Healthcare practices face numerous challenges in maintaining healthy revenue streams, but few issues can be as devastating to the bottom line as incomplete or improper credentialing. While it might seem like a purely administrative task, credentialing directly impacts a practice’s ability to receive reimbursement for services rendered. We’ll take a look at the multifaceted ways incomplete credentialing affects practice revenue and provides actionable strategies to prevent revenue loss.
Understanding the Credentialing Process
Before diving into the financial implications, it’s crucial to understand what credentialing entails. Credentialing is the systematic process of verifying a healthcare provider’s qualifications, including their education, training, licensure, and experience. This process isn’t just a one-time event – it’s an ongoing requirement that involves multiple stakeholders, including insurance companies, hospitals, and regulatory bodies.
The typical credentialing process includes:
- Primary source verification of medical education and training
- Confirmation of current state medical licenses
- Verification of board certifications
- Review of work history and clinical privileges
- Investigation of malpractice history
- Validation of DEA registration
- Confirmation of professional references
Each of these elements must be thoroughly documented and regularly updated to maintain active credentialing status. When any part of this process is incomplete or delayed, the financial consequences can be significant and far-reaching.
The Direct Financial Impact of Incomplete Credentialing
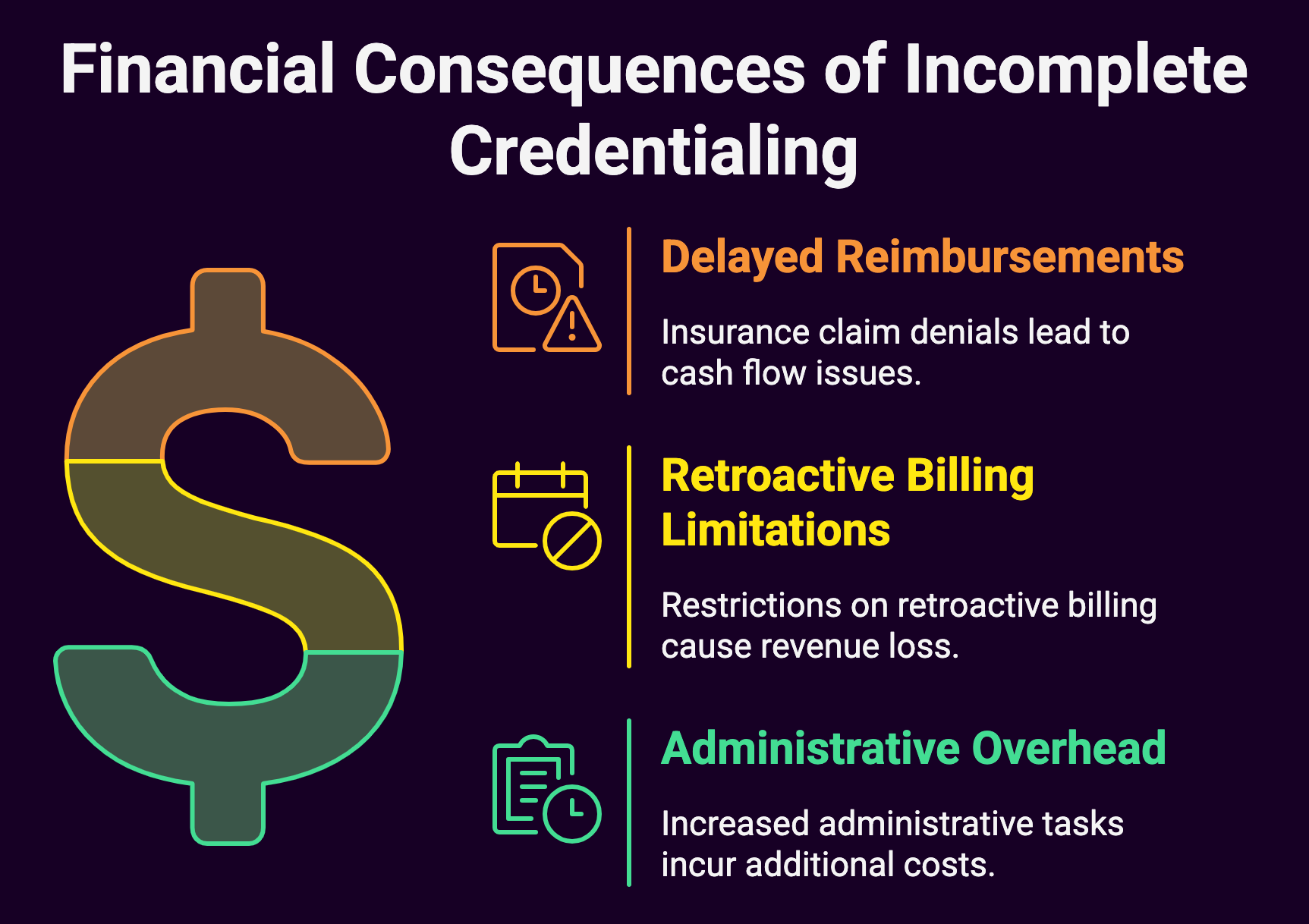
1. Delayed Reimbursements
Perhaps the most immediate and visible impact of incomplete credentialing is delayed reimbursement from insurance companies. When a provider isn’t properly credentialed with an insurance plan, claims submitted for their services are typically denied.
