Behavioral health professionals continue to face a complex and evolving landscape of reimbursement challenges. The good news? Strategic knowledge of Current Procedural Terminology (CPT) codes can significantly boost your practice’s financial health while ensuring you’re fairly compensated for the valuable services you provide.
Figuring out the nuances of behavioral health coding is no longer optional, it’s essential. The undermentioned content includes the latest updates to behavioral health CPT codes, uncover strategies to maximize your reimbursement, and provide practical tips for implementation that can make a tangible difference to your bottom line.
What’s New for 2025: Key CPT Code Changes
The behavioral health coding landscape has seen some meaningful shifts since last year.
Let’s break down the most significant changes that impact your practice:
Time-Based Service Revisions

The 2025 updates have brought refined time parameters for several key psychotherapy codes.
These adjustments better reflect the reality of clinical practice and provide more flexibility in service delivery:
- 90837 (Psychotherapy, 53+ minutes): Now allows for more specific documentation of extended sessions, with clearer guidelines on when to use add-on codes for sessions exceeding 60 minutes.
- 90834 (Psychotherapy, 38-52 minutes): Updated documentation requirements emphasize the need to record specific start and end times.
- 90832 (Psychotherapy, 16-37 minutes): Expanded clinical examples help clarify when this code is most appropriate versus using the crisis intervention codes.
Telehealth Permanence
Perhaps the most welcome change is the permanence of telehealth provisions that began during the COVID-19 pandemic.
After years of extensions and uncertainty:
- Telehealth services for most behavioral health CPT codes are now permanently reimbursable across all major payers
- Geographic restrictions have been largely eliminated
- Audio-only services remain billable for specific circumstances where video isn’t feasible
- Place of service (POS) coding has been streamlined with clearer distinctions between POS 02 (telehealth provided other than in patient’s home) and POS 10 (telehealth provided in patient’s home)
Collaborative Care Enhancements
The collaborative care model continues to gain traction, with enhanced reimbursement for coordination between behavioral health specialists and primary care providers:
- 99484 (Care management services for behavioral health conditions): Received a 12% increase in reimbursement for 2025
- 99492-99494 (Initial and subsequent psychiatric collaborative care management): Now include expanded eligible provider types, allowing licensed mental health counselors and marriage and family therapists to participate in collaborative care teams
New Assessment Codes
Several new assessment codes have been introduced to better capture the comprehensive nature of psychological and neuropsychological evaluations:
- 96146 (Psychological or neuropsychological test administration, with automated result only): Now includes specific parameters for digital therapeutics and assessments
- 96121 (Neurobehavioral status exam with interpretation and report, additional hour): Received clarification on documentation requirements and appropriate use cases
