Provider credentialing is a critical process in the healthcare industry that ensures patients receive care from qualified medical professionals. For healthcare providers seeking to join Kaiser Permanente’s network, understanding the credentialing process is essential to establishing a successful partnership with one of the nation’s largest integrated health systems.
Kaiser Permanente operates as both an insurance provider and a healthcare delivery system across eight states and the District of Columbia. With over 12 million members, it represents a significant opportunity for healthcare providers. However, joining Kaiser Permanente’s network involves a rigorous credentialing process that differs from traditional insurance-only networks.
The undermentioned content is a detailed overview of Kaiser Permanente’s credentialing process, the requirements providers must meet, and best practices for navigating the application successfully.
Kaiser Permanente’s Integrated Model
It’s important to understand Kaiser Permanente’s unique integrated model. Unlike traditional insurers that primarily contract with independent providers, Kaiser Permanente operates its own medical facilities and employs many of its healthcare professionals directly.
Kaiser Permanente consists of:
- Kaiser Foundation Health Plans (the insurance component)
- Kaiser Foundation Hospitals
- Permanente Medical Groups (physician-led organizations that provide care to Kaiser members)
This integrated model influences the credentialing process, as providers may be applying to join one of the Permanente Medical Groups as an employee or seeking to establish a contract as an external provider for specialized services.
Types of Provider Relationships with Kaiser Permanente
Kaiser Permanente offers several types of provider relationships:
- Employed Physicians and Providers: Practitioners who work directly for one of the Permanente Medical Groups.
- Contracted Providers: Independent practitioners or groups who provide services to Kaiser members through formal contracts.
- Affiliated Providers: Providers who have privileges at Kaiser facilities but are not directly employed.
- Community Providers: Independent practitioners who provide services to Kaiser members on a referral basis when services are not available within Kaiser’s network.
The credentialing process varies depending on the type of relationship you’re seeking with Kaiser Permanente.
The Kaiser Permanente Credentialing Process Overview
Kaiser Permanente maintains high standards for its provider network to ensure quality care for its members.
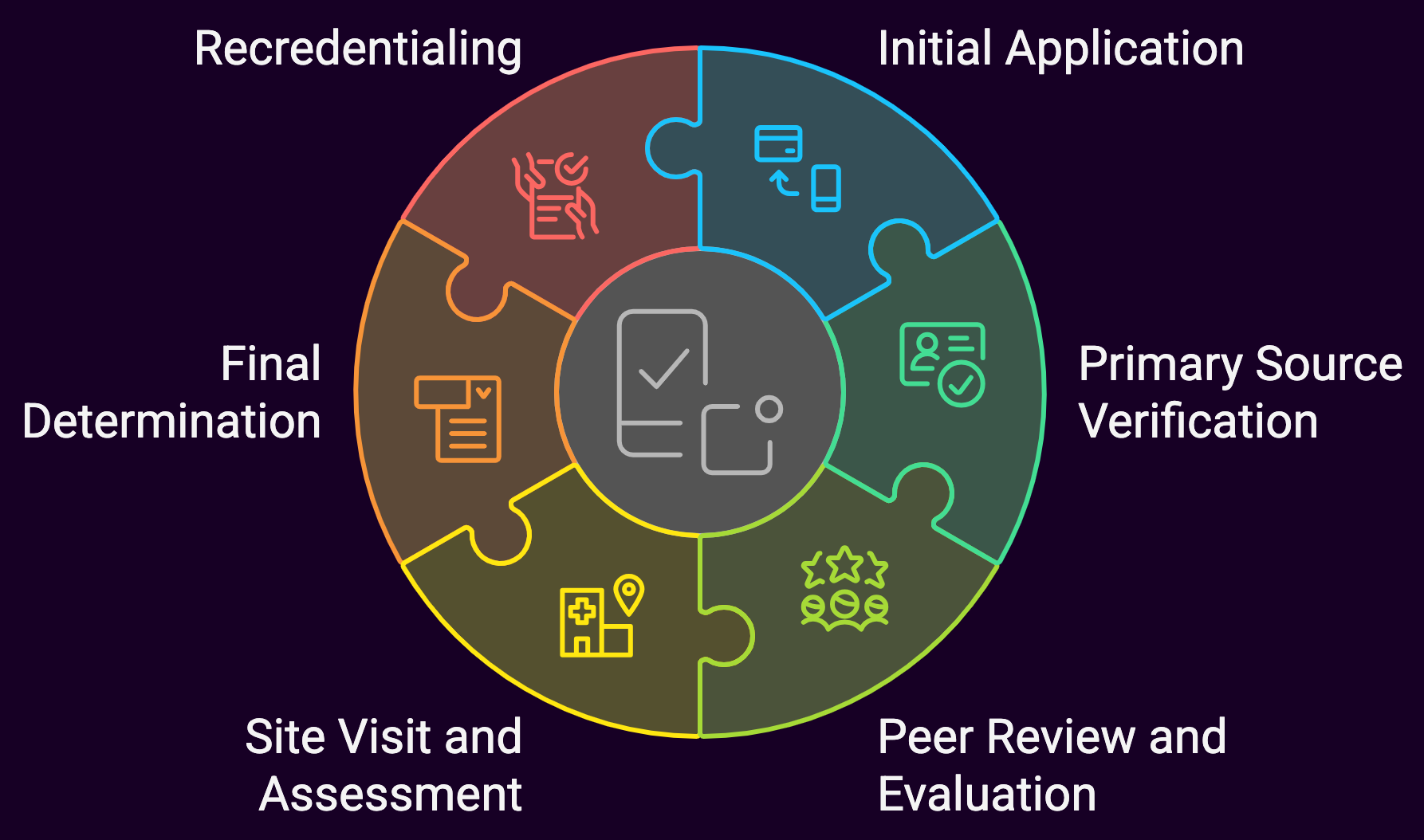
The credentialing process typically involves the following steps:
1. Initial Application
The credentialing process begins with an initial application. Providers must submit thorough information about their education, training, work history, and current practice. Unlike some other insurers, Kaiser Permanente’s application process may begin with an invitation to apply rather than an open application, particularly for employed positions.
2. Primary Source Verification
Kaiser Permanente conducts thorough primary source verification of all credentials, including:
- Medical education and training
- Board certifications
- State medical licenses
- DEA registration
- Work history
- Malpractice history
- National Practitioner Data Bank reports
- Office of Inspector General (OIG) exclusion list screening
3. Peer Review and Evaluation
