You’re sitting at your desk, staring at another credentialing application that’s weeks overdue. Your office manager is juggling three other urgent tasks. Your new physician is frustrated because they still can’t see patients. And you’re wondering… is there a better way to handle this?
The answer might surprise you. After 25+ years in medical credentialing, we’ve watched countless practices wrestle with this exact question. Should you keep it in-house, or should you outsource it to credentialing specialists?
What Does In-House Credentialing Actually Cost You?
 Many physicians assume handling credentialing internally saves money. After all, you’re not writing checks to an outside company, right? But when you dig into the actual costs, the picture changes dramatically.
Many physicians assume handling credentialing internally saves money. After all, you’re not writing checks to an outside company, right? But when you dig into the actual costs, the picture changes dramatically.
The salary expense is just the beginning. A credentialing coordinator typically earns $45,000-$65,000 annually, depending on your location and their experience level. Add benefits, payroll taxes, and workers’ compensation insurance, and you’re looking at $60,000-$85,000 in total compensation. For a practice credentialing multiple providers, you might need more than one person, multiplying these costs.
But here’s what most practices miss. Beyond salary, you’re paying for recruitment costs when turnover happens (and it does happen), training time that can stretch 3-6 months before someone becomes proficient, ongoing continuing education to keep staff current on changing requirements, software licenses for credentialing management systems ($3,000-$10,000 annually), office space and equipment for credentialing staff, and the management time your practice administrator spends overseeing credentialing operations.
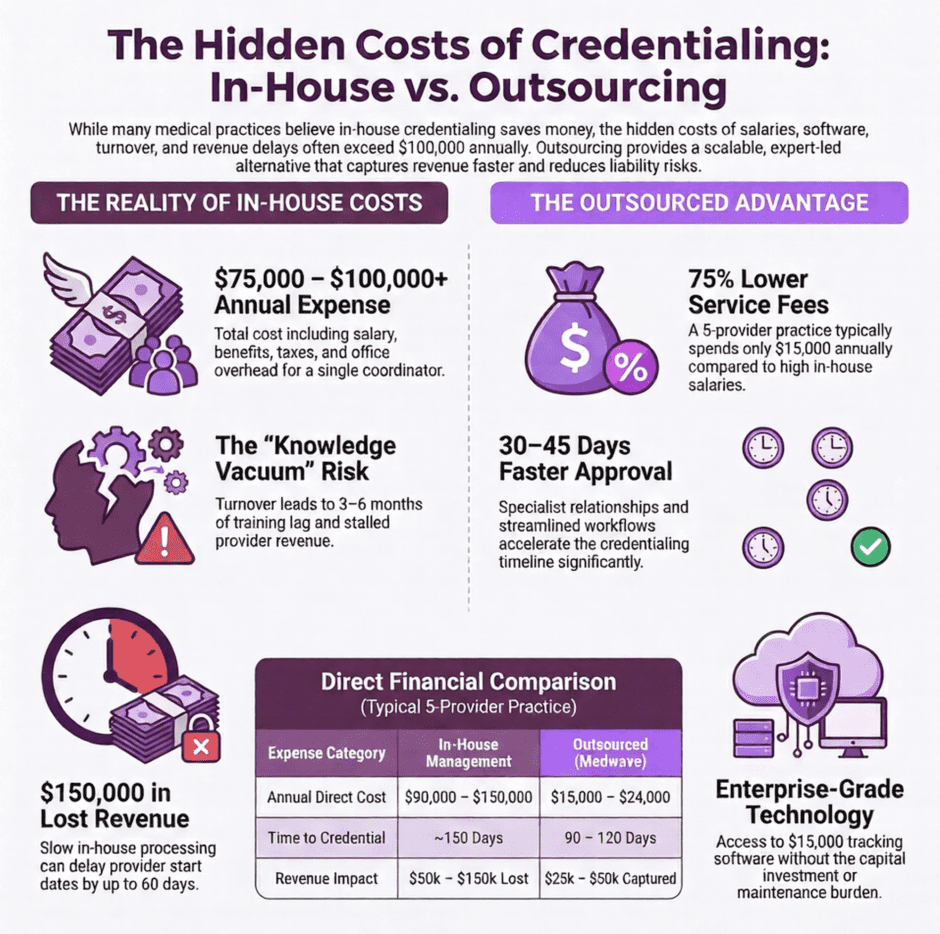
Add it all together, and your “free” in-house credentialing actually costs $75,000-$100,000+ per year for even a small practice. Larger practices with multiple locations and dozens of providers can easily spend $200,000-$300,000 annually.
