible with billing automation. Organizations are seeing costs plummet, accuracy soar, staff productivity multiply, and cash flow accelerate. RPA pays for itself rapidly while providing a substantial ROI. It truly takes medical billing performance into a new realm.
Overcoming Obstacles to Adoption
Despite the strong rationale for RPA in billing, obstacles have slowed wider adoption so far.
These barriers include:
- Integration challenges – Complex IT landscapes make integrating disparate systems tricky. RPA vendors are addressing this by developing turnkey solutions and pre-built connections.
- Security concerns – Handling sensitive patient data requires proper governance to ensure safety and compliance. Cloud-based RPA tools have robust security capabilities.
- Unexpected costs – While automation reduces labor expenses, there are upfront technology and implementation costs. The ROI typically justifies these investments.
- Change resistance – Some staff view RPA as a job threat or dislike switching systems. Leadership must foster an embracing culture via training and open communication.
These concerns are valid but can be overcome. Vendors work closely with clients to ensure smooth implementations that deliver ROI. The benefits clearly outweigh the costs for organizations ready to modernize.
The Outlook for Automated Billing
Gartner forecasts RPA adoption will keep accelerating as it expands across healthcare. By 2024, 90% of large healthcare systems will have deployed some form of RPA, up from less than 30% in 2021. By 2025, Gartner projects healthcare RPA spending will reach $1.3 billion.
Forrester also sees healthcare as the third largest adopter of RPA behind banking and insurance. It expects by 2023 half of healthcare organizations will employ RPA across front and back offices. Software robots will join the workforce in every major healthcare role from patient access to revenue cycle.
These projections make sense given the immense pressure on providers to digitize operations. COVID-19 also propelled adoption as automation helped manage surges in claims volume and staff shortages. Healthcare is reaching an inflection point with billing along with automation in other areas like patient engagement and population health management.
The types of RPA applications will also expand as the technology matures. Currently RPA focuses on structured data tasks. Incorporating unstructured data from images, PDFs and EHR notes will unlock even more use cases. Advances in artificial intelligence like machine learning and natural language processing allow more complex capabilities like handling patient inquiries. This will shape the next generation of smart bots.
The healthcare organizations that embrace RPA will reap substantial first-mover advantages. They will establish efficient future-proofed billing for the digital era. On the other hand, those that cling to obsolete manual processes risk competitive disadvantage. The clock is ticking to get onboard the RPA revolution in medical billing.
Preparing the Medical Billing Workforce
As routine billing work shifts from humans to machines, the responsibilities of billing staff will evolve as well. Technology will take over data entry and paperwork, freeing up human staff for higher-value duties. This requires retraining the workforce to thrive in an automated environment.
Here are ways medical billers can prepare for the increased use of RPA:
- Become fluent with RPA tools to maximize their capabilities. This may require learning new interfaces and functionalities.
- Leverage freed-up time for value-added tasks like denial prevention and complex claim resolution that require human discernment and relationships.
- Upskill on data analytics to derive insights from billing data and pinpoint workflow improvements. Data interpretation skills are essential.
Summary
Manual medical billing is no longer viable in modern healthcare. The future inevitably belongs to automated processes that boost efficiency and lower costs. RPA represents a game-changing technology that will kill the old way of doing things. Adoption is accelerating as forward-thinking healthcare organizations realize the huge benefits.
RPA improves billing accuracy, shortens revenue cycles, reduces overhead, ensures compliance, and enhances analytics. This empowers staff and delights patients. While overcoming some adoption obstacles, RPA provides a substantial ROI for those ready to transition into the digital age.
Medical billing jobs will be transformed rather than eliminated. Staff must embrace automation and use it as an ally to focus on higher-value responsibilities. With the right preparation, a bright future awaits for both human and robotic billers. The time is now to bury manual processes and realize the promise of an automated approach. RPA provides the answer to take medical billing into the modern era. The death of manual billing marks a new promising chapter for healthcare’s financial operations.