Strategic Coding for Maximum Reimbursement
Understanding the code updates is just the beginning. The real value comes from strategically implementing these codes to optimize reimbursement while maintaining compliance.
Let’s explore some powerful approaches:
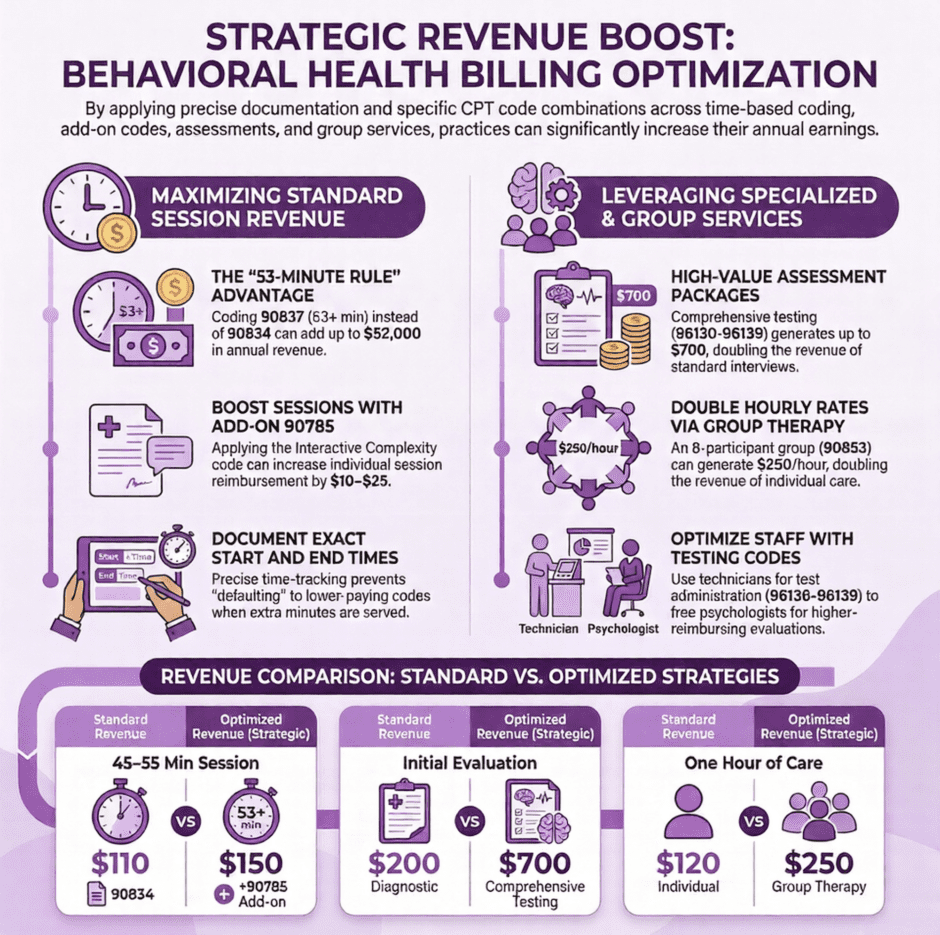
1. Master the Art of Time-Based Coding
Time-based codes remain the foundation of behavioral health billing, but many providers leave money on the table by imprecisely tracking and coding their time:
Practical Tip: Always document the exact start and end times of each session. When a session runs 52 minutes, don’t automatically default to 90834 (38-52 minutes) if you provided just one additional minute of service. That 53rd minute qualifies you for 90837, which typically reimburses at a higher rate.
Session began: 2:00 PM
Session ended: 2:54 PM
Total time: 54 minutes
CPT Code used: 90837 (53+ minutes)
Financial Impact: The difference between 90834 and 90837 can range from $15-40 per session depending on the payer. For a provider seeing 25 patients weekly, this attention to detail could generate an additional $19,500-52,000 annually.
2. Leverage Add-On Codes
Add-on codes are frequently underutilized but can substantially increase reimbursement for complex cases:
- 90785 (Interactive complexity add-on): Applicable when communication difficulties significantly complicate the delivery of care, such as when working with patients who have difficulty communicating, require the involvement of third parties, or exhibit high emotional reactivity
- 90833/90836/90838 (Psychotherapy add-on to E/M service): For psychiatrists and other qualified healthcare professionals who provide both medication management and psychotherapy in the same session
- 90840 (Psychotherapy for crisis, each additional 30 minutes): Ensures you’re properly compensated for extended crisis intervention services
Practical Tip: Review each session immediately after completion to identify any components that qualify for add-on codes. Create a quick reference sheet of common scenarios in your practice that warrant these codes.
Financial Impact: Regular use of the interactive complexity add-on code (90785) can increase session reimbursement by $10-25. If applicable to 30% of your caseload, this could add $3,900-9,750 annually for a provider seeing 25 patients weekly.
3. Optimize Assessment and Testing Services
Psychological and neuropsychological testing services typically reimburse at higher rates than therapy services, yet many providers don’t fully capture the extent of their assessment work:
- 96130-96133 (Psychological testing evaluation services): Now have clearer guidelines on the inclusion of test selection, integration of patient data, interpretation, and report writing
- 96136-96139 (Test administration and scoring): Remember these can be billed by technicians under supervision, freeing up the psychologist’s time for higher-reimbursing activities
Practical Tip: Create comprehensive assessment packages that appropriately utilize the full range of testing codes. Document all time spent on test selection, administration, scoring, interpretation, and report writing.
