Telestroke and teleneurology refer to the use of telehealth to provide acute stroke care and neurological care from a distance. This allows neurologists and stroke specialists to evaluate and manage patients in hospitals or clinics that may not have specialty care available onsite.
The use of telehealth and virtual care models in neurology has grown enormously over the past decade. Remote delivery of urgent stroke treatment and ongoing management of chronic neurological conditions via telehealth platforms are transforming access to specialized care. However, coding and billing for telestroke, teleneurology, and other virtual neurology services can be complex.
Neurologists, hospital coders, billing staff or outsourced billers face a shifting landscape of telehealth codes, modifiers, documentation rules, licensing regulations, and reimbursement policies that must be mastered to sustain telehealth programs.
Telestroke networks enabling community hospitals to consult stroke experts at hub facilities have been shown to dramatically improve door-to-needle times for clot-busting tPA treatment in acute ischemic stroke. The ability for an offsite neurologist or stroke team to promptly evaluate imaging, assess the patient via an audio-video link, and recommend guideline-based therapies has saved lives and reduced long-term disability.
Meanwhile, teleneurology expands access to ongoing care for chronic neurologic illnesses for patients in remote regions without local specialists. Virtual visits allow neurologists to manage medications, order testing, assess symptoms, and provide patient education without requiring lengthy travels.
However, optimized coding is essential for these telehealth services to be financially viable over the long-term. Failure to select the proper CPT and diagnosis codes, apply required telemetry modifiers, follow telehealth rules, and thoroughly document the medical record can lead to claim denial and lost revenue. As telehealth expands access and versatility of neurology practice, understanding payer coding guidelines is critical. It’s important to understand that several CPT (Current Procedural Terminology) codes are commonly used for telestroke and teleneurology billing services.
This in-depth review aims to explain the intricacies of codes and documentation for telestroke, general teleneurology, virtual check-ins, e-consults, remote monitoring, and emerging tech-enabled care models.
Key Uses of Telestroke and Teleneurology
Some key uses of telestroke include:
- Performing urgent consultations and examinations of suspected stroke patients in community hospitals without on-site stroke experts. This facilitates faster treatment decisions.
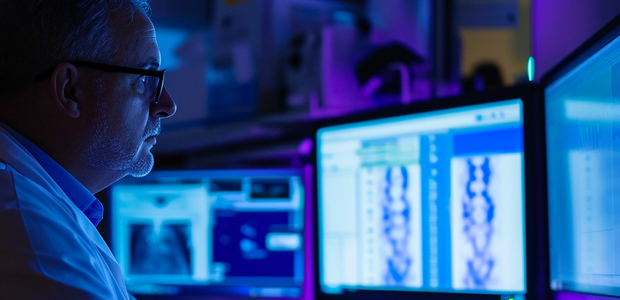
- Reviewing brain imaging studies and interpreting results remotely. CT and MRI scans can be viewed through teleradiology systems.
- Delivering timely recommendations for IV tPA thrombolysis when appropriate. This clot-busting medication must be given shortly after onset of ischemic stroke.
- Recommending other evidence-based treatments such as mechanical thrombectomy for large vessel occlusion strokes.
- Providing post-treatment management and follow up recommendations after acute treatment.
- Reducing time to treatment and door-to-needle times. Telestroke networks have been shown to significantly improve times for thrombolysis.
- Improving patient outcomes and reducing long-term disability rates from stroke.
Teleneurology similarly uses telehealth platforms to allow neurologists to diagnose, treat, and manage patients with various neurological conditions, remotely.
Some examples include:
- Conducting outpatient video visits with established patients for conditions like Parkinson’s disease, epilepsy, multiple sclerosis, and neuromuscular disorders.
- Performing urgent video consults for patients presenting to hospitals with neurological symptoms and concerns.
- Providing care for neurology patients located in rural areas without local specialists.
- Delivering follow up care and monitoring of neurological conditions via video visits.
- Adjusting medications and treatments for neurology patients through telehealth.