These denials create a domino effect of financial challenges:
- Cash flow disruption
- Increased accounts receivable
- Additional administrative work to resubmit claims
- Potential loss of revenue if the timely filing deadline passes
- Strain on working capital
For example, consider a primary care physician who sees 20 patients per day, with an average reimbursement of $100 per visit. If their credentialing lapses with just one major insurance carrier, they could lose $2,000 in revenue per day. Over a month, this amounts to approximately $40,000 in delayed or potentially lost revenue.
2. Retroactive Billing Limitations
Many practices operate under the misconception that they can simply bill retroactively once credentialing is complete. While some insurance companies do allow retroactive billing, others have strict limitations or don’t permit it at all.
This creates several problems:
- Permanent loss of revenue for services already provided
- Inability to collect from patients due to contractual obligations
- Potential compliance issues if attempting to bill patients directly
- Damaged relationships with patients who may be forced to pay out-of-pocket
3. Administrative Overhead
The cost of managing incomplete credentialing extends beyond lost reimbursements.
Administrative staff must dedicate significant time to:
- Tracking and following up on pending applications
- Responding to additional information requests
- Managing denied claims
- Communicating with insurance companies
- Updating patient records and billing systems
These activities represent both direct labor costs and opportunity costs, as staff members could be focusing on other revenue-generating activities instead.
Indirect Financial Consequences

1. Patient Satisfaction and Retention
Incomplete credentialing can significantly impact patient satisfaction and retention, which has long-term financial implications.
When patients discover their insurance won’t cover services due to credentialing issues, they may:
- Seek care elsewhere
- Leave negative reviews online
- Share their negative experiences with others
- Delay necessary follow-up care
The lifetime value of a patient can be substantial, especially in specialties with ongoing care needs. Losing patients due to credentialing issues can impact practice revenue for years to come.
2. Referral Network Disruption
Many practices rely heavily on referrals from other healthcare providers.
When credentialing issues arise, referring physicians may:
- Stop sending patients to avoid insurance complications
- Question the practice’s administrative competence
- Seek alternative referral partnerships
- Lose confidence in the practice’s ability to manage complex cases
Rebuilding damaged referral relationships takes time and effort, during which the practice continues to lose potential revenue.
3. Staff Morale and Productivity
Dealing with credentialing issues can take a toll on staff morale and productivity:
- Front desk staff must handle frustrated patients
- Billing staff face increased workload from denied claims
- Providers may feel pressure to see more patients to compensate for revenue loss
- Practice managers must divert attention from other important initiatives
Low morale and burnout can lead to increased staff turnover, adding recruitment and training costs to the practice’s financial burden.
The Ripple Effect on Practice Operations
1. Cash Flow Management
Incomplete credentialing can create serious cash flow challenges that affect various aspects of practice operations:
- Delayed vendor payments
- Difficulty meeting payroll obligations
- Postponed equipment purchases or upgrades
- Limited ability to invest in practice growth
- Increased reliance on credit lines or loans
These cash flow issues often result in additional expenses through:
- Late payment penalties
- Interest charges on loans or credit lines
- Missed early payment discounts from vendors
- Higher costs for emergency purchases or repairs
2. Growth and Expansion Limitations
When practices struggle with credentialing-related revenue issues, they often must postpone or abandon growth initiatives:
- Hiring new providers
- Opening additional locations
- Implementing new services
- Upgrading technology systems
- Marketing and outreach efforts
This opportunity cost can be substantial, especially in competitive markets where other practices continue to grow and evolve.
