Medical credentialing represents one of the most significant administrative challenges facing both healthcare providers and organizations. What should be a straightforward process has evolved into a labyrinthine system of paperwork, verification steps, and regulatory compliance that consumes valuable time, resources, and energy. But there’s good news on the horizon: with the right approach and technology solutions, these credentialing headaches can be substantially reduced or even eliminated altogether.
The Credentialing Crisis
 Medical credentialing exists for an essential reason: to ensure patient safety by verifying that healthcare providers possess the proper qualifications, training, and experience to provide care. This fundamental process helps maintain quality standards across the healthcare industry and protect patients from unqualified practitioners.
Medical credentialing exists for an essential reason: to ensure patient safety by verifying that healthcare providers possess the proper qualifications, training, and experience to provide care. This fundamental process helps maintain quality standards across the healthcare industry and protect patients from unqualified practitioners.
However, the execution of this noble goal has become increasingly problematic. The average credentialing process can take anywhere from 90 to 180 days to complete, creating substantial delays in onboarding new providers. During this limbo period, qualified healthcare professionals remain unable to practice, organizations lose potential revenue, and patients experience reduced access to care. In an era of healthcare provider shortages, these inefficiencies represent a critical issue for the entire healthcare ecosystem.
Common Pain Points in Traditional Credentialing
What makes credentialing so challenging?
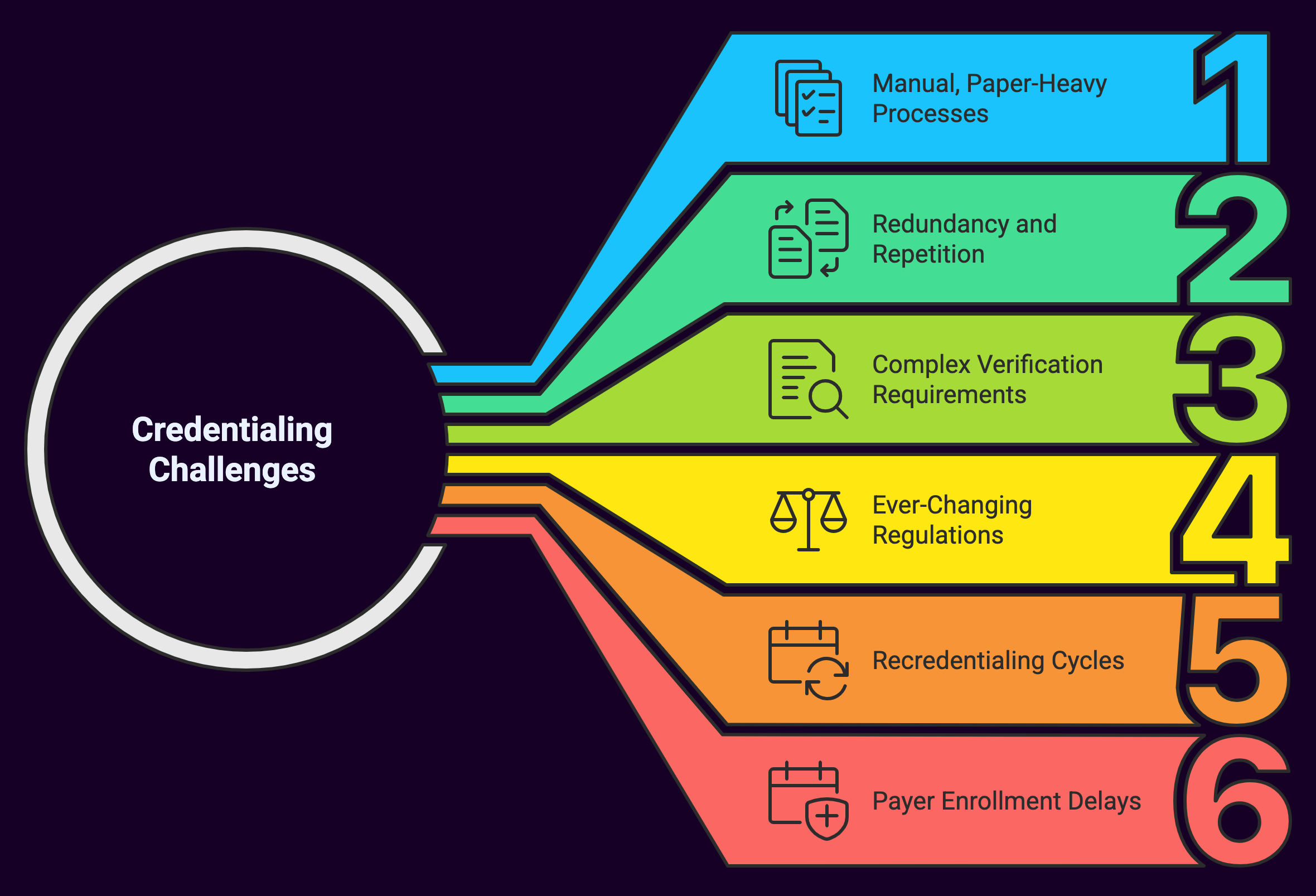
Let’s examine the most significant problems:
1. Manual, Paper-Heavy Processes
Despite technological advancements in virtually every other aspect of healthcare administration, credentialing often remains trapped in manual workflows that rely heavily on paper forms, physical signatures, and document shipping. Each provider application can involve hundreds of pages of documentation that must be meticulously reviewed, organized, and stored.