- Ordering additional testing like EEGs, EMGs, nerve conduction studies etc., which can be performed at another location.
- Reducing unnecessary transfers to higher levels of care when safe outpatient management is possible via teleneurology.
The use of telestroke and teleneurology services has grown exponentially with the expansion of telehealth technology, remote physician licensure, and favorable reimbursement policies. Coding and billing these services appropriately is key for sustainable teleneurology programs.
CPT Codes for Telestroke Evaluations and Consultations
The main CPT (Current Procedural Terminology) codes neurologists and telestroke providers report for remote evaluations of suspected stroke patients include:
Outpatient or Office E/M Codes
- 99201: Used for a straightforward interval history and exam via telehealth with straightforward medical decision making. Typical time 10 minutes.
- 99202: Report for an expanded problem focused history and exam with straightforward medical decision making. Typical time 20 minutes.
- 99203: Appropriate for a detailed history and exam with low level medical decision making complexity. Typical time 30 minutes.
- 99204: Billed for a comprehensive history and exam with moderate complexity medical decision making. Typical time 45 minutes.
- 99205: Reported for a comprehensive history and exam with high complexity decision making. Typical time 60 minutes.
- 99212-99215: Used for established patient telestroke evaluations proportionate to work required.
These E/M codes are selected based on the extent of data review, complexity of decision making, and time required for the telehealth encounter. A detailed history, review of systems, and neurological exam conducted via telestroke technology can meet key components for higher level E/M services.
Hospital Inpatient and Observation Codes
- 99218: Initial observation or inpatient hospital care via telehealth with straightforward decision making. Typical time 30 minutes.
- 99219: Initial observation or inpatient hospital care with detailed history, exam and/or medical decision making of moderate complexity. Typical time 50 minutes.
- 99220: Used for the most extensive inpatient telestroke consultation requiring comprehensive history, exam and high complexity decision making. Typical time 70 minutes.
- 99224-99226: Subsequent inpatient or observation telestroke care coded based on clinical work required and medical decision complexity.
Inpatient vs. outpatient status determines whether office or hospital admission codes are utilized. Level selection depends on clinical documentation and medical decision making complexity.
Telehealth Consultation Codes
- G0406: Follow-up inpatient telehealth consultation, typically 15 minutes communicating with the patient/family and reviewing data.
- G0407: Follow-up inpatient telehealth consultation, typically 25 minutes.
- G0408: Follow-up inpatient telehealth consult, typically 35 minutes or more.
- G0425: Initial inpatient telehealth consult, typically 30 minutes with the patient and reviewing records.
- G0426: Initial inpatient consultation via telehealth, typically 50 minutes.
- G0427: Initial inpatient telehealth consultation, typically 70 minutes or more of clinical discussion.
These G codes are an alternative to initial and follow up admission E/M services when the telehealth contact originates from the consulting office. The time thresholds help guide code selection.
Prolonged Visit Code
- 99354: Prolonged E/M or psychotherapy service beyond the typical time of the base code. Used in addition to office/outpatient visit code when telestroke evaluation exceeds the average time by 30 minutes.
- 99355: Report for each additional 30 minutes beyond the first hour of prolonged service time.
Neurology Exam Codes
- 96116: Neurobehavioral status exam by physician or psychologist via telehealth, typically taking 60 minutes.
- 96121: Neurobehavioral status exam via telehealth, typically taking 30 minutes.
These detail the neurological testing completed during a telestroke evaluation like mental status, cranial nerve, motor exam, etc,. 96116 is used for a full examination and 96121 for an interval, follow up or abbreviated exam.
Telehealth Modifiers
- 95: Synchronous telehealth service rendered via real-time interactive audio and video telecommunications system. Appended to most telestroke visit codes.
- GQ: Asynchronous (store and forward) telehealth service like reviewing prerecorded videos or images via a HIPAA-compliant platform.
- GT: Via interactive audio and video telecommunication systems for federal telehealth services. May be used together with modifier 95.