- 96130: 1 unit (first hour of psychological test evaluation)
- 96131: 2 units (additional 2 hours spent on integration of results and report writing)
- 96136: 1 unit (first 30 minutes of test administration by psychologist)
- 96137: 1 unit (additional 30 minutes of test administration by psychologist)
Financial Impact: A comprehensive assessment using appropriate code combinations can generate $350-700 in reimbursement, compared to $150-250 for a standard diagnostic interview.
4. Don’t Overlook Group Services
Group therapy and intervention services can significantly increase practice efficiency and revenue:
- 90853 (Group psychotherapy): Continues to be a cost-effective treatment modality, with 2025 bringing clearer documentation requirements on how individual attention is provided within the group context
- 90849 (Multiple-family group psychotherapy): Often overlooked but can be an effective intervention with its own distinct code
Practical Tip: Consider offering specialized groups that meet specific community needs. Document the individualized attention each participant receives, as this has become a focus of audits.
Financial Impact: A weekly group with 8 participants can generate $150-250 per hour, potentially doubling hourly revenue compared to individual sessions.
Documentation Best Practices for Audit-Proof Claims
Even the most strategic coding won’t help if documentation doesn’t support the services billed.
The following documentation strategies can help ensure your claims withstand scrutiny:
1. Embrace Medical Necessity
Every service must be clearly tied to medical necessity through proper diagnosis and treatment planning:
Best Practice: For each session, document:
- Specific symptoms or functional impairments being addressed
- How the intervention relates to the diagnosis
- Patient’s response to intervention
- Progress toward treatment goals
Patient continues to experience panic attacks (3 in past week, down from 5 previously reported) affecting ability to use public transportation. Today’s session focused on implementing exposure hierarchy techniques specifically targeting anticipatory anxiety about bus travel. Patient demonstrated increased understanding of panic cycle and successfully practiced diaphragmatic breathing when experiencing initial physiological arousal.
2. Maintain Time Documentation
For time-based codes, specific time notation is no longer just good practice—it’s essential:
Best Practice: Document:
- Exact start and end times for each service
- Total time spent
- How time was allocated (especially for assessment and testing services)
90834 Psychotherapy, 45 minutes
Session began: 10:15 AM
Session ended: 11:00 AM
Total time: 45 minutes
Time spent on cognitive restructuring techniques and homework review to address persistent negative thought patterns related to diagnosed Major Depressive Disorder.
3. Support Complex Services
For higher-reimbursing or add-on codes, additional documentation elements are needed:
Best Practice: For interactive complexity (90785), clearly document the specific factors that complicated the delivery of care.
Interactive complexity factors present:
- Session required involvement of parent to address behavioral interventions for 10-year-old patient with ADHD
- Child demonstrated high emotional reactivity with frequent interruptions and difficulty focusing, requiring adaptation of therapeutic techniques and materials
- Used play therapy techniques to facilitate communication due to patient’s developmental level
Technology Tools for Reimbursement Optimization
In 2025, leveraging technology has become essential for maximizing reimbursement potential:
1. AI-Enhanced Documentation Solutions
Several new platforms offer artificial intelligence capabilities that can help identify potential coding opportunities:
- Real-time suggestions for add-on codes based on documentation keywords
- Alerts for services approaching time thresholds that would qualify for higher-level codes
- Documentation completeness checks to ensure all elements required for specific codes are present
Practical Tip: While AI tools can enhance your coding practices, always review suggestions critically. These tools should support—not replace—your clinical judgment.
2. Automated Claim Scrubbers
Modern practice management systems now include sophisticated claim scrubbers that can:
- Identify modifier requirements for telehealth services
- Flag potential code combinations that may trigger denials
- Suggest alternative coding approaches when payer-specific rules might otherwise lead to rejections
Financial Impact: Reducing claim rejections by even 5% can improve cash flow and save dozens of hours in administrative time annually.
