Remember the days when healthcare provider enrollment meant drowning in a sea of paperwork? I’m talking about mountains of forms, countless phone calls, and weeks (or even months) of waiting for approvals. It’s fascinating to see how far we’ve come from those paper-heavy days to today’s streamlined digital provider enrollment processes. We’ll examine this remarkable transformation that has revolutionized how healthcare providers join insurance networks and medical groups.
The Paper Era: Where It All Began
Back in the day (and we’re talking not too long ago), provider enrollment was nothing short of a administrative nightmare. Picture this: a newly graduated physician wanting to join an insurance network would need to complete dozens of different applications, each requiring essentially the same information but in slightly different formats. Fun times, right?
Traditional Paper-Based Process
A typical enrollment packet would include countless pages requiring detailed information about: Here’s the kicker: providers had to fill out this information repeatedly for each insurance company, hospital, or healthcare organization they wanted to work with. It was like writing the same essay over and over again, just changing the header each time. The verification process wasn’t any better. Staff members had to manually verify each piece of information by calling schools, previous employers, and licensing boards. They’d then file these verifications in massive folders that would eventually take up entire rooms of storage space. If you needed to find something specific? Well, hope you packed a lunch because you’d be digging through files for hours. By the early 2000s, it became crystal clear that the paper-based system was no longer sustainable. Healthcare organizations were facing several critical challenges: The expenses associated with paper-based enrollment were astronomical. Think about it: paper, printing, postage, storage space, and the sheer number of staff hours required to process applications. One study estimated that the average cost of credentialing a single provider could range from $200 to $400, not including the organization’s overhead costs. The timeline for completing provider enrollment could stretch anywhere from 90 to 180 days. That’s half a year of potential revenue lost while waiting for paperwork to process! These delays weren’t just frustrating – they were costly for both healthcare organizations and providers. Human error in manual data entry was a constant issue. One missing digit in a license number or a transposed date could result in rejected applications and restart the entire process. Studies showed that paper-based credentialing had an error rate of up to 10%, meaning one in ten applications had some type of mistake. Keeping up with changing regulations and maintaining accurate records was becoming increasingly difficult. The risk of non-compliance with state and federal regulations was a constant concern, especially as healthcare regulations became more complex. The first wave of digital transformation in provider enrollment began in the late 1990s and early 2000s. Organizations started with basic digital solutions, like scanning paper documents and storing them electronically. While this was a step forward from physical storage, it was really just digitizing the paper problem rather than solving it. The Council for Affordable Quality Healthcare (CAQH) made a significant breakthrough in 2002 with the launch of ProView (formerly known as the Universal Provider Datasource). This platform allowed providers to submit their information once and share it with multiple organizations – a radical concept at the time! At Medwave, we’ve produced our own form which allows our clients to create or update a CAQH Pro-View account. Early digital solutions faced their own challenges: Early software was often clunky and not user-friendly. Many healthcare organizations lacked the IT infrastructure to support these new systems, and staff members needed extensive training to use them effectively. Change is hard, and many organizations and providers were hesitant to abandon familiar paper-based processes. There were concerns about data security, system reliability, and the learning curve associated with new technology. Different systems often couldn’t communicate with each other effectively, leading to data silos and the need for manual data entry despite having digital systems in place. Fast forward to today, and the provider enrollment landscape has undergone a complete metamorphosis. Modern digital credentialing and enrollment systems offer features that would have seemed like science fiction just a few decades ago: Modern systems can automatically verify credentials with primary sources, reducing the verification process from weeks to days or even hours. These systems maintain continuous monitoring of licenses, sanctions, and other critical credentials, alerting organizations to any changes in real-time. Cloud technology has revolutionized how provider data is stored and accessed. Organizations can now: AI has transformed many aspects of provider enrollment: Some organizations are now exploring blockchain for provider credentialing, offering benefits like: The shift to digital provider enrollment has delivered numerous tangible benefits: What once took months can now be completed in weeks or even days. Some organizations report reducing their enrollment timeline by up to 75% after implementing digital solutions. Digital processes have significantly reduced costs associated with provider enrollment: Digital systems have dramatically reduced error rates through: Modern digital enrollment systems have transformed the provider experience: Despite the tremendous progress, the digital transformation of provider enrollment isn’t without its challenges: With increasing cybersecurity threats, organizations must invest heavily in: Healthcare organizations often use multiple systems that need to work together seamlessly: While digital systems save money in the long run, the initial investment can be substantial: For organizations looking to optimize their digital provider enrollment processes, here are some key best practices: Create standardized workflows for different provider types and specialties while maintaining flexibility for unique situations. Establish clear policies for: Ensure all stakeholders are properly trained on: Continuously assess and optimize your digital enrollment system: Looking ahead, several emerging trends are likely to shape the future of provider enrollment: We’re likely to see even greater automation in: Future systems will offer: Organizations will leverage data analytics for: Future systems will focus on: The transformation of provider enrollment from paper to digital has been nothing short of revolutionary. What was once a time-consuming, error-prone process has evolved into a streamlined, efficient system that benefits all stakeholders in the healthcare ecosystem. As technology continues to advance, we can expect even more innovations that will further improve the provider enrollment process. Organizations who embrace this digital transformation while maintaining focus on security, compliance, and user experience will be best positioned to thrive in the evolving healthcare landscape. The key is to view digital transformation not as a one-time project but as an ongoing journey of continuous improvement and adaptation to changing needs and technologies.

