
Payer contracting stands as a critical challenge for healthcare providers of all sizes. Recognizing the intricacies and high stakes of this process, Medwave has emerged as a leading solution provider in this space. With our complete suite of payer contracting services, we offer healthcare organizations expert guidance and support to handle insurance negotiations and contract management.
We’ll take a look at the essentials of payer contracting and highlights how our specialized services are helping healthcare providers secure more favorable terms, optimize their revenue cycles, and ultimately focus more on what matters most, delivering high-quality patient care.
What is Payer Contracting?
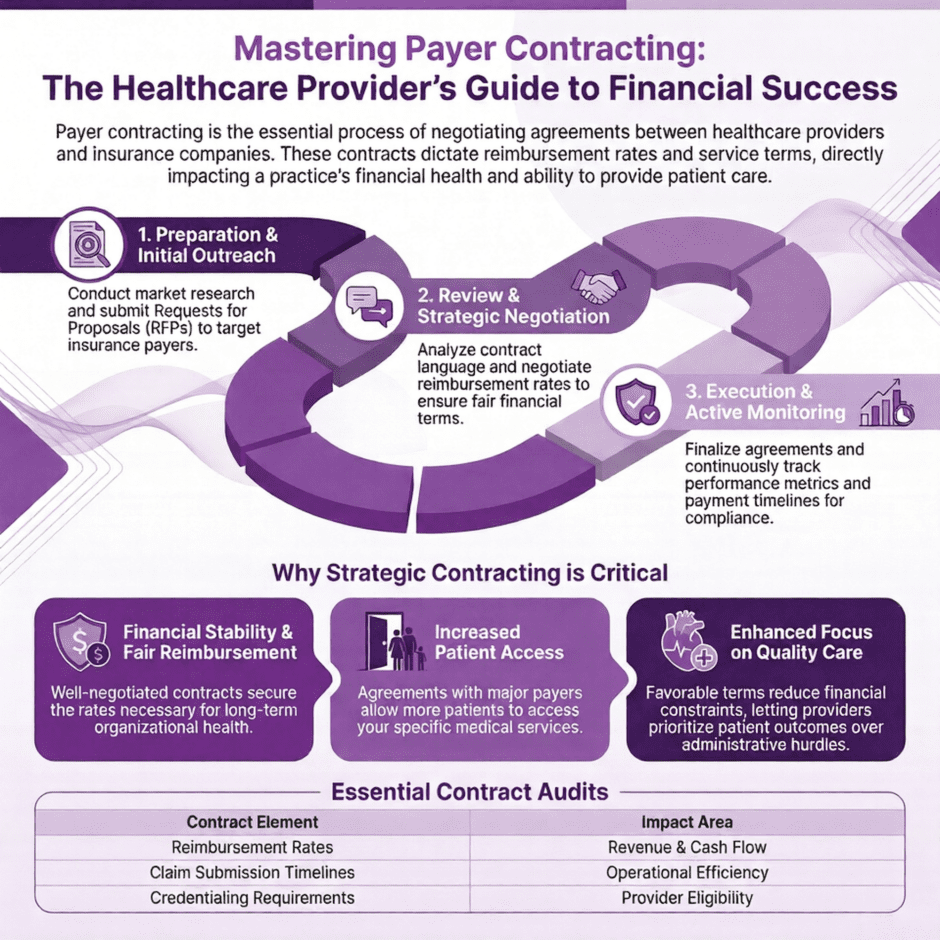
Payer contracting refers to the process of negotiating and establishing agreements between healthcare providers and insurance companies or other payers. These contracts define the terms under which providers will deliver services to the payer’s members and how the payer will reimburse the provider for those services.
The Importance of Effective Payer Contracting
Effective payer contracting is essential for several reasons:
- Financial stability: Well-negotiated payer contracts ensure fair reimbursement rates, contributing to the financial health of healthcare organizations.
- Patient access: Contracts with major payers increase the number of patients who can access a provider’s services.
- Quality of care: Favorable contract terms can support providers in delivering high-quality care without financial constraints.
- Competitive advantage: Strong payer relationships can differentiate a provider in a competitive market.
Key Components of Payer Contracts
Payer contracts typically include the following elements:
- Reimbursement rates and methodologies
- Covered services and exclusions
- Term and termination provisions
- Claims submission and payment timelines
- Credentialing requirements
- Performance metrics and quality measures
- Dispute resolution procedures
The Payer Contracting Process
The payer contracting process typically involves several steps:
- Preparation and research
- Initial outreach and request for proposal (RFP)
- Contract review and analysis
- Negotiation
- Contract finalization and execution
- Implementation and monitoring
Strategies for Successful Payer Contracting
To achieve favorable outcomes in payer contracting, consider the following strategies:
- Know your market position and value proposition
- Analyze historical claims data and financial performance
- Benchmark reimbursement rates against industry standards
- Develop a clear negotiation strategy and priorities
- Build strong relationships with payer representatives
- Leverage technology for contract management and analysis
- Consider engaging professional negotiators or consultants
Common Challenges
Healthcare providers often face various challenges during the payer contracting process:
- Negotiating fair reimbursement rates
- Deciphering complex contract language and terms
- Keeping up with changing healthcare regulations
- Managing multiple contracts with different payers
- Addressing disparities in negotiating power
- Adapting to value-based care models
The Future of Payer Contracting
As the healthcare landscape continues to evolve, payer contracting is likely to see significant changes:
- Increased adoption of risk-sharing arrangements
- Greater emphasis on data sharing and interoperability
- Integration of artificial intelligence in contract analysis and negotiation
- Expansion of value-based purchasing programs
- Growing focus on patient engagement and satisfaction metrics
Summary: Payer Contracting is Crucial

Payer contracting is a complicated, yet essential process for healthcare providers. Knowing all about the intricacies of contracting, adopting effective strategies, and staying informed about industry trends enables providers to negotiate favorable terms that support their financial stability and enable them to deliver high-quality patient care.
Mastering the art of payer contracting will remain a critical skill for successful healthcare organizations.
Payer contracting is an ongoing process that requires continuous attention, adaptation, and refinement. Investing time and resources into developing strong payer relationships and negotiation skills, allows healthcare providers to position themselves for long-term success in an ever-changing healthcare landscape. Regular review and optimization of payer contracts can lead to improved financial performance, enhanced patient care, and a stronger competitive position in the healthcare market.
Medwave, as Your Payer Contracting Experts
 Medwave, a leading healthcare consulting firm, offers payer contracting services to healthcare providers, helping them manage insurance negotiations and contract management. With our team of experienced healthcare professionals, we provide end-to-end support throughout the entire contracting process.
Medwave, a leading healthcare consulting firm, offers payer contracting services to healthcare providers, helping them manage insurance negotiations and contract management. With our team of experienced healthcare professionals, we provide end-to-end support throughout the entire contracting process.
Our services include market analysis to determine competitive reimbursement rates, contract review and optimization to ensure favorable terms, and skilled negotiation with payers to secure the best possible agreements.
Through partnering with Medwave, healthcare providers can benefit from expert guidance, streamlined processes, and improved financial outcomes in their payer contracting efforts, allowing them to focus more on delivering high-quality patient care while optimizing their revenue cycle management.
