RPA is Key to Improving Revenue Cycle Management
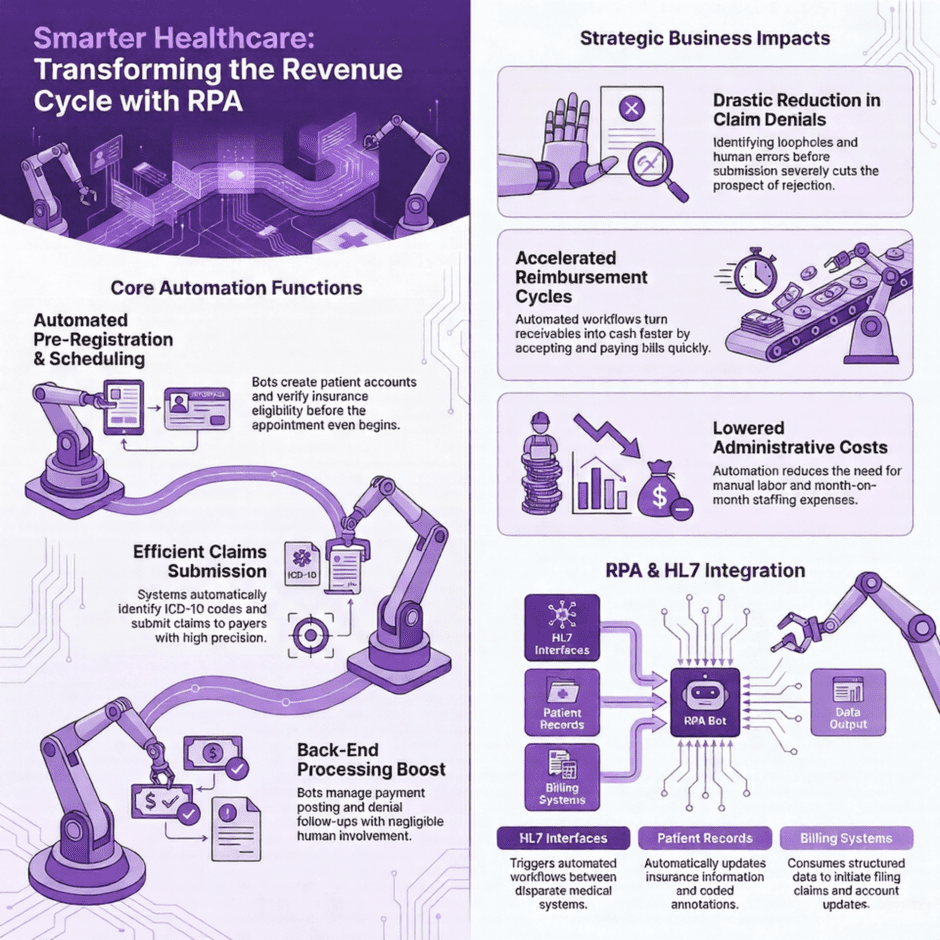
Robotic Process Automation (RPA) refers to the use of software robots to smartly automate repetitive and rule-based tasks. Within healthcare revenue cycle management, RPA can be used to streamline various tasks such as claims submission, payment posting, and denial management.
For example, an RPA system can be programmed to automatically retrieve patient data from electronic health records, verify insurance eligibility, submit claims to insurance companies, and follow up on any claim denials. This automation can significantly reduce the time and effort required for these tasks, improve accuracy and efficiency, and allow healthcare staff to focus on more complex tasks that require human expertise.
Additionally, robotic process automation can also help healthcare organizations reduce costs associated with medical billing by eliminating errors, reducing the need for manual labor, and improving the speed of processing claims. Overall, automation can be an effective tool to help healthcare organizations improve their revenue cycle management and ultimately provide better care to their patients.
Systematic Revenue Cycle Management
The following factors must be addressed:
- Scheduling appointments – The process of producing a methodical yet patient-centered procedure of scheduling appointments that provides the patient the time priority needed.
- Insurance eligibility certification – The insurance specifics and eligibility criteria required from the patient and then confirmed through the proper procedures.
- Setting up a patient account – A procedure that initiates the patient’s account within the healthcare organization and is constantly brought up to date based on subsequent services provided.
- Medical history ID – The upkeep of a detailed record that looks into into the patient’s medical history and all the pertinent issues that may or may not affect the patient’s health.
- Insurance coverages – Pinpointing the patient’s insurance authorizations and coverage and their impact on the processes for claims reimbursement, denial management, etc.