3. Telehealth Optimization Tools
With telehealth now a permanent fixture, specialized tools can help ensure compliance and maximize reimbursement:
- Platforms that automatically track session time and generate appropriate time documentation
- Integration with EHRs to populate place of service codes and modifiers correctly
- Built-in compliance features that document internet connection quality and verify patient location for state licensing requirements
Payer-Specific Strategies
Different payers have different rules, and knowing these variations can significantly impact reimbursement:
1. Medicare Nuances
Medicare continues to have distinct requirements that affect reimbursement:
- The 2025 Medicare Physician Fee Schedule included a 2.7% increase for most behavioral health services
- Medicare now reimburses Licensed Professional Counselors (LPCs) and Marriage and Family Therapists (MFTs), but at 85% of the physician fee schedule
- Incident-to billing rules have been clarified, with stricter supervision requirements but expanded eligible provider types
Practical Tip: For Medicare patients, consider the financial implications of who provides services. While expanding access through multiple provider types is beneficial, assigning higher-complexity cases to providers who receive 100% of the fee schedule (vs. 85%) can optimize practice revenue.
2. Commercial Insurance Variations
Each commercial payer has unique policies worth knowing:
- Some national insurers have implemented their own versions of collaborative care reimbursement that differ from the standard CPT codes
- Prior authorization requirements vary significantly, with some payers requiring reauthorization for specific code transitions (e.g., moving from 90791 to 90837)
- Medical necessity documentation thresholds differ between payers, with some requiring explicit functional impairment language
Practical Tip: Create a payer matrix for your top 5 insurance companies, outlining their specific requirements for your most commonly used codes. Update this quarterly as policies change.
3. Employee Assistance Program (EAP) Maximization
EAP sessions are often undervalued but can serve as an important revenue stream and referral source:
- 2025 has seen increased standardization of EAP billing practices
- New codes specifically for brief interventions now apply to many EAP services
- Conversion rates from EAP to regular insurance can be optimized with proper documentation
Practical Tip: Develop clear protocols for transitioning patients from EAP to insurance-based services, including template language for documenting medical necessity that satisfies both EAP requirements and subsequent insurance coverage.
Implementing Your Reimbursement Optimization Plan
Knowledge without implementation yields no benefit.
Here’s a structured approach to putting these strategies into practice:
1. Conduct a Billing Audit
Begin by assessing your current practices:
- Review 20 random claims from the past quarter
- Compare billed codes against documentation to identify under-coding or compliance risks
- Calculate the potential revenue difference if optimal coding had been used
Practical Tip: Create a spreadsheet tracking the audit findings, potential revenue impact, and specific action items for improvement.
2. Develop Provider Education
Make coding knowledge accessible to all clinicians in your practice:
- Create laminated quick-reference guides for common scenarios
- Implement monthly coding updates during team meetings
- Consider investing in specialized behavioral health coding training
Practical Tip: Use real examples from your practice (appropriately de-identified) to illustrate both successful coding and missed opportunities.
3. Establish Quality Control Processes
Build systems that catch coding opportunities before claims are submitted:
- Implement a peer review process for documentation of complex services
- Create standard templates that prompt for elements supporting higher-level codes when appropriate
- Schedule quarterly internal audits to ensure continued compliance and optimization
Summary: Building a Sustainable Practice Through Strategic Reimbursement
 Maximizing reimbursement is about sustainability, just as much as it’s about increasing revenue. When behavioral health providers are fairly compensated for their work, they can continue providing essential services to their communities without risking burnout or financial strain.
Maximizing reimbursement is about sustainability, just as much as it’s about increasing revenue. When behavioral health providers are fairly compensated for their work, they can continue providing essential services to their communities without risking burnout or financial strain.
The 2025 CPT code updates represent both challenges and opportunities. Strategically implementing the aforementioned approach ensures that your practice receives appropriate compensation for the valuable services you provide.
Optimization is an ongoing process. Set aside time quarterly to review your coding practices, stay informed about payer policy updates, and refine your approach as the reimbursement landscape continues to evolve.
Combining clinical excellence with coding expertise allows you to create the foundation for a thriving practice that can sustainably serve patients for years to come.
Disclaimer: This article is provided for informational purposes only and does not constitute legal, billing, or financial advice. CPT codes and reimbursement rates are subject to change, and providers should verify current information with their specific payers before implementing any coding strategies.