Preventive Strategies and Best Practices
1. Establishing a Robust Credentialing Program
To minimize revenue impact, practices should implement a comprehensive credentialing program that includes:
Dedicated Credentialing Staff
- Assign specific team members to manage credentialing
- Provide ongoing training and education
- Establish clear accountability measures
- Create backup coverage for key personnel
Technology Solutions
- Implement credentialing software
- Set up automated reminder systems
- Use tracking tools for application status
- Maintain digital document repositories
Standard Operating Procedures
- Document all credentialing processes
- Create checklists for common tasks
- Establish quality control measures
- Define escalation procedures
2. Proactive Monitoring and Maintenance
Successful practices maintain active oversight of their credentialing status:
Regular Audits
- Review provider enrollment status
- Check expiration dates for licenses and certifications
- Verify insurance panel participation
- Monitor claim denial patterns
Calendar Management
- Track renewal deadlines
- Schedule regular updates
- Plan for application processing time
- Coordinate with provider schedules
Communication Systems
- Regular updates to providers
- Structured reporting to practice leadership
- Clear channels for staff feedback
- Established protocols for patient communication
Financial Risk Management Strategies
1. Revenue Protection Measures
Practices can implement several strategies to protect revenue during credentialing challenges:
Financial Reserves
- Maintain adequate cash reserves
- Establish lines of credit
- Create emergency funding plans
- Budget for credentialing-related expenses
Alternative Revenue Streams
- Develop cash-pay services
- Implement time-of-service collections
- Explore ancillary service opportunities
- Consider membership or subscription models
Insurance Coverage
- Maintain appropriate liability coverage
- Consider business interruption insurance
- Review coverage for credentialing errors
- Evaluate cyber liability protection
2. Operational Efficiency Improvements
Practices can offset potential revenue losses through improved efficiency:
Workflow Optimization
- Streamline administrative processes
- Automate routine tasks
- Implement lean management principles
- Optimize scheduling systems
Resource Allocation
- Cross-train staff members
- Share resources between locations
- Optimize provider schedules
- Manage supply costs effectively
The Role of Technology in Credentialing Management
1. Software Solutions
Modern credentialing management software can significantly reduce revenue impact through:
Automation Features
- Application tracking
- Document management
- Expiration alerts
- Status reporting
Integration Capabilities
- Electronic health records
- Practice management systems
- Billing software
- Human resources systems
Analytics and Reporting
- Revenue impact analysis
- Processing time metrics
- Compliance monitoring
- Performance tracking
2. Digital Transformation Benefits
Implementing technology solutions can provide numerous advantages:
Increased Efficiency
- Reduced processing time
- Fewer manual errors
- Better resource utilization
- Improved data accuracy
Enhanced Compliance
- Automated updates
- Built-in verification
- Audit trail maintenance
- Standardized processes
Legal and Compliance Considerations
1. Regulatory Requirements
Practices must navigate complex regulatory requirements:
Federal Regulations
- Medicare enrollment requirements
- HIPAA compliance
- Federal fraud and abuse laws
- DEA registration requirements
State Requirements
- Licensing board regulations
- State-specific credentialing rules
- Insurance department requirements
- Facility licensing requirements
2. Risk Management
Proper risk management is essential for protecting practice revenue:
A. Documentation Requirements
- Maintain detailed records
- Track all communication
- Document decision-making processes
- Keep audit trails
B. Compliance Programs
- Develop written policies
- Provide staff training
- Conduct regular audits
- Establish reporting procedures
Future Trends and Considerations
1. Industry Changes
The credentialing landscape continues to evolve:
Digital Transformation
- Blockchain technology
- AI-powered verification
- Cloud-based solutions
- Mobile accessibility
Regulatory Evolution
- Standardization efforts
- Simplified processes
- Interstate compatibility
- Universal applications
2. Practice Adaptation
Successful practices must prepare for future changes:
Technology Investment
- Regular system updates
- Staff training programs
- Integration planning
- Security measures
Process Evolution
- Continuous improvement
- Best practice adoption
- Innovation integration
- Flexibility maintenance
Summary: Incomplete Credentialing Can Negatively Affect Revenue
Incomplete credentialing represents a significant threat to practice revenue, but its impact can be minimized through proper planning, robust systems, and proactive management. Medical practices must stay ahead of credentialing requirements to maintain healthy revenue streams and sustainable operations.
Success in credentialing management requires a comprehensive approach that includes:
- Strong leadership commitment
- Adequate resource allocation
- Effective use of technology
- Continuous process improvement
- Regular staff training
- Proactive risk management
It’s a good idea to understand the full scope of how incomplete credentialing affects practice revenue. Through the implementation of appropriate preventive measures, healthcare practices can protect their financial health and focus on their primary mission: providing quality patient care.
The investment in proper credentialing management, while potentially substantial, pales in comparison to the potential revenue loss and operational disruption that can result from incomplete or improper credentialing. Practices face increasing financial pressures and regulatory requirements. Therefore, maintaining effective credentialing processes becomes not just an administrative task, but a crucial component of financial success and organizational sustainability.