These telemetry modifiers identify the type of technology used to deliver the remote stroke care services. Appropriate modifiers must be included for payer reimbursement.
Common Telestroke Diagnoses and CPT Code Pairs
- I63.9 Cerebral infarction, unspecified: 99204-95 for left MCA stroke telehealth consult.
- I61.9 Hemorrhagic stroke, unspecified: 99223-95 for telehealth follow up of right ICH.
- G45.9 Transient cerebral ischemic attack, unspecified: 99202-95 for transient neuro deficits.
- R47.02 Dysarthria: 96121-GT to assess speech changes after anterior circulation stroke.
- Z86.73 Personal history of transient ischemic attack (TIA): 99212-95 for HPI and interval exam of post-TIA patient via video.
- R51 Headache: G0406-95 for short interval follow up on post-stroke headache via telehealth.
Proper code selection reflects the clinical details of the telestroke or TIA evaluation, management, counseling, and treatment recommendation provided. Accurate coding is crucial for fair reimbursement.
Billing and Coding Considerations for Telestroke Services
When coding and billing for telestroke services, some important considerations include:
- The level of telehealth service is determined by the same key factors as regular E/M visits – history detail, exam extent, and medical decision making complexity. Time is also a key factor.
- Thorough medical record documentation is required to justify the level of E/M, consultation, or prolonged services codes reported.
- Informed consent for telehealth should be obtained and documented prior to initiation of the visit.
- Licensure requirements must be met for providing interstate telestroke consults across state lines. Physicians should be licensed in the patient’s state.
- Established telehealth policies, network agreements, and emergency privileges should be in place at spoke/originating sites receiving telestroke consultation services.
- Proper modifiers 95 or GQ must be included on claims to identify services as telehealth. GT modifier can also be appended for federal telehealth sites.
- Telepresenters or nurses at the patient’s bedside can assist with elements like vitals and exam maneuvers under physician direction.
- HIPAA-compliant interactive audio-video systems must be utilized to ensure privacy and security.
- Medical reasons for telehealth use instead of in-person care should be documented such as after hours, rural setting, rapid specialist access etc.
By following coding guidelines and documentation requirements, neurologists can effectively report their remote telestroke care without undercoding or risking claim denials. As telehealth use expands, payers are increasingly providing fair reimbursement for properly coded telehealth services.
CPT Codes for Teleneurology Services
In addition to telestroke care, neurologists also leverage telehealth to provide outpatient and inpatient teleneurology consultations, visits, and management for a broad spectrum of neurological conditions.
Some of the main CPT codes used for teleneurology billing include:
Outpatient Consultation and Office Visit Codes
- 99241-99245: Used for new patient consultations and evaluations via telehealth. Code level is based on history, exam and decision complexity.
- 99212-99215: Reported for established neurology patients, with code choice dependent on clinical work required.
- 99358: Prolonged visit code for extended time spent beyond that of the companion office/outpatient code.
- 99441-99443: Used for virtual check-ins, remote assessments, and brief digital E/M services for established patients. Choice depends on time spent.
Hospital Care Services
- 99221-99223: Initial hospital inpatient or observation care for new or established patients via telehealth.
- 99231-99233: Subsequent hospital care for admitted patients involving telehealth.
- 99251-99255: Inpatient consultations for new or established hospitalized patients conducted via telehealth.
Telehealth Consultation Codes
- G0406-G0408: Follow up telehealth inpatient consults that originate from the consultant’s office.
- G0425-G0427: Initial inpatient telehealth consults that originate from the consulting physician’s office.
- G2010: Remote analysis of recorded video and/or image data like earlier EEG, EMG or skin images.
Care Management Services
- 99484: Complex chronic care management services provided remotely with clinical staff and patient under direction of physician.
- 99487-99489: Used for additional time spent in remote patient care management beyond the initial 20 minutes per month.
- 99490: Reports 20 minutes or more of remote chronic care management in a calendar month.