Kaiser Permanente’s credentialing committee, composed of peer physicians, reviews the application and verification results. This committee evaluates the provider’s qualifications, practice patterns, and professional conduct.
4. Site Visit and Assessment
For certain provider types, particularly those who will be seeing patients in non-Kaiser facilities, a site visit may be conducted to assess the practice location, medical record keeping, accessibility, and adherence to safety standards.
5. Final Determination
Based on the exhaustive review, Kaiser Permanente’s credentialing committee makes a final determination on the provider’s application. This decision may include full approval, conditional approval, or denial.
6. Recredentialing
Kaiser Permanente requires recredentialing every three years. This process verifies that providers continue to meet the organization’s standards and have maintained their credentials.
Specific Requirements for Kaiser Permanente Credentialing
Education and Training Requirements
Kaiser Permanente requires providers to have:
- Graduation from an accredited medical school or appropriate professional school
- Completion of a residency program in the specialty in which the provider will practice
- Current board certification or active pursuit of board certification (typically within 5 years of completing training)
Licensure and Certification Requirements
Providers must maintain:
- Current, unrestricted state medical license in the state where they’ll practice
- Current, unrestricted DEA registration (if applicable)
- Current malpractice insurance meeting Kaiser Permanente’s minimum coverage requirements (typically $1 million per occurrence/$3 million aggregate, though this may vary by specialty and location)
- Appropriate board certification or eligibility
Professional Standards and Conduct Requirements
Kaiser Permanente evaluates providers based on:
- No history of license revocation or suspension
- No history of Medicare/Medicaid exclusion
- No felony convictions related to healthcare
- No pattern of excessive malpractice claims
- Demonstrated adherence to clinical practice guidelines and evidence-based medicine
- Commitment to Kaiser Permanente’s quality standards and patient-centered approach
Navigating Kaiser Permanente’s Regional Structure
Kaiser Permanente operates across multiple regions, each with its own Permanente Medical Group:
- Northern California (The Permanente Medical Group)
- Southern California (Southern California Permanente Medical Group)
- Northwest (Northwest Permanente)
- Hawaii (Hawaii Permanente Medical Group)
- Colorado (Colorado Permanente Medical Group)
- Mid-Atlantic States (Mid-Atlantic Permanente Medical Group)
- Washington (Washington Permanente Medical Group)
- Georgia (Southeast Permanente Medical Group)
Each region may have specific credentialing requirements in addition to the organization-wide standards. Providers should be aware of regional variations and direct their application to the appropriate regional entity.
The CAQH ProView Connection
Kaiser Permanente participates in the Council for Affordable Quality Healthcare (CAQH) ProView system, which streamlines the credentialing process. Providers can maintain their professional information in the CAQH database, which can then be accessed by Kaiser Permanente during the credentialing process. At Medwave, we make it easier on those we credential. We’ve designed a form to create or update a CAQH Pro-View account.