The Breaking Point: Why Change Was Necessary
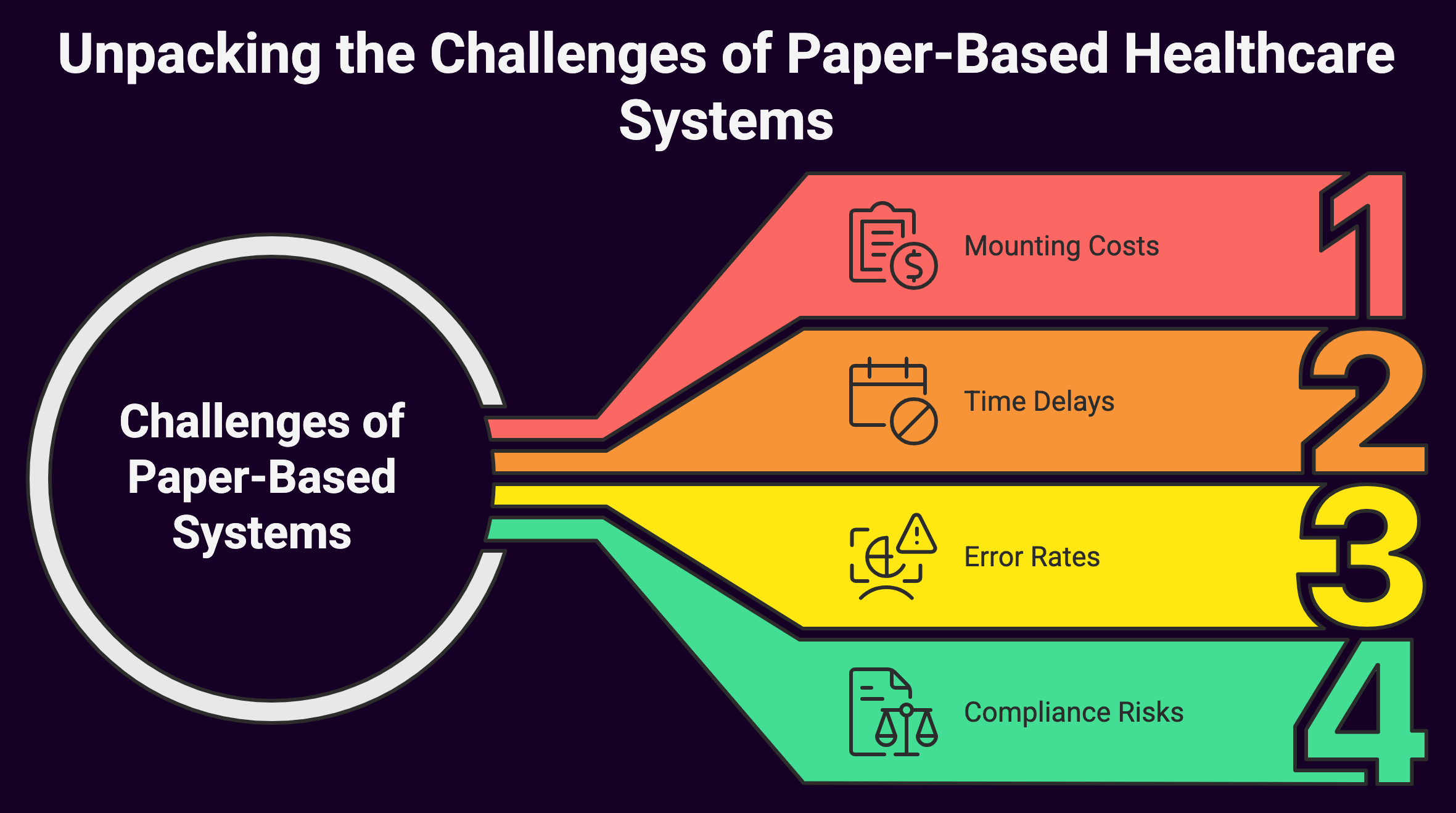
Mounting Costs
Time Delays
Error Rates
Compliance Risks
The Digital Dawn: Early Attempts at Modernization
Technology Limitations
Resistance to Change
Integration Issues
The Modern Era: True Digital Transformation
Automated Primary Source Verification
Cloud-Based Solutions
Artificial Intelligence and Machine Learning
Blockchain Technology
The Benefits of Digital Transformation
Faster Processing Times
Cost Reduction
Improved Accuracy
Enhanced Provider Experience
Challenges and Considerations in the Digital Age
Data Security and Privacy
Integration Complexity
Cost of Implementation
Best Practices for Modern Provider Enrollment
Standardize Processes
Implement Strong Data Governance
Provide Comprehensive Training
Regular System Evaluation
The Future of Provider Enrollment
Increased Automation
Enhanced Integration
Advanced Analytics
Improved User Experience
Summary: Paper to Digital Transformation Provider Enrollment