What Happens When Your Credentialing Person Leaves?
Here’s a scenario we’ve seen play out dozens of times. Your credentialing coordinator gives two weeks’ notice. Suddenly, you’re facing a knowledge vacuum. Where are the pending applications? Which payers have which requirements? What deadlines are approaching?
The cost of turnover in credentialing roles is devastating. During the time it takes to find, hire, and train a replacement (typically 3-6 months), credentialing work either stops completely or gets handled poorly by staff with no training. New providers wait longer to start seeing patients, costing you thousands in lost revenue per week. Recredentialing deadlines get missed, potentially dropping providers out of insurance networks. Critical documents expire without anyone noticing.
We’ve watched practices lose six-figure sums because credentialing fell through the cracks during staff transitions. And it happens more often than you’d think, because credentialing is stressful, detail-oriented work with little recognition.
How Much Does Outsourced Credentialing Really Cost?
 Outsourced credentialing typically charges per provider, per month. Industry rates generally run $150-$400 per provider monthly, depending on the service level, number of providers, and how many payers you need.
Outsourced credentialing typically charges per provider, per month. Industry rates generally run $150-$400 per provider monthly, depending on the service level, number of providers, and how many payers you need.
Let’s do the math for a typical scenario. A practice with five providers paying $250 per provider monthly would spend $15,000 annually ($250 x 5 providers x 12 months). Even with ten providers, you’re looking at $30,000 per year.
Compare that to the $75,000-$100,000 you’d spend managing it in-house with one employee. The cost difference is substantial, and that’s before we factor in the value of faster credentialing, fewer errors, and your staff’s time freed up for other work.
Some practices worry about initial setup fees, which typically run $500-$1,500 per provider for getting everything organized and transferred to the credentialing company. Yes, that’s an upfront investment. But spread over the years you’ll work with a credentialing partner, it’s minimal compared to the ongoing savings and improved performance.
What About Speed and Revenue Impact?
Time equals money in healthcare, never more so than with credentialing. Every week a new provider waits for credentialing approval costs you actual revenue.
Let’s look at real numbers. A primary care physician typically generates $50,000-$75,000 in monthly revenue. If in-house credentialing takes 150 days instead of the 90-120 days a specialist achieves, you’re losing 30-60 days of revenue. That’s $50,000-$150,000 in lost collections per provider.
Credentialing companies have streamlined processes, established relationships with verification sources, and dedicated staff whose only job is moving applications through quickly. They know exactly who to call at medical schools, licensing boards, and payers. They’ve done this hundreds or thousands of times.
Your office manager trying to handle credentialing between managing staff schedules, dealing with patient complaints, and ordering supplies? They’re learning as they go, and speed suffers.
Do Credentialing Errors Really Cost That Much?
 One missed license expiration can shut down your entire practice overnight. We’ve seen it happen. One practice we consulted with had their physician’s license expire because their in-house coordinator was out sick during the renewal period and forgot to follow up. The practice couldn’t see patients for three days while they rushed the renewal through. Lost revenue: over $30,000. Patient frustration equals immeasurable.
One missed license expiration can shut down your entire practice overnight. We’ve seen it happen. One practice we consulted with had their physician’s license expire because their in-house coordinator was out sick during the renewal period and forgot to follow up. The practice couldn’t see patients for three days while they rushed the renewal through. Lost revenue: over $30,000. Patient frustration equals immeasurable.