Neurobehavioral Exam Codes
- 96116: In-depth neurobehavioral status exam lasting roughly 60 minutes, conducted via telehealth.
- 96121: Abbreviated or follow up neurobehavioral status exam taking approximately 30 minutes.
Telehealth Modifiers
- 95 or GT: Used to label synchronous audiovisual services.
- GQ: Identifies store and forward asynchronous telehealth services.
Common neurology diagnoses addressed via telehealth often include seizures (G40, R56), migraines (G43, R51), dementia (F01, F03), MS (G35), Parkinson’s (G20), and various neuropathies (G60, G62). Accurate coding is key.
Billing and Coding Tips for Teleneurology Services
- Modifier 95 or GT is required to denote telehealth care modalities.
- Consent should be obtained from the patient to conduct care through telehealth technologies.
- Medical necessity for virtual care instead of in-office visits should be documented where applicable.
- The same level selection principles apply to telehealth visits as regular E/M services.
- Time-based coding can be utilized as an alternative to key component-based coding if more accurate.
- Virtual check-ins and e-visits may involve provider work outside of face-to-face time.
- Documentation should be complete in the medical record to corroborate all codes reported.
- Licensed independent practitioners can bill for telehealth services directly.
- Laws regarding telehealth care across state lines should be reviewed.
- Policies for telehealth privileges should be established at originating facility sites.
With these coding and billing principles in mind, neurologists can be reimbursed appropriately for medically necessary teleneurology services delivered via telehealth. As technology expands access to specialized neurology expertise through telehealth, following payer coding and documentation requirements is vital.
Innovations in Virtual Neurology Care
The telestroke and teleneurology landscape is constantly evolving with new technologies and video consultation platforms aimed at improving access and care delivery for complex neurological conditions.
Some innovations in virtual neurology care include:
- Increased adoption of patient portals, remote monitoring devices, and wearable technology that can sync data with the EHR during telehealth visits. This facilitates neurologic care from a distance.
- Use of digital symptom diaries, speech/movement analysis tools, and vision/cognitive testing apps that allow remote clinical assessment. Patients can complete or use these prior to a video visit.
- New specialized cameras and devices that can visualize eye movements, visual fields, pupil reactions etc during a live remote neuro exam.
- Advancements in telehealth bots, virtual assistants, and automated screening questionnaires which can collect patient data prior to a telehealth encounter.
- Stroke and seizure action plans empowering patients to record episodes and neurological events digitally to share through a patient portal or televisit.
- Natural language processing applied to telehealth visit transcripts to analyze speech and language, assess cognition, and detect subtle neurological deficits.
- Artificial intelligence to interpret and flag changes on remote patient-transmitted images, videos, and graphical tests like facial expressions, gaits, or gestures.
- Mixed reality technologies using augmented reality during telehealth consults to simulate and evaluate in-clinic assessments from afar.
- Remote presence robotic technology allowing the neurologist to virtually project into and navigate the patient’s room from their office using a mobile interface.
These technologies and innovative virtual platforms are expanding the possibilities of telestroke, teleneurology, and remote neurologic care. With specialty expertise limited, improved access through telehealth can provide timely, evidence-based care to underserved patient populations.
As video visit adoption accelerates across neurology, properly coding and documenting these services remains essential to sustainable telehealth programs. Telehealth presents new opportunities to enhance patient-centered, data-rich neurological care for the future.
Summary
To summarize, the main CPT codes used for telestroke and teleneurology billing include:
- E/M codes (99201-99215) for telehealth consultations
- Telehealth consultation codes (G0406-G0408, G0425-G0427)
- Brief communication code (G0373)
- Neuro exam codes (96116, 96121)
- Interactive complexity code (90785)
- Patient training code (93792)
Relevant modifiers include 95, GQ, and GT. Common ICD-10 diagnoses cover cerebrovascular conditions, transient ischemic attacks, headaches, movement disorders, and other neurological disorders. Proper coding is essential for reimbursement of remote neurology and stroke services conducted via telehealth.