Steps for utilizing CAQH with Kaiser Permanente:
- Register with CAQH ProView if you haven’t already
- Ensure your CAQH profile is complete and up-to-date
- Authorize Kaiser Permanente to access your CAQH data
- Regularly update your CAQH information
Using CAQH can significantly reduce paperwork and expedite the credentialing process.
Kaiser Permanente’s Online Provider Portals
Kaiser Permanente offers online portals for providers to manage their relationship with the organization.
These portals vary by region but typically include:
- KP Provider Connect
- KP Link
- Regional provider portals for specific Permanente Medical Groups
These portals allow providers to:
- Check credentialing status
- Update practice information
- Access clinical resources
- Submit claims (for contracted providers)
- Communicate with Kaiser Permanente departments
Familiarity with these portals is essential for efficient practice management with Kaiser Permanente.
Timeframe for Kaiser Permanente Credentialing
The credentialing process with Kaiser Permanente typically takes 60-120 days from application to final decision.
However, this timeframe can vary based on:
- Completeness of the initial application
- Complexity of the provider’s history
- Responsiveness to requests for additional information
- Regional variations in processing times
- Employment versus contracting status
For employed positions, the credentialing process is often integrated with the hiring process, which may extend the timeline.
Best Practices for Successful Credentialing with Kaiser
Before Applying
- Research Kaiser Permanente’s Needs: Understand the specific needs of the Kaiser Permanente region where you’re applying. Some regions may have greater needs for certain specialties or in specific geographic areas.
- Understand the Integrated Model: Familiarize yourself with Kaiser Permanente’s integrated care model and how your practice would fit within it.
- Prepare Your Documentation:
- Gather all necessary documentation, including:
- Medical school diploma
- Residency/fellowship certificates
- Board certification
- State medical licenses
- DEA registration
- Current CV
- Malpractice insurance documentation
- Professional references
- Gather all necessary documentation, including:
- Update Your CAQH Profile: Ensure your CAQH ProView profile is complete and current.
During the Application Process
- Be Thorough and Accurate: Complete all application materials thoroughly and accurately. Inconsistencies or omissions can delay the process.
- Respond Promptly: Address any requests for additional information or clarification promptly.
- Follow Up Appropriately: Check on your application status periodically, but avoid excessive inquiries.
- Prepare for the Interview: If applying for an employed position, prepare for a formal interview process that evaluates both clinical skills and cultural fit with Kaiser Permanente’s team-based approach.
After Credentialing Approval
- Complete Orientation: Kaiser Permanente typically requires new providers to complete orientation to their systems and processes.
- Learn the EMR System: Kaiser Permanente uses Epic as its electronic medical record system. Familiarity with this system is crucial.
- Understand Kaiser Permanente’s Clinical Guidelines: Familiarize yourself with Kaiser Permanente’s clinical practice guidelines and quality metrics.
- Prepare for Ongoing Monitoring: Kaiser Permanente continuously monitors provider performance through various quality metrics and patient satisfaction scores.
Special Considerations for Different Provider Types
Primary Care Providers
Primary care providers often have additional requirements, including:
- Demonstrated experience in preventive care
- Comfort with team-based care models
- Ability to coordinate care across specialties
- Familiarity with population health management
Specialists
Specialists should be prepared to:
- Work collaboratively with Kaiser Permanente primary care providers
- Follow Kaiser Permanente’s referral processes
- Adhere to Kaiser Permanente’s practice guidelines for their specialty
- Participate in quality improvement initiatives
Allied Health Professionals
Non-physician providers such as nurse practitioners, physician assistants, and therapists have specific credentialing requirements that may include:
- Appropriate supervision agreements
- Collaborative practice agreements
- Scope of practice documentation
- Additional state-specific requirements
Handling Credentialing Challenges
If you encounter challenges during the Kaiser Permanente credentialing process, consider these strategies:
- Address Gaps or Issues Proactively: If you have gaps in your work history, malpractice claims, or other potential red flags, address them proactively in your application with appropriate context and explanation.
- Provide Additional Documentation: Be prepared to provide additional documentation or references to support your application if requested.
- Request Reconsideration: If your application is denied, you may have the opportunity to request reconsideration. Provide any new information that might influence the decision.
- Seek Feedback: If unsuccessful, request specific feedback on areas where you could strengthen your application for future consideration.
Summary: Getting Credentialed with Kaiser Permanante
Credentialing with Kaiser Permanente represents a significant opportunity to join one of the nation’s most respected integrated healthcare systems. The process is rigorous, but navigable with proper preparation and attention to detail. The credentialing process is an important quality assurance measure that protects patients and ensures the delivery of high-quality healthcare. Approaching the process with patience, thoroughness, and professionalism will increase your chances of success and help establish a strong foundation for your relationship with Kaiser Permanente.