- Patient claims history – An analysis of the history of the patient that identifies if any claims have been rejected in the past, along with a record of the denial management.
- Medical billing – The process of producing accurate medical bills for the services provided.
Automating the Revenue Cycle
Revenue Cycle Automation
- Pre-registration – An automated procedure that produces an account for the patient, including medical history specifics, insurance coverage and all other relevant information.
- Patient scheduling – This process creates an efficient method to arranging initial patient appointments and all following appointments, with the patient always as the chief concern.
- Automated billing – Invoices are generated via basic data entries in which claims are pinpointed, verification carried out, medical bills created, and claims submitted, all in the most efficient manner.
- Reduced claims rejection and claims returned – Via the ability to recognize loopholes and human errors, the prospect of claims denial is severely cut.
- Effective claims submission – The identification of the ICD-10 code is automated via clear-cut data entries, along with the description of treatments required. As a direct result, reimbursement is much quicker.
- Charge capture duties identified – All services that convert into billable charges are detected and documented through automatic significance.
- Back-end processes boosted – Even after the claims are tendered, the additional processes of payment posting, handling of statements, collection of income and claims rejections or denials are managed via the automated software with negligible human involvement.
- Faster turnaround – These automated processes inherently turn into faster receivables with claims accepted and bills being paid at a much faster rate.
- Reduction in costs – The need for administrative staff is lessened through automated systems and saves the month-on-month cost of extra staff.
Healthcare Revenue Cycle Workflow Automation in Practice
The objective of workflow automation is to make best use of a healthcare facility’s revenue cycle and make sure claims are paid swiftly. This is a win-win. The healthcare provider collects timely payment, while patients go through a effortless, error-free visit to the doctor.
To realize these two goals (an enhanced revenue cycle and claims paid swiftly) it’s important to gather correct information from the very start, when a patient account is initiated.
In a recent case study, it was found that employees at a hospital in New York were obliged to accomplish tiresome tasks and enter relative data. Repetitive work can clearly lead to weariness and unintended mistakes. As a result, the hospital team realized the need to modernize these procedures and instigate workflows and systems to enhance accuracy and make sure the best exercise of personal time.
Since workflow is a cycle, each step flows into the ensuing step. If the original information is recorded with mistakes or essential information is missing, small errors can result in major problems in later steps.
Workflow Automation Subsists to Rid These Errors
Healthcare revenue cycle workflow automation systems achieve the following tasks:
- Concentrate on front-end tasks to push claims along
- Migrate patient files and produce non-patient files
- Proactively confirm and revise patient information
- Automatically add coded annotations
- Substantiate insurance information before a patient’s visit
- Revise obsolete or missing policies prior to an appointment
Why Workflow Automation Should Matter
As a decision-maker at a healthcare facility, you’re devoted to boosting revenue and reducing the costs of your facility. Automation helps make this stress-free. When healthcare facilities invest in workflow automation software, they benefit it two main ways: reducing expenses and improving workflow.
By making an investment in a system to proactively double-check patient information, healthcare facilities can reduce human error, enhance the organization’s revenue cycle workflow, curtail expenses and devote more time on revenue-generating, value-added efforts.
Medical Billing Robotic Process Automation is not only a shrewd investment, but a healthy one.
HL7
 The adoption of HL7 messaging standards allows for easier system integration and interoperability within healthcare organizations. This creates an opportunity to leverage robotic process automation to consume data from HL7 interfaces to drive workflows between disparate systems. RPA bots can interpret data in HL7 format exchanged between electronic medical records, billing systems, imaging repositories and more to automatically initiate processes like creating patient accounts, updating insurance information, filing claims and beyond.
The adoption of HL7 messaging standards allows for easier system integration and interoperability within healthcare organizations. This creates an opportunity to leverage robotic process automation to consume data from HL7 interfaces to drive workflows between disparate systems. RPA bots can interpret data in HL7 format exchanged between electronic medical records, billing systems, imaging repositories and more to automatically initiate processes like creating patient accounts, updating insurance information, filing claims and beyond.
The structured data population of HL7 messages enables reliable bot-based transaction processing not otherwise achievable through unstructured data that would require more sophisticated AI.
Overall, HL7 integration lays a foundation of accessible, shared data upon which RPA bots can scale automation of repetitive tasks to improve healthcare productivity and efficiency. Tight coupling between standardized HL7 interfaces and RPA bot triggering will continue expanding as providers seek accelerated digital transformation strategies.
Reach out to us today, in order to hear about our RPA solutions and whether it’s a good fit against your claim volume, etc,. We can tackle all of your revenue cycle automation needs.