Credentialing mistakes carry real financial consequences. Billing for services while credentialing has lapsed requires refunding all payments received, which can total tens of thousands of dollars. Missing recredentialing deadlines drops you out of insurance networks, requiring patients to go elsewhere. Inadequate background checks expose you to malpractice liability if something goes wrong. Errors in initial applications delay approvals by weeks or months while you fix them.
Professional credentialing companies have quality control processes specifically designed to catch these errors before they become problems. They maintain automated tracking systems that flag upcoming expirations months in advance. They have multiple reviewers check every application before submission.
Can you afford the same level of quality assurance in-house? Most practices can’t.
What’s Your Staff’s Time Actually Worth?
When your office manager or practice administrator spends 15 hours weekly on credentialing, that’s 15 hours they’re not spending on more valuable activities. What’s the opportunity cost?
Consider what else that time could accomplish. Your practice administrator could focus on negotiating better payer contracts (potentially worth thousands monthly in improved reimbursement). They could implement process improvements that increase patient throughput and revenue. They could develop staff training programs that reduce turnover and improve patient satisfaction. They could focus on recruiting and retaining high-quality clinical staff.
Every hour spent chasing down credentialing documents is an hour not spent on strategic initiatives that could grow your practice. That opportunity cost is real, even if it doesn’t show up on your profit and loss statement.
Can You Really Scale Credentialing In-House?
 Here’s where in-house credentialing really breaks down. Your practice needs vary throughout the year. Maybe you hire three new providers this quarter and none next quarter. Maybe you’re opening a new location next year that requires credentialing everyone at multiple new hospitals.
Here’s where in-house credentialing really breaks down. Your practice needs vary throughout the year. Maybe you hire three new providers this quarter and none next quarter. Maybe you’re opening a new location next year that requires credentialing everyone at multiple new hospitals.
In-house staff can’t flex up and down efficiently. If you have capacity to handle five credentialing projects simultaneously, what happens when you suddenly need to handle twelve? You either let timelines slip (costing revenue), pay overtime (increasing costs), or hire another person (who may not be needed once the rush is over).
Outsourced credentialing scales automatically. Need to credential ten new providers next month? Your credentialing company allocates additional resources to your account. Back to maintaining existing credentials? You’re only paying for what you need.
What About the Technology Investment?
Good credentialing requires good technology. Tracking systems for deadlines, document storage, workflow management, payer requirement databases, these tools aren’t cheap.
Quality credentialing software runs $3,000-$15,000 annually. And that’s just the license. You also need someone to maintain it, update it, back it up, and train staff how to use it. Most practices using spreadsheets and file folders for credentialing aren’t equipped to scale or maintain quality control.
When you outsource credentialing, you get access to enterprise-level technology without the capital investment. Your credentialing company has already made that investment and spreads the cost across many clients. You benefit from their technology without writing a check for software licenses.
How Do You Measure Quality and Compliance?
 Credentialing requirements change constantly. New payer policies, updated state regulations, revised accreditation standards, these changes happen monthly. Staying current requires dedicated attention.
Credentialing requirements change constantly. New payer policies, updated state regulations, revised accreditation standards, these changes happen monthly. Staying current requires dedicated attention.
Can your in-house staff keep up? Unless credentialing is their full-time job and they’re actively involved in professional associations, attending conferences, and networking with other credentialing specialists, probably not.
Credentialing companies employ certified credentialing specialists who make it their business to stay current. They’re members of NAMSS (National Association Medical Staff Services). They attend industry conferences. They share knowledge across their client base. When a payer changes their application process, they know immediately and adjust.
Your office manager might not find out until an application gets rejected.
What’s the Real Risk of Going It Alone?
The risks of in-house credentialing extend beyond financial costs. Compliance violations can result in accreditation problems, government audits, or network terminations. A single provider practicing with lapsed credentials creates liability exposure that could cost you everything.
We’ve seen practices face serious consequences from credentialing failures. One practice billed Medicare for six months while their physician’s Medicare enrollment was lapsed. They had to refund over $200,000 and faced penalties. Another practice missed a recredentialing deadline with their primary payer, dropping all providers out of network. They lost half their patients in three months.