2. Redundancy and Repetition
Healthcare providers frequently practice at multiple facilities, yet each organization typically requires its own separate credentialing process, often requesting identical information in slightly different formats. This means physicians and other providers must repeatedly submit the same documentation, creating unnecessary duplication of effort.
3. Complex Verification Requirements
Primary source verification (the process of directly confirming a provider’s credentials with the original source) is both necessary and notoriously time-consuming. Credential verification organizations (CVOs) must contact educational institutions, previous employers, licensing boards, and other entities individually, often waiting weeks for responses.
4. Ever-Changing Regulations
Credentialing requirements continuously evolve based on changes in state regulations, payer policies, and accreditation standards. Keeping up with these changes requires constant vigilance and adaptation, placing additional burden on already-stretched credentialing departments.
5. Recredentialing Cycles
The work doesn’t end once a provider is initially credentialed. Most organizations require recredentialing every two to three years, creating a perpetual cycle of verification activities that must be managed across the entire provider roster.
6. Payer Enrollment Delays
After organizational credentialing comes payer enrollment. The process of getting providers approved to bill various insurance companies. Each payer has unique requirements and timelines, further extending the overall onboarding process and delaying revenue collection.
The Real-World Impact of Credentialing Challenges
These issues aren’t merely administrative inconveniences, they represent significant operational and financial problems:
For Healthcare Organizations:
- Lost revenue during credentialing delays (potentially $7,500 to $30,000 per provider per month)
- Increased administrative costs for credentialing staff
- Compliance risks from inadequate verification
- Delayed service implementation and practice growth
- Frustrated physicians and staff
For Healthcare Providers:
- Income loss during waiting periods
- Professional frustration and decreased satisfaction
- Career advancement delays
- Redundant paperwork requirements
- Confusion about application status
For Patients:
- Reduced access to needed specialists
- Longer wait times for appointments
- Potential care discontinuity
- Higher healthcare costs passed along from administrative inefficiencies
The Path Forward: Modernizing Credentialing Processes
The good news is that these problems are not insurmountable. Modern technology solutions designed specifically for healthcare credentialing can dramatically improve efficiency, reduce errors, and accelerate provider onboarding.
Here’s what an ideal approach includes:
1. Centralized Digital Data Management
Modern credentialing requires a secure, centralized platform where provider information can be stored, accessed, and updated in real-time. This eliminates redundant data entry and creates a single source of truth for provider credentials.
2. Automation of Routine Tasks
Many verification activities can be automated through integration with primary sources, including license verification, OIG/SAM checks, and National Practitioner Data Bank queries. Automation reduces both human error and processing time.
3. Intelligent Workflow Management
Advanced credentialing systems can track application progress, automatically assign tasks to appropriate team members, and flag exceptions that require human intervention, ensuring nothing falls through the cracks.
4. Document Management Capabilities
Digital document storage with OCR (optical character recognition) capabilities allows for quick retrieval and analysis of provider documents, eliminating paper files and enhancing security.
5. Integration Capabilities
Modern solutions should seamlessly connect with existing healthcare systems, including EHRs, HR platforms, and practice management software to ensure data consistency across systems.
6. Analytics and Reporting
Robust reporting provides visibility into process bottlenecks, credentialing timeframes, and upcoming renewal requirements, enabling continuous process improvement.
A Viable Solution to Credentialing Challenges
One organization at the forefront of transforming the credentialing landscape is Medwave. Our innovative approach to medical credentialing addresses the core problems faced by healthcare organizations while providing the technological foundation needed for long-term success.
How Medwave Transforms Credentialing
Medwave’s comprehensive credentialing solution tackles the traditional pain points head-on through several key capabilities:
Streamlined Digital Application Process
Medwave’s platform eliminates paper-based workflows through a user-friendly digital application system. Providers can complete applications online, upload documents directly to the secure system, and track their application status in real-time. This transparency improves provider satisfaction while dramatically reducing initial processing time.