These aren’t theoretical risks. They’re real situations that happen to real practices trying to manage credentialing without the expertise or systems to do it correctly.
Does Outsourcing Mean Losing Control?
 Many physicians worry that outsourcing credentialing means giving up control. What if the credentialing company makes mistakes? What if they don’t communicate well? What if you can’t see what’s happening?
Many physicians worry that outsourcing credentialing means giving up control. What if the credentialing company makes mistakes? What if they don’t communicate well? What if you can’t see what’s happening?
Here’s the Reality
Reputable credentialing companies provide more transparency than most in-house operations. You get online portals showing exactly where each credential stands. You receive regular status reports and alerts about deadlines. You have dedicated account managers you can reach directly.
Compare that to asking your office manager “Hey, where are we with Dr. Smith’s credentialing?” and getting a shrug because they haven’t had time to check in two weeks.
With the right credentialing partner, you actually gain visibility and control because you’re working with systems specifically designed for tracking and reporting credentialing status.
What Questions Should You Ask Before Deciding?
Making the in-house versus outsourced decision requires honest assessment of your situation.
Ask yourself these questions:
- About current costs: How much are you really spending on credentialing now (including all hidden costs)? How many hours per week do staff spend on credentialing? What’s the true cost of revenue delays from slow credentialing? What have credentialing errors cost you in the past year?
- About capability: Does your staff have certified credentialing expertise? How quickly can you handle urgent credentialing needs? What happens if your credentialing person quits tomorrow? How well do you track recredentialing deadlines and license expirations?
- About scalability: Are you planning to add providers or locations? Can your current process handle 2x or 3x the credentialing volume? What would it cost to expand your in-house capability?
Your honest answers to these questions will likely point you toward the right solution.
The Bottom Line on Costs and Benefits
After working in this field for over 25 years, we can tell you that the math almost always favors outsourcing for practices with fewer than 20 providers. The cost savings alone justify it. The speed improvements, error reduction, and strategic value of freeing up your staff’s time make it a clear winner.
Total Cost Comparison Break Down
In-House Credentialing for a 5-provider practice:
- Staff salary and benefits: $60,000-$85,000
- Software and technology: $3,000-$10,000
- Training and education: $2,000-$5,000
- Lost revenue from delays: $25,000-$50,000
- Total annual cost: $90,000-$150,000
Outsourced Credentialing for the same practice:
- Service fees: $15,000-$24,000
- Faster credentialing (revenue capture): +$25,000-$50,000
- Net annual cost: ($10,000) to $24,000
You’re either saving $66,000-$126,000 per year or actually making money compared to in-house credentialing because of faster revenue capture.
The larger your practice, the more providers you credential, the more locations you manage, the bigger these numbers get in favor of outsourcing.
How Medwave Makes the Difference
 At Medwave, we’ve spent over two decades perfecting the credentialing process. We handle billing, credentialing, and payer contracting for practices nationwide, and we’ve seen every possible credentialing scenario.
At Medwave, we’ve spent over two decades perfecting the credentialing process. We handle billing, credentialing, and payer contracting for practices nationwide, and we’ve seen every possible credentialing scenario.
Our team knows exactly how to get providers credentialed quickly and correctly. We maintain relationships with payers across the country. We use technology platforms specifically built for credentialing efficiency. And we back everything with quality assurance processes that virtually eliminate errors.
When you partner with us for credentialing, you’re gaining a strategic advantage that helps your practice grow faster, operate more efficiently, and avoid costly mistakes.
The practices we work with typically see new providers credentialed 30-45 days faster than they achieved in-house. They eliminate credentialing-related errors that previously cost them thousands in lost revenue. And their staff focuses on high-value activities instead of drowning in paperwork.
Ready to find out exactly what outsourced credentialing could save your practice? Contact us today for a personalized cost-benefit analysis based on your specific situation. We’ll show you the real numbers and help you make the decision that’s right for your practice.