Intelligent Automation
The platform incorporates intelligent automation throughout the credentialing workflow. Their system can automatically verify certain credentials through direct integrations with primary sources, trigger follow-up communications for missing information, and manage re-credentialing cycles proactively rather than reactively.
Customized Workflow Management
Understanding that every healthcare organization has unique requirements, Medwave offers customizable workflows that align with specific organizational policies and procedures. This adaptability ensures compliance with internal standards while maintaining optimal efficiency.
Comprehensive Provider Data Repository
At the heart of Medwave’s solution is a secure, centralized provider data repository that serves as the single source of truth for all credentialing information. This repository supports not only initial credentialing but also ongoing monitoring, privileging, and re-credentialing activities.
Integrated Payer Enrollment
Medwave extends beyond organizational credentialing to streamline the payer enrollment process as well. By managing both processes in a coordinated fashion, they help reduce the overall time-to-revenue for new providers.
Regulatory Compliance Monitoring
The healthcare regulatory landscape is constantly evolving. Medwave’s platform stays current with changing requirements from accreditation bodies, state licensing boards, and federal regulations, ensuring organizations remain compliant without dedicating excessive resources to regulatory tracking.
Analytics and Performance Insights
Through robust reporting and analytics capabilities, Medwave provides organizations with actionable intelligence about their credentialing operations. These insights help identify bottlenecks, measure process improvements, and quantify the return on investment from credentialing optimization.
Real Results: The Impact of Modern Credentialing Solutions
Organizations that implement modern credentialing solutions like Medwave’s typically experience significant improvements:
- Reduced Credentialing Timeframes: Processing times often decrease by 50% or more, allowing providers to begin practicing, and generating revenue, much sooner.
- Lower Administrative Costs: Automation reduces the staff time required for routine verification tasks, allowing credentialing specialists to focus on exception handling and more complex cases.
- Improved Data Accuracy: Digital systems with built-in validation reduce errors in provider data, enhancing compliance and patient safety.
- Greater Provider Satisfaction: Streamlined processes and transparent status updates lead to higher satisfaction among physicians and advanced practice providers.
- Enhanced Compliance: Systematic tracking of expiring credentials and automated alerts ensure timely re-credentialing and reduce compliance risks.
Implementing a Modern Credentialing Solution: Best Practices
For healthcare organizations considering a transition to a modern credentialing system like Medwave, several best practices can help ensure success:
1. Conduct a Thorough Process Analysis
Before implementing new technology, thoroughly document current workflows, identifying pain points, redundancies, and manual processes that could benefit from automation.
2. Establish Clear Success Metrics
Define what success looks like with specific, measurable targets such as reducing credentialing time from 120 days to 45 days or decreasing credentialing-related provider complaints by 75%.
3. Engage Stakeholders Early
Include representatives from all affected departments (medical staff office, provider recruitment, compliance, IT) in planning discussions to ensure the solution meets diverse needs.
4. Plan for Data Migration
Develop a comprehensive strategy for transferring existing provider data and documents to the new system, with careful attention to data validation and quality control.
5. Invest in Training
Thorough training for all system users is essential for realizing the full benefits of new technology. Budget adequate time and resources for initial and ongoing education.
6. Start with Quick Wins
Identify high-impact, relatively simple improvements that can demonstrate value quickly while building momentum for more complex changes.
Looking Ahead: The Future of Medical Credentialing
As healthcare continues to evolve, credentialing processes will need to keep pace with industry changes.
Forward-thinking organizations like Medwave are already exploring advanced capabilities:
Blockchain for Credential Verification
Blockchain technology offers the potential for immutable, instantly verifiable credential records that could dramatically accelerate verification processes while enhancing security.
Predictive Analytics
Advanced analytics can identify potential credentialing issues before they occur, allowing proactive intervention and further reducing delays.
Unified Provider Passports
Industry initiatives toward standardized credentialing data sets could eventually lead to “provider passports” that eliminate redundant verification across organizations.
Summary: Transforming Challenges into Opportunities
The credentialing problems facing healthcare organizations today are significant, yet solvable. With solutions like Medwave’s credentialing product, what has traditionally been a source of frustration can become a strategic advantage. Reducing costs, accelerating revenue capture, improving provider satisfaction, and ultimately enhancing patient care.
Embracing modern approaches to credentialing allows healthcare organizations to transform this necessary administrative function from a bottleneck into a catalyst for organizational success. The question is no longer whether credentialing problems can be fixed (with the right partner and technology, they absolutely can be), but rather how quickly organizations will seize the opportunity to revolutionize this critical function.

